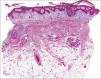
Can psoriasis cause irreversible alopecia? This was the question posed by one of our patients, a 21-year-old woman with no medical history of interest who had plaque psoriasis affecting the scalp, the upper part of the chest, and the midface area. Her condition, which had first developed more than 10 years earlier, was initially well controlled with topical drugs, but deteriorated rapidly when she was 18 years of age, causing significant psychosocial stress. Methotrexate, the first systemic treatment prescribed, was withdrawn due to poor tolerance. After that a very good response was achieved with ciclosporin, but her condition relapsed immediately when an attempt was made to reduce the dose. Ciclosporin was followed by etanercept, with minimal improvement; ustekinumab, which required frequent cycles of oral corticosteroids to control flares; and infliximab, to which she had a good response until the eighth cycle, when her condition became progressively more severe. The scalp was the site with the most severe and extensive lesions, and hair density was significantly reduced on the psoriatic plaques. When infliximab was discontinued, the patient was admitted to hospital to facilitate more intensive topical care and to start treatment with prednisone and methotrexate 12.5 mg/wk, a regimen that achieved significant improvement and good tolerance. Three months after the hospitalization, inflammation and scaling on the scalp were minimal, but the patient had large alopecic plaques on the parietal and temporal scalp, cicatricial in appearance. Histologic study of tissue from the edge of one of these plaques revealed psoriasiform epidermal changes, reduced hair follicle density, patchy peri-infundibular lymphocytic inflammatory infiltrate, and fiber tracts as well as absent and atrophic sebaceous glands (Fig. 1). After excluding other possible causes of alopecia (including bacterial and fungal superinfection), a diagnosis of psoriatic scarring alopecia was made. Two years later, the bald plaques persist, although partial repopulation has occurred (Fig. 2). The patient has continued to experience psoriasis outbreaks, which some months ago required treatment with a combination of adalimumab and methotrexate, a regimen that achieved partial control of the lesions.
Scarring alopecia associated with scalp psoriasis was first described by Shuster in 1972,1 but has not yet been fully accepted; major doubts require clarification. In recent editions of dermatology books, psoriatic alopecia is described as a form of nonscarring alopecia; however, some 20 cases of scarring alopecia related to psoriasis have been reported in the international literature (Table 1). The article by Runne and Kroneisen-Wiersma2 is the one that comes closest to the initial descriptive study by Shuster, encompassing the various clinical forms of alopecia in psoriasis, including a cicatricial type. Psoriatic scarring alopecia is usually characterized by a circumscribed pattern of hair loss and histology showing psoriasiform changes with perifollicular, or more specifically peri-infundibular, lymphocytic infiltrate and fibrous tracts. Atrophy of the sebaceous glands was initially described as characteristic of psoriatic plaques, with or without alopecia, but other authors have subsequently related this finding more specifically with psoriatic scarring alopecia.3 Also of note is the patchy follicular involvement, which would explain the subsequent hair repopulation, even when fibrosis is detected in the biopsy sample.
Characteristics of Reported Cases of Scarring Alopecia Associated With Psoriasis.
| Year | Authors | Cases | Psoriasiform | Fibrosis | Histology | Cultures | Follow-Up | Repopulation | |
|---|---|---|---|---|---|---|---|---|---|
| Perifollicular infiltrate | Sebaceous Gland Atrophy | Bacteria and fungi | |||||||
| 1972 | Shuster1 | 6 | Yes | Yes | Yes | No | Negative | 10 y | 1 patient |
| 1983 | Fernandes Rodrigues et al.4 | 1 | Yes | Yes | Lymphohistiocytic | No | Negative | — | — |
| 1990 | Wright and Messenger5 | 3 | Yes | Yes, patchy | Peri-infundibular lymphocytic | Yes | Negative | 3 mo | — |
| 1992 | Van de Kerkhof and Chang6 | 1 | Yes | Yes | Lymphohistiocytic | No | Negative | — | — |
| 1992 | Runne and Kroneisen-Wiersma2 | 5 | Yes | Yes, patchy | Peri-infundibular lymphocytic | Yes | Negative | — | — |
| 1995 | Kretzschmar et al.7 | 1 | Yes | Yes | Lymphohistiocytic | No | Negative | — | — |
| 1999 | Bardazzi et al.3 | 4 | Yes | Yes | Peri-infundibular lymphocytic | Yes | Negative | — | — |
| 2000 | Schön et al.8 | 1 | Yes | Yes, patchy | Lymphocytic | No | Negative | — | — |
| 2013 | Almeida et al.9 | 1 | Yes | Yes | Yes | Negative | 3 wks | — | |
| Our case | 1 | Yes | Yes, patchy | Lymphocytic peri-infundibular | Yes | Negative | 2 y | Partial | |
A more recent development is psoriatic alopecia induced by tumor necrosis factor (TNF) inhibitors. The prevalence of psoriasis as a paradoxical reaction to anti-TNF is estimated to be between 1.5% and 5%. It is considered to be particularly associated with infliximab and to frequently affect flexural areas and the scalp. Associated alopecia is exceptional, and scarring alopecia has been reported in only 1 case.10
The etiology and pathogenesis of psoriatic scarring alopecia is not clear and several questions arise. If psoriasis causes inflammation and abnormal keratinization of the epidermis, why does it not have the same effect on follicular epithelium and alter the maturation of hair follicles with dystrophic bulbs, fine hairs and predominance of hairs in the telogen phase. If inflammation is severe, it is not surprising that inflammatory cells should invade the follicular epithelium, leading eventually to its destruction. On the other hand, if neutrophils are one of the cells primarily involved in the psoriatic process, why is folliculotropic lymphocytosis observed? Neither can we ignore the possible role of external factors, such as scratching, superinfection and even the weight exerted by the thick scales on the scalp, which may impede the normal growth and maturation of the follicle.
In conclusion, psoriatic scarring alopecia is a rare and controversial condition which some authors consider to be a separate entity and others see as a secondary alteration. How then should we answer our patient's question? Does she have irreversible scarring alopecia? We do not know, and more clinical studies with histologic correlation and longer-term follow-up are needed. For the moment, for us and our patient, her condition is a “persistent” alopecia.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Gutiérrez García-Rodrigo C, Rivera Díaz R, Vanaclocha Sebastián F, Rodríguez Peralto JL. ¿La psoriasis produce alopecia irreversible?. Actas Dermosifiliogr. 2016;107:527–530.