Attention has been focused on new ways to understand and manage urticaria ever since the recent addition of novel drugs to the therapeutic arsenal, the updating of clinical practice guidelines, and the publication of pathophysiologic insights. The Andalusian Section of the Spanish Academy of Dermatology and Venereology (AEDV) has developed a clinical pathway that defines quality-of-care characteristics and makes recommendations on decision-making affecting patients with urticaria. We present a patient-centered approach to care, in which the patient's clinical pathway through the health care system includes links between primary and hospital care to ensure continuity—a key feature of quality.
La incorporación de nuevos fármacos al arsenal terapéutico, la actualización de las guías de práctica clínica y los hallazgos fisiopatológicos recientemente comunicados hacen que el manejo y conocimiento de la urticaria sea un tema de candente actualidad. La Sección territorial andaluza de la AEDV ha desarrollado un proceso de atención en el que se describen el recorrido del paciente, las características de calidad de las actuaciones y las recomendaciones para la toma de decisiones en los pacientes con urticaria. Presentamos un enfoque centrado en el paciente, y en el que se muestra su devenir en el sistema sanitario y la interrelación entre la atención primaria y hospitalaria, garantizando un punto clave, su continuidad asistencial.
Interest in urticarial skin disease has risen in the last 10 years. A simple search of the US National Library of Medicine databases reveals that the number of publications indexed under the keyword urticaria in just the last year easily exceeds 600. The reasons behind the growing interest were well summarized in a recent opinion article in this journal, in which authors Gimenez-Arnau et al.1 remarked on the following developments:
- •
the recent publication of European clinical practice guidelines,
- •
our improved understanding of the pathogenesis of the disease,
- •
the emergence of patient associations and the participation of a variety of professionals in World Urticaria Day, and most importantly,
- •
the development of new biologic therapies available to treat the condition.
A disease with a prevalence of nearly 1% in the United States2 and similar rates in other Western countries like Spain,3 naturally draws attention. Chronic urticaria affects middle-aged populations and has a resulting economic impact on employed persons as well as the use of hospital resources. The patient with urticaria is a high user of health care services through visits to the emergency department, primary care clinics, and specialists—mainly dermatologists, allergy specialists, or internists.
The clinical practice guidelines updated in 20094 and revised again in 20145 were based on a systematic review of the literature applying the GRADE scale (Grading of Recommendations Assessment, Development and Evaluation). The members of 21 Spanish and international associations involved in the management of urticaria participated in the effort, which established an easy-to-use treatment algorithm incorporating indications that are implicitly or explicitly in accordance with each drug's summary of product characteristics. (An example is cyclosporin, whose use in the treatment of urticaria refractory to conventional treatment with antihistamines is regulated in Andalusia by resolution SA352/2012 of November 15, 2012.) However, the guidelines have not yet been analyzed and filled out with revisions specific to each participating country.6
While our main objective in managing the diagnosis and treatment of urticaria is to achieve rapid and complete control over signs and symptoms by prescribing appropriate medications according to the best available evidence of safety and efficacy, meeting that goal requires individualized case management. However, tailored care is not incompatible with planning the pathway our patients should follow in the health care system so that duplicated effort and unnecessary interventions are avoided.
Here is where systematizing care through process planning becomes essential. A clinical pathway, or care plan, specifies the who, when, where and how that govern the delivery of care for a condition or a set of related ones.
Our aim in this paper is to present the consensus reached by dermatologists of the national health service (NHS) of Andalusia regarding the care process for patients with urticaria. We describe the clinical pathway, the necessary steps and interventions, and the characteristics of quality of care for each act.
Defining the Clinical Pathway RequiredThe need to define and develop a framework for providing quality care efficiently in the Andalusian NHS led the working group to map the care processes that have been in place since 2000. This strategy has a single fundamental aim: to guarantee the quality of NHS services.7
The care process plan encompasses an overview of the actual path a patient will follow through the system. Work flows have been reordered and interventions that are of no use have been eliminated.
Elements intrinsic to the plan are
- •
interventions designed to be patient-, or user-, centered,
- •
the active involvement of health care professionals organized into multidisciplinary working groups,
- •
clinical practice that is appropriate according to guidelines and care plans,
- •
integrated recording of information, and finally,
- •
continuity of care to ensure cooperation between the various levels of the health care system.
The only care process plan currently in use in clinical management units (CMUs) in dermatology in the autonomous community of Andalusia is the one for the integrated care of skin cancer.8 Therefore, the Andalusian Regional Section of the Spanish Academy of Dermatology and Venereology (AEDV) took the portfolio of medical and surgical services in dermatology and the treatment of sexually transmitted infections of 20149 as its starting point and developed pathways for prioritized conditions and those for which no documentary support was currently in place. The conditions chosen were atopic dermatitis, sexually transmitted infections, benign cysts or tumors, and urticaria.
The Clinical Pathway and Characteristics Relevant to Quality of Care and Decision-MakingThe patient interacts with both primary care physicians and specialists after referral along the clinical pathway described in Tables 1 and 2, which define the who, what, where, when, and how of steps in the sequential phases of a process that guarantees continuity of care. (See Appendix A for the drafting process.)
Quality-of-Care Characteristics to Apply When Attending Persons With a Clinical Picture Compatible With a Diagnosis of Urticaria in Primary Care Centers and Emergency Departments.
| Care in the primary care center or emergency service Family practitioner, primary care nurse, primary care pediatrician |
| 1. Medical history |
| 1.1 Unequivocally identify the patient according to established procedures (a CSP). 1.2 Take the patient's medical history, including the following information: 1.2.1 The patient and family's past histories of urticaria, angioedema, and atopic dermatitis 1.2.2 The patient's history of other diseases (infections, inflammatory processes, allergies, digestive problems, psychosomatic diseases, stress, surgical implants), prior and current therapies (nonsteroidal anti-inflammatory drugs, hormone treatments, laxatives, immunizations, alternative medicine, etc.) 1.2.3 Factors or triggers associated with urticarial flare-ups: food, medications, physical stimuli, other 1.2.4 Prior treatments for urticaria 1.2.5 Symptoms, including the following: Pruritus (intensity and clinical course); pain and burning sensations Wheals: shape, size, location/distribution Angioedema: clinical course, frequency and duration of lesions, variations during the day; patterns on weekends, vacations or trips; joint pain; affective disorders, etc. Systemic signs and symptoms: respiratory and digestive symptoms, headache, hypotension, fever, joint pain. 1.2.6 History of dependence/addiction (to alcohol, smoking, other); occupational history (profession, pastimes) |
| 2. Physical examination |
| 2.1 Wash hands properly before and after the examination (a CSP). Examine the patient to identify manifestations of urticarial disease (wheals, angioedema). The characteristic signs are wheals, papuloerythematous lesions, or pale lesions with white halos tending to coalesce. The lesions appear suddenly (withinminutes), are fleeting, and usually resolving in <24hours. Angioedema is marked by the swelling of mucosal tissues (especially the lips and eyelids but also the larynx) or other soft tissues; the swelling resolves more slowly than urticarial lesions and can last 48hours. Often there are no signs on the skin surface or itching, but the condition might be painful. |
| 3. Documentation and provision of information |
| 3.1 Record data from the medical history and examination in the patient's chart; also note the clinical diagnosis and plan of action (an information-oriented CSP). 3.2 If urticaria is suspected, explain this clearly and precisely to the patient and family; record the clinical judgment in the patient's chart (an information-oriented CSP). 3.3. The referral to a specialist should be arranged during the same visit. A system for priority referrals to the specialist must be established based on signs and symptoms for optimal efficiency and use of health care resources. 3.4 According to expert opinion, referral to a specialist is necessary in the following situations: 3.4.1 When there is diagnostic uncertainty and a firm diagnosis is required (see Table 2, point 7.2, on differential diagnosis) 3.4.2 In chronic urticaria (lasting >6 wk), to confirm physical, food, or medication triggers 3.4.3 Acute urticaria (lasting <6 wk) that is refractory to first- and second-line therapies 3.4.4 Chronic urticaria (lasting >6 wk) that does not respond to second-line therapies (second-generation H1 antihistamines at a dose 4-fold higher than usually prescribed) 3.4.5 In chronic urticaria (lasting >6 wk), for additional tests If referral is indicated, write a full report for the dermatology CMU to ensure the transfer of information between professionals in different care settings as well as to ensure continuity of care (a CSP). |
| 4. Treatment |
| 4.1 When cases do not qualify for referral to the dermatology CMU, initiate general measures to manage the rash with first- or second-line treatments (i.e., second-generation H1antihistamines at the usual or 4-fold higher doses). |
Abbreviations: CMU, clinical management unit; CSP, critical safety point affecting patients as listed by the health service of the government of Andalusia (the Junta).
Quality-of-Care Characteristics to Apply When Attending Persons With Urticaria in Dermatology CMUs.
| Care in a dermatology CMU Professionals: Dermatologists, dermatology CMU nurses |
| 5. Medical history |
| 5.1 Unequivocally identify the patient according to established procedures (a CSP). 5.2 Update the patient's medical history as described in point 1.2 (Table 1), and expand it with the following information: 5.2.1 Evaluate the severity of the urticaria (scored on the UAS7 scale). 5.2.2 Evaluate the impact of urticaria on the patient's quality of life using an appropriate scale (e.g., the CU-Q2OL, AE-QOL, or DQLI). |
| 6. Physical examination and additional tests |
| 6.1 Wash hands adequately before and after the examination (a CSP). 6.2 Update the physical examination described in point 2.2. 6.3 Perform a dermatologic examination to describe the lesions, note their distribution and patterns formed (wheals, angioedema, anatomical location, etc.). 6.4 Evaluate patients with chronic urticaria as appropriate based on suspected triggers, using the following examinations and tests: pressure test (for pressure urticaria), ice-cube test (for cold urticaria), vortex provocation test (for vibratory urticaria), UV provocation test (for solar urticaria), stroking (for symptomatic dermatographism), wet gauze contact (for aquagenic urticaria), exercise (for cholinergic urticaria), and skin patch tests (for contact urticaria). 6.5 The urticaria diagnosis: this is a clinical diagnosis based on medical history and/or physical examination of a pruriginous rash of wheals and/or angioedema that is fleeting (<24hours). 6.6 A skin biopsy may be ordered if the clinical diagnosis is uncertain. Inform the patient or caregiver of the reasons for taking the biopsy, its objectives, and possible complications (an information-oriented CSP). Written informed consent is required before a biopsy can be performed (an information-oriented CSP). 6.7 There are no laboratory or other types of tests that can differentiate or confirm a diagnosis of urticaria. Complementary testing is not recommended in acute urticaria (strong recommendation based on clinician consensus). The following routine test complement is recommended for all patients with chronic urticaria: complete blood count, eosinophil sedimentation rate, C-reactive protein level. Depending on the patient's medical history, the following tests might be ordered: total serum immunoglobulin (Ig) E concentration, microbiologic processing, (e.g., for Helicobacter pylori detection), thyroid hormone level, antithyroid antibody assay, antinuclear antibody assay, and autologous serum skin test (for autoimmune urticaria). The search for trigger factors in chronic urticaria should be guided by information in the patient's medical history (strong recommendation, clinician consensus). |
| 7. Classification and differential diagnosis |
| 7.1 Current recommendations say that urticaria should be classified according to the 2013 EAACI/GA2LEN/EDF/WAO guidelines, which define the following types and subtypes: Types of urticaria: 7.1.1 Acute urticaria: appearance of spontaneous wheals, angioedema or both for <6 wk 7.1.2 Chronic urticaria: appearance of urticaria flare-ups (wheals, angioedema or both) for >6 wk Subtypes of chronic urticaria: 7.1.3 Chronic spontaneous urticaria: spontaneous appearance of wheals, angioedema or both lasting ≥6 wk and due to known or unknown causes 7.1.4 Inducible urticaria: symptomatic dermographism, cold urticaria, delayed pressure urticaria, solar urticaria, heat urticaria, vibratory angioedema, cholinergic urticaria, contact urticaria, aquagenic urticaria 7.2 Rule out the following diagnoses for each urticaria type: 7.2.1 Acute urticaria: drug eruptions (IgE mediated, idiosyncratic, cell mediated), food reactions (IgE mediated or not), intravenous infusion reactions (to contrast agents, immunoglobulins), infections (childhood viral diseases, mononucleosis, prodromal period of hepatitis B viral infection), polymorphous erythema, allergic contact dermatitis. 7.2.2 Chronic urticaria: urticarial vasculitis, familial fever syndromes with urticaria-like eruptions, Schnitzler syndrome, mastocytosis, Wells syndrome, polymorphous erythema |
| 8. Documentation and provision of information |
| 8.1 Record data from the medical history and examination as well as the clinical diagnosis and action plan (an information-oriented CSP). 8.2 If lesions are present at the time of the visit, clinical and dermoscopic images are recommended. The patient's written informed consent must be given before photographs are taken (an information-oriented CSP). 8.3 Patients with urticaria should take photographs of lesions during flare-ups to help with diagnosis and follow-up. 8.4 If food or medication triggers are suspected, refer the patient to the CMU for allergies. |
| 9. Treatment |
| 9.1 First-line treatment: H1antihistamines at conventional doses 9.1 Second-line treatment: H1antihistamines at up to 4-fold the usual dose 9.3 Third-line treatment: cyclosporin or omalizumab at the recommended doses. Systemic corticosteroids should only be used for occasional flare-ups and for no longer than 10 d. |
| 10. Follow-up |
| Patient follow-up must include a thorough medical history and a physical examination. Severity and effects on quality of life should be scored (UAS7 and DQLI, respectively). |
Abbreviations: AE-QOL, Angioedema Quality of Life; CMU, clinical management unit; CSP, critical safety point affecting patients as listed by the health service of the government of Andalusia (the Junta); CU-Q2OL: Chronic Urticaria Quality of Life; DQLI: Dermatology Quality of Life index; EAACI/GA2LEN/EDF/WAO, European Academy of Allergy and Clinical Immunology/Global Allergy and Asthma European Network/European Dermatology Forum/World Allergy Organization; Ig, immunoglobulin; UAS7, Urticaria Activity Score 7.
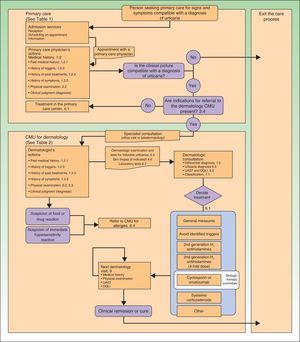
Table 1 (primary care) and Table 2 (specialized care) list the activities of multidisciplinary teams of health care and other professionals who attend the patient with urticaria as part of a coordinated process. The organization of the tables follows the patient's pathway through a system that includes both health care and related services. Aspects and dimensions of quality of care, clinical effectiveness, critical safety points (CSPs), nursing care, information-oriented CSPs, nonclinical interventions, and the recommendations of experts have been incorporated into the tables. The flow chart (Fig. 1) shows how specialist follow-up is carried out and offers a summary of a therapeutic approach rooted in the recently updated European guidelines.5
Methodology and LimitationsThe Metaplan approach10 that was used to draft this paper is a qualitative focus-group method for generating ideas and solutions, exploring opinions and reaching consensus; the focus groups also formulate objectives, make recommendations, and draft action plans. The method gathers information on cards that can be posted on a board to add a visual component to discussions. A moderator leads the group and structures the analysis and discussion in keeping with the context for the activity.
The intention is to foster the full participation of all members equally without the moderator exercising influence over individuals’ opinions. The method seeks to facilitate focus and foster understanding of ideas, using visual aids (posted cards) to expand on the spoken word. Gaps are left so that participants can fill them by suggesting new ideas to add to the board in an orderly way. Experts agree that these techniques break complex statements down into simpler ones, making them easier for participants to grasp. Complex ideas may even be condensed visually to only a single word or two, clarifying them and bridging gaps created during spoken communication.
The dermatologists who drafted the present paper came from all the provinces and health centers in the autonomous community of Andalusia. Support in applying the method was given by professionals from the Spanish Society for Quality in Health Care (SECA).
Finally, we note that the recommendations based on the consensus of experts with a wide range of clinical and management experience correspond to evidence level IV; this limitation applies to this paper.
ConclusionsIn conclusion, we propose a clinical pathway for urticaria, a condition that is commonly seen in dermatology practices. The dermatologist is clearly the best qualified specialist to manage patients with urticaria in an integrated way, in collaboration with allergy specialists, family practitioners, and other professionals. The dermatologist can confirm the diagnosis, ruling out possible alternative diagnoses such as other inflammatory or reactive skin conditions. The specialist can also assess severity and manage an exhaustive therapeutic plan that is well informed by appropriate clinical practice guidelines. The actions involved in clinical management, however, must be undertaken in an orderly way and in concert with other specialists and professionals. The patient, for whom continuity of care must be guaranteed, is at the center of this process. We believe the proposed clinical pathway is a dynamic starting point that will facilitate the approach we describe here.
| Overall definition of the process |
| Definition of the functions of the care process |
| Time frame: start point, end point and byways of the process |
| Persons responsible for care |
| Beneficiaries of care and aims of the process |
| Beneficiaries of care and expectations |
| Outcomes and exit points |
| Process components |
| Elements of the process and resources applied |
| Activities undertaken and quality-of-care characteristics |
| Flow-chart or graphic representation of the pathway |
| Structure of indications for care |
| Identification of the subgroup of patients with the condition (e.g., urticaria) who will undergo additional tests |
| Wait time before referring a patient to a specialist |
| Grouping of patients with the condition (e.g., urticaria) by severity and effect on quality of life (e.g., scoring with the UAS7 and DQLI, respectively) |
Abbreviations: DQLI, Dermatology Quality of Life Index; UAS7, Urticaria Activity Score 7.
Please cite this article as: Ruiz-Villaverde R, Moreno-Ramírez D, Galán-Gutierrez M, de Troya M, Reyes-Alcázar V, Alcalde M, et al. Proceso de atención al paciente con urticaria aguda y crónica. Documento de consenso de la sección territorial andaluza de la Academia Española de Dermatología y Venereología. Actas Dermosifiliogr. 2016;107:482–488.