Fungal infection is increasingly frequent among immunocompromised patients and is involved in potentially fatal conditions, mainly as a result of the baseline status of the patient affected. Recent years have seen reports of cases caused by less common fungi that are highly resistant to antifungal drugs. Such cases require a high index of suspicion and rapid initiation of treatment to prevent the expected outcome.
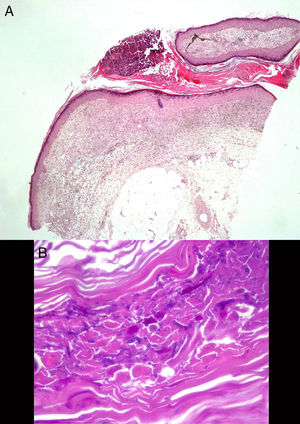
We report the case of an 82-year-old man who came to the emergency department at our center with a 6-week history of pruriginous skin lesions that first appeared on the dorsum of the left hand and progressed upwards. The patient had previously been a heavy smoker, and his history was remarkable for type 2 diabetes mellitus, prostate cancer (for which he was receiving palliative treatment), and chronic lymphatic leukemia. He was receiving treatment with insulin glargine and oxycodone/naloxone. He reported that his condition had worsened despite topical antifungal treatment and various oral antibiotics that were started by his primary care physician, as well as local treatments. He denied having fever and relevant systemic symptoms. The examination revealed a well-defined erythematous-violaceous plaque on the dorsum of the left hand. The plaque was slightly infiltrated, with multiple pustular and crusted lesions on the surface, and was spreading in a sporotrichoid pattern over the dorsum of the forearm, where ulcerated lesions alternated with fluctuant violaceous nodules that were seeping purulent exudate (Fig. 1 A and B). The most notable findings of the laboratory workup performed in the emergency department were a minimum increase in C-reactive protein concentration (0.8mg/dL) and mild neutrophilia (8980/μL) without leukocytosis. The chest radiograph revealed a cavitated nodule in the middle field of the left lung. A review of the tests carried out in primary care revealed a fungal culture in which Scedosporium apiospermum complex was isolated, with a minimum inhibitory concentration of 1 for voriconazole. The patient was diagnosed with sporotrichoid lymphocutaneous fungal infection and admitted because of possible disseminated infection while immunosuppressed. Treatment was started with oral voriconazole at 400mg/12h on day 1 and 200mg/12h on the following days. Histopathology revealed a sinus tract filled with hyperkeratotic material, with a pustule on the surface. Periodic acid-Schiff staining revealed mytotic structures in the form of spores and hyphae with clear 45° branching (Fig. 2). Tissue culture confirmed isolation of S apiospermum and was negative for bacteria and mycobacteria. The antifungal susceptibility profile confirmed sensitivity to voriconazole. The result of polymerase chain reaction assay with Sporothrix schenckii and mycobacteria was negative. The patient's skin complaint progressed favorably, with crusting lesions that replaced the pustules on the dorsum of the hand and ulcerated lesions instead of nodules on the forearm. Computed tomography of the chest confirmed the presence of a cavitated nodule in the left lower lobe and other, smaller nodules that were probably fungal in origin (given the patient's baseline status and after agreement with his family, we decided against further testing). Nevertheless, the possibility of endocarditis with septic embolism was ruled out using transthoracic echocardiography. During admission, the most remarkable observation was severe voriconazole-induced hyponatremia, which resolved gradually with fluid and electrolyte therapy and temporary suspension of the drug. Onset of self-limiting episodes of visual hallucinations necessitated cranial computed tomography, which ruled out fungi in the parenchyma. Therefore, the episodes were considered part of a multifactorial confusional state. The favorable laboratory outcome and clinical course led us to discharge the patient after reintroducing voriconazole. The bullous and nodular lesions disappeared after 22 days of intravenous treatment, leaving residual purpuric lesions (Figs. 1C and D), and the follow-up radiograph revealed complete cavitation of the lung nodule.
A and B, Well-defined infiltrated erythematous-violaceous plaque on the dorsum of the hand, with pustular and crusted lesions on the surface. Nodular and ulcerated lesions distributed in a sporotrichoid fashion on the forearm. C and D, Lesions resolving in the form of purpuric macules and crusted debris on the dorsum of the hand and forearm.
S apiospermum is a ubiquitous mold found throughout the world. It is isolated in rural soil, contaminated water, and cattle and bird excrement. It mainly infects immunosuppressed patients,1 in whom it more frequently disseminates through the bloodstream. The main routes of transmission are direct inoculation via the skin and inhalation of spores.2 The main targets are the skin, the lungs, and the central nervous system.2 The most widely reported skin manifestations are bullous necrotic purpura3,4 and the spirotrichoid form,5,6 both of which occurred together in the case we present. A high index of suspicion, early diagnosis, and rapid initiation of treatment are essential if we are to improve a prognosis that is already poor. Although histology was unable to identify the pathogen, it was complemented with a positive culture (whitish colonies that progress to grayish and brownish colonies [Fig. 3]) in order to establish the diagnosis. In addition, the extension study reveals the presence of invasive fungal infection.7 Therefore, skin involvement is essential for identification of the condition and for the need to speed up therapeutic procedures (see above). Monotherapy with voriconazole is postulated as the antifungal drug of choice depending on the resistance detected,8 although dosing and duration of treatment have not been established. Despite efforts made to date, mortality continues to be high (40%-100% depending on the series).8,9
We present a case of opportunistic infection by S apiospermum, a little-known pathogen with a peculiar clinical presentation that has not yet been reported in Spain. A multidisciplinary approach is essential owing to the poor baseline status of affected patients, the need to use highly toxic drugs, and the eventual associated systemic complications. In this sense, the dermatologist may play a fundamental role in early diagnosis and survival.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Company-Quiroga J, Martínez-Morán C, Moreno A, Borbujo J. Púrpura bullonecrótica de distribución esporotricoide por Scedosporium apiospermum. Actas Dermosifiliogr. 2018;109:374–376.