An otherwise healthy 15-year-old boy from a rural area of Catalonia came to the clinic for a periodic check-up of his acne. Examination of the patient's torso revealed several asymptomatic brownish erythematous circular plaques. The patient was unsure of when they first appeared. He denied having taken drugs, recent travel, contact with animals, and flea bites.
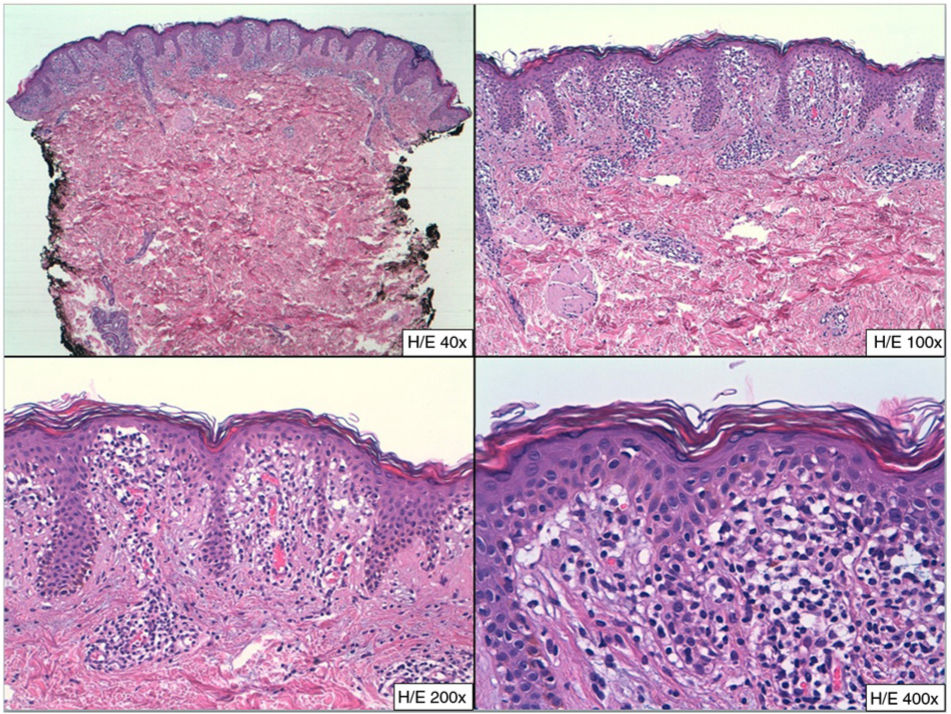
Physical ExaminationPhysical examination revealed a nonscaling brownish erythematous annular plaque on the skin of the upper abdomen with central hypopigmentation and various isolated smaller circular macules on the abdomen, proximal part of the arms (Fig. 1), and back. The face, palms, and soles were spared, as were the mucous membranes. The affected skin was neither atrophied nor indurated, and sensitivity was unaltered.
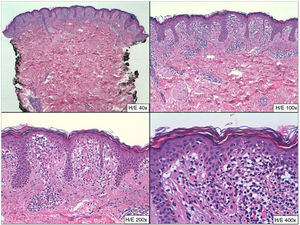
HistopathologyFig. 2 showed a dense lichenoid infiltrate on the tips of the papillae and numerous necrotic keratinocytes. Also visible was a chronic perivascular infiltrate in the superficial dermis. No granulomas, atypical lymphocytes, dermal fibrosis, or vasculitis were observed. Periodic acid–Schiff staining was negative.
Additional TestsThe results of the complete blood count and biochemical tests were normal, and serology for Borrelia species was negative.
What is your diagnosis?
DiagnosisAnnular lichenoid dermatitis of youth (ALDY).
Treatment and Clinical CourseGiven the diagnosis of ALDY, we prescribed clobetasol propionate 0.1% cream for 4 weeks. This led to complete resolution of the lesions. The patient remained free of lesions until the last check-up, which was 6 months after the lesions had resolved.
DiscussionALDY is an uncommon condition whose etiology and pathogenesis are unknown. It forms part of the broad group known as lichenoid dermatitis, and diagnosis is necessarily based on the correlation between clinical and histopathologic findings. The condition is probably underdiagnosed, with only 46 cases reported in the literature since it was first described in 2003. ALDY generally affects children and adolescents—it is rare in adults—most frequently from the Mediterranean area, with a slight predominance in males.1 Clinically, it presents as annular erythematous plaques or macules with a whitish center mainly affecting the trunk. It is usually asymptomatic. The clinical differential diagnosis is broad and is mainly with morphea, deep erythema annulare centrifugum, mycosis fungoides, tinea corporis, chronic migratory erythema, scleroatrophic lichen, granuloma annulare, and even sarcoidosis.
The correlation between clinical and histopathological data is essential. Histologically, ALDY presents as lichenoid dermatitis affecting mainly the dermal papillae and associated with a mild chronic perivascular inflammatory infiltrate in the superficial dermis. The infiltrate is predominantly CD3+ and CD4+, and in some cases, exocytosis of lymphocytes may be observed. When the condition could be confused with mycosis fungoides, it is necessary to perform a clonal rearrangement study, which should yield a negative result.2 Also useful is the frequent finding of CD20 positivity in the ALDY infiltrate; this is usually negative in mycosis fungoides.3
While benign and usually self-limiting, it can be treated successfully with both topical and oral corticosteroids.2 Phototherapy, topical calcineurin inhibitors, and oral antibiotics can be used in the most refractory cases.4
A recent study of 14 patients in western Austria pointed to a possible association between ALDY and Borrelia burgdorferi.3 The authors detected spirochetes in 11 of the 14 samples and a positive result in 9 of the 12 serology tests performed. In fact, 1 patient diagnosed with ALDY eventually had plaque morphea. Therefore, the authors suggested that B burgdorferi could play a role in the etiology or even that ALDY could be an incipient phase of morphea. In the case we present, the association with B burgdorferi was ruled out by serology testing.
We report a typical case of ALDY, with classic clinical and histopathological characteristics that enable us to present an uncommon condition about which we still have much to learn.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mir-Bonafé JF, Claret-de Castro A, Rozas-Muñoz E. Placas anulares en el tronco de un adolescente. Actas Dermosifiliogr. 2020;111:319–320.