We herein report a case of Behçet's disease (BD), which was stable until the Great East Japan Earthquake, but deteriorated thereafter and presented with Sweet's syndrome-like facial erythemas, along with exacerbation of other mucocutaneous conditions.
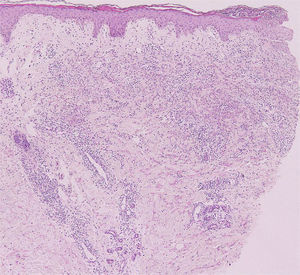
A 36-year-old male visited our hospital, complaining of fever, genital ulcer, folliculitis-like lesions, and erythema nodosum (Fig. 1a), and had been diagnosed previously with incomplete type BD six years ago. He received treatment with minocycline, colchicine, and his symptoms were under control. However, his symptoms recurred along with a fever of up to 39°C and throat pain following the Great East Japan Earthquake in March 2011 when he was evacuated from home and placed at a shelter. Physical examination revealed multiple oral ulcers, folliculitis on the back, tender subcutaneous erythematous nodules on the knee, and tender infiltrative erythematous plaques with surface scales on the cheek, forehead, and neck (Fig. 1b and c). A biopsy specimen taken from his face showed dense neutrophil infiltration throughout the dermis (Fig. 2). Laboratory examination showed elevated levels of white blood cell counts (12,200/μl with 80% neutrophils), C-reactive protein (11.44mg/dl), and erythrocyte sedimentation ratio (41mm/h). Antistreptolysin O (ASO) level was within normal ranges. HLA typing was negative for HLA-B51, but positive for HLA-A2, A24, B54, and B62. He was successfully treated with oral prednisolone (20mg/day).
The present case developed infiltrative erythemas on the face mimicking Sweet's syndrome, along with other cutaneous symptoms such as folliculitis and erythema nodosum. A biopsy specimen from the face revealed dense neutrophil infiltration throughout the dermis. Patients with BD rarely present with Sweet's syndrome-like infiltrative erythema.1 On the other hand, several cases have been reported as a co-existence of BD and Sweet’ syndrome; symptoms of Sweet's syndrome appear representing a flare or in the acute phase of BD.2 BD and Sweet's syndrome share common pathogenesis such as neutrophil activation, and Th1 type cytokines contribute to the pathogenesis of both disorders. We prefer to interpret our case as Sweet's syndrome-like eruptions that developed along with other symptoms such as oral ulcers, folliculitis, and erythema nodosum-like lesions in the exacerbation of BD, rather than the co-existence of Sweet's syndrome with BD, although the criteria of Sweet's syndrome are fulfilled. There were no other apparent triggers such as upper airway or gastrointestinal infections and the use of new drugs for the induction of Sweet's syndrome-like eruptions. Although the frequency is low, BD may be one of the underlying diseases susceptible for developing Sweet's syndrome-like eruptions. We have followed-up the patient for almost 10 years, and although he has had the occasional worsening of BD, the Sweet's syndrome-like eruption occurred only once. Our patient has HLA-B54, which may be an important genetic background in the development of Sweet's syndrome-like eruption.
Psychosocial stress has been reported to be a triggering and worsening factor of BD, and patients frequently develop a neurobehavioural syndrome, defined as ‘neuro-psycho-BD’. Our patient's symptoms were possibly exacerbated by mental stress caused by the Great East Japan Earthquake. Mental health problems have affected many residents of evacuation zones in Fukushima,3 although there are no studies of the deterioration of BD examining a number of patients. Anxiety and depression are common psychiatric disorders in patients with BD and more numerous than in controls,4 and psychological stressors influence the onset and flare of BD and/or recurrent aphthoid stomatitis. Approximately 70% of patients with BD recognized a stress factor prior to the onset of the disease, and 80% of patients with BD declared stress in the relapse period.5The hypothalamic-pituitary-adrenal axis affects the immune system, and thus in the present case the stress-induced immune alterations may have worsened the symptoms of BD.
Conflicts of interestNone declared.
Funding sourcesNone.