An 88-year-old man with no history of interest came to the clinic with pruritus and vesicles on both hands that had first appeared 5 days earlier. He had not previously experienced insect bites or injury and had had no previous history of lesions of this type. Physical examination revealed the presence of multiple, tense vesicles that were round-oval in shape and contained a serous or serosanguineous fluid. They were scattered over the palms and wrists, although the thenar and hypothenar eminences were spared (Fig. 1). The vesicles were frequently on areas of erythematous-edematous skin. No similar lesions were found on other areas of the body or on the mucous membranes.
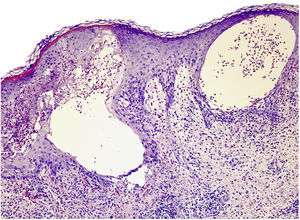
We therefore decided to order a biopsy. We obtained 2 skin fragments for study with hematoxylin-eosin staining and direct immunofluorescence. Examination of the biopsy specimen revealed an orthokeratotic epidermis with irregular acanthosis, marked exocytosis of eosinophils, and spongiosis with spongiotic vesicles. The superficial and mid dermis revealed perivascular dermatitis comprising a mixed infiltrate that was mainly lymphocytic with abundant eosinophils (Fig. 2).
What is your diagnosis?
DiagnosisDyshidrosiform bullous pemphigoid (DBP).
Clinical Course and CommentDirect immunofluorescence revealed the presence of linear deposits of immunoglobulin (Ig) G and complement component C3 (C3) in the basement membrane. The clinical and pathological findings enabled us to confirm a diagnosis of DBP. We initiated treatment with oral prednisone (0.5mg/kg), together with topical zinc sulfate 1/1000 and clobetasol dipropionate cream, once per day. The lesions improved significantly after 5 days.
DBP is a rare variant of bullous pemphigoid that was first described in 1979 by Levine et al.1 It most commonly affects elderly patients, and its etiology is unknown. DBP is characterized by tense blisters with clear and often hemorrhagic content, which are found initially or exclusively on the palms and soles. In some cases, the blisters develop after pruritic eczematous or urticarial lesions, whereas in others, the urticarial lesions persist without formation of blisters. Bullous pemphigoid is characterized by subepidermal blisters with abundant eosinophils in histopathology. However, intradermal spongiotic vesicles with eosinophils in the interior may also be present.2 This phenomenon, which is known as eosinophilic spongiosis, is characterized by intercellular edema composed of an inflammatory eosinophilic infiltrate. It constitutes a reactive pattern in the epidermis that is observed in a wide range of skin conditions.3 According to Crotty et al.,3 this histopathological finding is very frequently associated with bullous pemphigoid. Nevertheless, additional histopathological criteria must be fulfilled before the diagnosis of bullous pemphigoid can be confirmed.
As with bullous pemphigoid, DBP is characterized by linear deposits of IgG and C3 in the basement membrane. The lesions frequently resolve with residual hyperpigmentation, although without scarring or milia.4 Treatment consists of topical or systemic corticosteroids according to the severity and/or extension of the process and the disease. The disease can progress via 3 different pathways: (a) the bullous lesions remain confined to the palms and soles; (b) onset is in acral regions of the palms and soles, with subsequent extension to the rest of the skin; and (c) concomitant appearance of lesions on the palms and soles, together with generalized lesions.5 The patient in the present case is in complete remission, with no new vesicles on the palms or soles or on other areas. Residual hyperpigmentation persisted for several weeks.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Conde-Ferreirós A, Santos-Briz Terrón Á, Cañueto J. Lesiones ampollosas en las palmas. Actas Dermosifiliogr. 2020;111:321–322.