Aggressive carcinomas of the scalp usually occur in elderly patients with multiple comorbidities. Complete excision of this type of tumor often involves the removal of periosteum, and the resulting defects can be difficult to reconstruct.
ObjectiveTo evaluate the usefulness of porcine type I collagen dressings as adjunct or definitive treatment in the surgical closure of scalp defects without periosteum.
Materials and methodsWe performed a prospective study between January 2009 and November 2011 of patients with scalp defects larger than 5cm resulting from surgery that required the removal of periosteum to obtain tumor-free margins.
ResultsThe most prevalent type of tumor was recurrent cutaneous squamous cell carcinoma. The surgical defects ranged in diameter from 5 to 7cm. In 100% of the patients who received a graft after dressing removal (n=4), the graft took well. In the patients in whom the biosynthetic dressing was definitive (n=6), granulation tissue filled the defect and complete closure was achieved in approximately 3.5 months.
ConclusionsThe use of porcine type I collagen dressings as an adjunct or definitive tool for the closure of surgical defects on the scalp measuring more than 5cm in which periosteum has been removed proved to be simple, inexpensive, and effective.
Los carcinomas cutáneos agresivos que aparecen en el cuero cabelludo se desarrollan habitualmente en pacientes de edad avanzada que presentan múltiples comorbilidades.
La exéresis completa de estos tumores incluyen en muchos casos al periostio, lo que conlleva que la reconstrucción de este tipo de defectos se convierta en un reto.
ObjetivoSe evalúa la utilidad de un parche de colágeno porcino tipo I como tratamiento coadyuvante o definitivo en el cierre quirúrgico de este tipo de defectos cutáneos.
Material y métodosSe realizó un estudio prospectivo en el que se incluyeron aquellos pacientes que presentaron defectos de más de 5cm en el cuero cabelludo en los que el periostio tuvo que ser extirpado para alcanzar márgenes libres de enfermedad entre enero de 2009 y noviembre de 2011.
ResultadosLa tumoración más prevalente fue el carcinoma epidermoide cutáneo recurrente. El defecto postquirúrgico osciló entre 5 y 7cm de diámetro. En el grupo de casos en los que se colocó un injerto post-parche (n=4), en el 100% de los casos el tejido prendió completamente. En el caso de aquellos pacientes en los que el parche fue el recurso definitivo (n=6), el tejido de granulación generado por el material biosintético de colágeno porcino ocupó el defecto quirúrgico dejándolo completamente restituido en aproximadamente 3,5 meses.
ConclusionesEl parche de colágeno porcino tipo I es una herramienta sencilla, barata y eficaz en el tratamiento coadyuvante o definitivo del cierre de defectos quirúrgicos del cuero cabelludo de más de 5cm que carecen de periostio.
Aggressive cutaneous carcinomas of the scalp typically occur in elderly patients with multiple comorbidities.
In the majority of cases, complete excision of this type of tumor, generally performed using Mohs micrographic surgery, leaves a large surgical defect in which it will have been necessary to excise the periostium in order to achieve disease-free margins.
The periostium, also known as the pericranium, is a dense connective tissue membrane of tough, fibrous vascular tissue that covers the external surface of the bone. Reconstruction of these types of defect can be a surgical challenge after resection of this membrane, as the base of the defect is left with almost no vascular supply.
The most logical approach to the closure of such a defect would be a skin flap. However, these tumors typically present high recurrence rates, and distortion of the tissues could therefore mean that recurrences might be missed. Grafting would thus appear to be the most recommendable option, but the limited vascular supply of the skin defect would lead to a high risk of necrosis.
We present a study to evaluate the usefulness of a biosynthetic patch formed of silicone and porcine type I collagen as a method to induce neovascularization on bone devoid of periostium; this new vessel formation would enable the defect to be closed either by second intention or by the placement of a skin graft in a second operation.
Material and MethodsStudy PopulationA prospective study was performed that included all patients seen between January 2009 and November 2011 in the dermatology department of the Fundación Instituto Valenciano de Oncología, Valencia, Spain, with scalp defects greater than 5cm in diameter in which excision of the periostium had been required to achieve disease-free margins.
All patients received detailed information about the study from the investigator in an understandable language, both orally and as a written informed consent form. The study was approved by the institutional review board of the referring hospital.
Description of the Porcine Type I Collagen Biosynthetic Patch (Biobrane)Biobrane is a porous semisynthetic patch that first came onto the market in 1979. It consists of 2 minimally separated membranes; the external layer is silicone, which reduces evaporative water loss from the defect, and the internal layer is formed of a matrix of nylon and porcine type I collagen. The minute pores of the silicone membrane make it permeable to topical antimicrobial products.1,2 This type of patch has mainly been employed in the management of burns patients,3 although there are also reports of its use to treat patients with other conditions, such as toxic epidermal necrolysis, paraneoplastic pemphigus, and bullous epidermolysis.4,5
Method of ApplicationThe biosynthetic patch was placed directly on the bone without periostium and was anchored using 4 silk sutures at equal distances. A topical antibiotic cream or ointment was then applied with the double intention of preventing infection and stopping the patch from adhering to the granulation tissue when this appeared. The patch was then covered with a tulle or silicone dressing and a simple bandage.
Wound Care After Placement of the PatchWound care of the surgical defect was performed by the nursing staff of the dermatology unit until complete closure of the defect; this was done weekly for the first month, every 2 weeks during the second month, and monthly thereafter, until the defect had closed completely.
Selection of Patients for Definitive Closure by Second Intention or by Partial-Thickness Skin GraftingThe criteria used to determine whether definitive closure was to be achieved with the patch or with the subsequent placement of a graft in a second surgical intervention are listed in Table 1.
Criteria for Selection of Closure Technique in Patients Treated Using the Biosynthetic Patch.
| Closure by Second Intention | Two-Stage Closure With Graft Placement |
| Age >65 yTwo or more cardiovascular risk factorsaPast history of cardiovascular or cerebrovascular accidentPoor general state of healthPatient refusal to undergo a second operationUsual skin donor sites already used | Age ≤65 yConcern for the cosmetic resultGood general state of health |
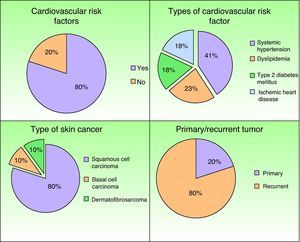
Ten patients (5 women and 5 men aged between 34 and 90 years; mean age, 62 years) were included in the study (Tables 2–4). Cardiovascular risk factors, most frequently systemic hypertension, were detected in 62% of patients (Fig. 1). The most common scalp tumor was squamous cell carcinoma (8 cases), followed by basal cell carcinoma (1 case) and dermatofibrosarcoma protuberans (1 case). In 80% of cases, the tumors were recurrences of a primary tumor previously excised using conventional surgery (Fig. 1). The most common site of the tumor was the frontal region (in5 patients), followed by the parietal region (3 patients) and the occipital region (2 patients). Mohs micrographic surgery had been used in all patients included in the study, and disease-free margins had been achieved. The size of the resulting surgical defects varied between 5×5cm and 8×7cm (mean,5.85×5.45cm).
Characteristics of the Patients Included in the Study.
| Case No./Age, y/Sex | Cardiovascular History | Smoking/Alcohol | Tumor Treated (Primary/Recurrent) | Initial Size of the Surgical Defect, cm | Site | Objective of the Biosynthetic Patch |
| 1/62/M | Systemic hypertension | No | Squamous cell carcinoma (recurrent) | 5×5 | Frontal | Definitive closure |
| 2/67/M | DyslipidemiaImmunosuppressants for liver transplant | No | Squamous cell carcinoma (recurrent) | 7×7 | Frontal | Definitive closure |
| 3/89/M | Systemic hypertensionIschemic heart disease | No | Squamous cell carcinoma (recurrent) | 7×6 | Frontal | Definitive closure |
| 4/75/M | Systemic hypertensionType 2 diabetesDyslipidemia | No | Squamous cell carcinoma (primary) | 7×7 | Occipital | Definitive closure |
| 5/54/F | Systemic hypertension | Yes (smoking, 1 packet/day) | Basal cell carcinoma (recurrent) | 8×7 | Occipital | Two-stage surgery |
| 6/90/F | Systemic hypertension | No | Squamous cell carcinoma (recurrent) | 5.5×5 | Frontal | Definitive closure |
| 7/84/F | Systemic hypertensionType 2 diabetesDyslipidemiaIschemic heart disease | No | Squamous cell carcinoma (recurrent) | 5×5 | Frontal | Definitive closure |
| 8/34/F | No | No | Dermatofibrosarcoma (primary) | 7.5×5.5 | Parietal | Two-stage surgery |
| 9/60/M | Systemic hypertensionType 2 diabetesDyslipidemiaIschemic heart disease | No | Squamous cell carcinoma (recurrent) | 7×7 | Parietal | Two-stage surgery |
| 10/50/F | No | No | Basal cell carcinoma (recurrent) | 5×5 | Parietal | Two-stage surgery |
Abbreviations; F, Female; M, male.
Characteristics of the Patients in Whom the Biosynthetic Patch Was Used as the Method of Definitive Closure.
| Case No./Age, y/Sex | Time to Initiation of Granulation, d | Time to Complete Closure, d | Patient Satisfaction (Scale of 0 to 10) | Complications During Wound Care | Follow-up After Complete Closure, mo | Complications During Follow-up |
| 1/62/M | 22 | 110 | 10 | Hypergranulation | 6 | No |
| 2/67/M | 14 | 100 | 10 | No | 14 | No |
| 3/89/M | 18 | 121 | 9 | No | 10 | No |
| 4/75/M | 9 | 95 | 9 | No | 19 | Recurrence, retreatment and definitive closure with a patch |
| 6/90/F | 15 | 130 | 10 | Hypergranulation | 5 | No |
| 7/84/F | 18 | 134 | 9 | No | 10 | No |
Abbreviations: F, Female; M, male.
Characteristics of the Patients in Whom the Biosynthetic Patch Was the Intermediate Step Before Placement of a Partial-Thickness Skin Graft to Cover the Defect.
| Case No./Age, y/Sex | Complications During Wound Care | Time to Initiation of Ganulation, d | Interval Between Operations, d | Graft Necrosis | Patient Satisfaction, (Scale of 0 to 10) | Follow-up After Complete Closure, mo | Complications During Follow-up |
| 5/54/F | No | 16 | 40 | No | 10 | 26 | Recurrence, retreatment and definitive closure with a patch, with complete closure |
| 8/36/F | No | 19 | 35 | No | 10 | 12 | No |
| 9/85/M | No | 20 | 35 | No | 10 | 12 | No |
| 10/50/F | No | 20 | 31 | No | 10 | 13 | No |
Abbreviations: F, Female; M, male.
In all cases, granulation tissue started to appear in the base of the defect between 9 and 22 days (mean, 17.1 days) after placement of the biosynthetic patch.
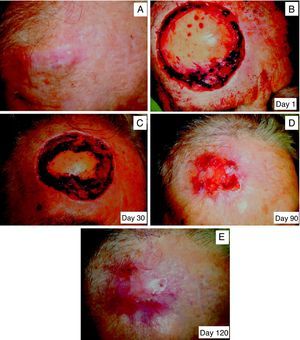
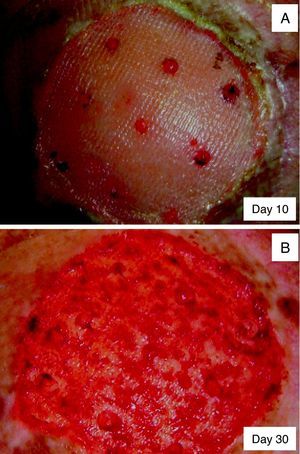
The patch of porcine type I collagen was used as the definitive means to achieve closure by second intention in 6 cases (Table 3). The mean time from placement of the patch until closure of the defect varied between 95 and 134 days (mean,115 days) (Fig. 2, A-E). The only complication was the appearance of hypergranulation in 2 patients, but this was easily resolved using silver nitrate (Fig. 3, A and B).
A 69-year-old patient who underwent excision of a recurrent cutaneous squamous cell carcinoma. A, Initial lesion. B, Mohs micrographic surgery (scheduled surgery) requiring 3 stages to achieve disease-free margins. C, Day 30 after application of the biosynthetic membrane, Biobrane. D, Day 90 after the application of the biosynthetic membrane. E, Day 120; complete epithelialization of the defect.
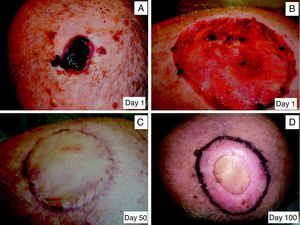
In 4 patients, the biosynthetic patch was used as a co-adjuvant device, and the defect was subsequently closed by placement of a partial-thickness skin graft. The time between placement of the biosynthetic patch and placement of the skin graft varied between 31 and 40 days (mean,35.25 days). The vascular supply of the graft was adequate in all cases, and none of the grafts presented necrosis during the follow-up period (Fig. 4, A-D).
An 81-year-old patient who underwent excision of a recurrent cutaneous squamous cell carcinoma. A, Initial lesion. B, Skin defect during the granulation phase. C, Placement of a skin graft. D, Eighty days after grafting; there is an area of radiodermitis secondary to the adjuvant radiation therapy.
Patients were followed up for a mean of 12 months after complete closure of the defect was achieved. During that time, 2 patients (cases 4 and 5) with squamous cell carcinoma developed lesions that were clinically and histologically compatible with recurrence, requiring further operation. Closure of the defects was once again performed with the biosynthetic patch used as the definitive method of closure, with excellent results.
DiscussionThe scalp is defined as the anatomical area located over the cranium, above the neck and the orbital line. The soft tissues that cover this area are the thickest of all the body surface and are divided into 6 layers: skin, subcutaneous cellular tissue, aponeurosis or galea, areolar tissue (which unites the galea with the periostium, permitting movement), periostium or pericranium, and bone. The blood supply to the scalp depends principally on the subcutaneous cellular tissue and periostium.6
Large scalp defects are most commonly due to the surgical treatment of malignant skin tumors, typically squamous cell carcinoma and basal cell carcinoma, and to neurosurgical interventions of various types. In addition, the dense vascular network in this region means that the scalp is a common site for skin metastases that may require surgical excision.7
The complexity of the reconstruction of surgical defects of the scalp varies according to whether the defects are small or large. Direct closure is usually used for small defects (diameter <3cm) in patients with a good general state of health.8 In these cases the primary objective is to comply with certain cosmetic requirements, such as preservation of the hairline and symmetry of the eyebrows and ensuring the absence of bald patches.9
In the case of large scalp defects (diameter ≥3cm) there is a series of factors that must be analyzed in order to determine the most appropriate reconstruction technique (Table 5).10–12 The main techniques used to close these defects include skin flaps with or without tissue expanders, partial- or full-thickness skin grafts, and microvascular fascial and myocutaneous skin grafts.13–15 The majority of these scalp defects can be closed using these techniques. However, when the excision of an aggressive tumor has required resection of the periostium and has left a large surgical defect, the requirements for safe and effective reconstruction using the aforementioned techniques are not satisfied (Table 6). For example, a complex case would be one requiring closure of a defect whose largest diameter is greater than 5cm, created by the excision of a recurrent tumor that invaded the periostium in a patient over 65 years of age. In such cases, a skin flap would not be advisable due to its complexity, the possible comorbidities, the aggressive nature of the surgical reconstruction, and the risk of recurrence of the malignant skin tumor within 5 years of treatment.16 In this type of tumor, the ideal approach would be a skin graft, but resection of the periostium would mean that the vascular bed necessary for the graft to take and not to necrose would be absent. A valid, safe, and effective alternative is therefore necessary.
Factors That Inhibit Vascularization of the Surgical Defect.
| Past history | Age >65 yPresence of cardiovascular risk factors (dyslipidemia, diabetes mellitus, systemic hypertension)History of ischemic heart disease or myocardial infarctionHistory of transient ischemic attack or cerebrovascular accidentSmoking/alcohol/recreational drugs |
| Type of tumor excised | Recurrent tumorTumors with infiltration of the periostium |
| State of the perilesional skin | Previously operated skinSkin treated using radiation therapy |
Advantages and Disadvantages of the Different Techniques for Reconstruction of a Scalp Defect Greater Than 5cm in Diameter That Lacks Periosteum.
| Advantages of a flap | Disadvantages of a flap |
| Blood supply | Risk of failure with age >65 y |
| Acceptable cosmetic result | Risk of failure due to associated comorbidities |
| Moderate technical complexity | Risk of necrosis due to excessive tissue tension |
| Interference with early detection of tumor recurrence | |
| Advantages of a skin graft | Disadvantages of a skin graft |
| Simple technique | Suboptimal cosmetic result (depression in the area of the graft) |
| No interference with early detection of tumor recurrence | High risk of necrosis of the graft due to limited or absent vascular supply |
| Advantages of the biosynthetic patch | Disadvantages of the biosynthetic patch |
| Induction of new blood vessel formation directly on the bone despite: | Price (biosynthetic patch, 55 Euro) |
| - Age | - Periodic wound care by qualified nursing staff |
| - Comorbidities | |
| - Multiple operations | |
| - Absence of periostium | |
| Acceptable cosmetic result | Time to closure with second intention healing (3.5 mo) |
| Simple technique | |
| No interference with early detection of tumor recurrence | |
The substitute skin patch, specifically the dermal regeneration template, has been used for 3 decades to reconstruct large surgical defects of the scalp.17,18 This material, composed of cross-linked bovine collagen and chondroitin-6-sulfate, achieves good results in the closure of scalp defects that lack periostium. However, the fact that it is necessary to perforate the bone in such cases in order to achieve a good vascular bed to supply the patch, associated with the need for specific methods of subsequent wound care involving the use of a negative pressure (VAC) system, and the high price of this material, means that this method of closure is not usually used.17,18
The biosynthetic silicone patch with porcine type I collagen (Biobrane), not previously used for the repair of large scalp defects, is an excellent alternative. The biological component of the dressing is able to generate new blood vessels in the base of the defect and, in contrast to other biosynthetic materials, it does not require perforation of the cranium when applied. The success rate achieved with this method (100% in our series) is better than that achieved with closure using a full-thickness skin graft, which requires perforation of the external table of the cranium (success rate, 28%), or closure using a skin flap with tissue expanders, which requires reoperation in up to 14% of cases.13–15 The bovine-collagen biosynthetic patch is more costly and more complicated to apply (need for cranial perforation), and is not superior to Biobrane in terms of efficacy or efficiency.17,18
The method of application is relatively simple, as the patient does not require any initial preparation and the biosynthetic patch is placed directly on the cranium devoid of periostium, without the need for perforation of the bone. Granulation tissues starts to appear in the base of the defect within an average of 2 weeks, and it characteristically grows from the periphery of the defect towards the center, though oval reddish islets of granulation tissue can also develop over the bone surface (Fig. 5). This would suggest that the patch induces the formation of new capillary blood vessels from the borders of the defect as well as from the very limited vascular supply of the bone in the base of the defect, leading to the production of a neoperiostium. This means that it is advisable to follow up patients who have been treated using a biosynthetic patch.
Patients can live life as usual while the patch is in place, but it is essential that they return to the dermatology clinic for the necessary wound care. Nursing staff at these clinics must therefore be familiar with this material and follow the postsurgical wound care protocol described below. Wound care must initially be performed weekly, as the patch must be removed immediately after the formation of granulation tissue in the base to prevent the formation of areas of hypergranulation that would impede closure (Fig. 3). Closure occurs concentrically from the periphery and, as it progresses, the nursing staff trim the patch from the areas where granulation tissue has developed, leaving the material in the areas still to regenerate. After the fifth week, by which time the base of the defect will be completely covered by granulation tissue and the patch will have been completely withdrawn, wound care can be performed every 2 weeks and the decision can be taken on whether to allow closure by second intention or to perform further surgery to cover the defect with a partial-thickness skin graft (Tables 2–4).
The main complication of the use of the porcine type I collagen biosynthetic patch is hypergranulation of the base of the defect, though this is easily corrected with topical silver nitrate (Fig. 3). The risk of infection is very low if the usual hygiene measures for care of a simple wound are followed.
The main limitation of this closure technique is the need for trained staff to perform the initial wound care after application of the patch, following the steps described above, though in daily practice this is simple.
In view of the aggressiveness of the tumors treated, patients should continue to be followed up closely after closure of the skin defect. In our series, 2 patients (cases 4 and 5) presented clinical and pathologic findings compatible with local recurrence at 4 and 6 months, respectively, after complete closure of the defect, and further surgical intervention was therefore required. Closure of the defects was once again achieved through the use of the biosynthetic patch in both cases, allowing the defects to heal by second intention; the same optimal results of closure were achieved as after the first operation.
The main limitation of this study is the small number of cases presented. However, as reconstruction of large defects devoid of periostium is uncommon, we consider that the conclusions drawn from this group of patients could be useful to surgical practice.
In summary, in the last decade, the increase in life expectancy means that, in daily practice, we can meet elderly patients with multiple comorbidities who develop locally aggressive tumors in chronically sun-exposed areas, especially the head. The excision of these tumors leaves large skin defects whose reconstruction is a major surgical challenge. Based on the results of our study, we can assert that the silicone patch with porcine type I collagen is a simple, inexpensive device that is an effective coadjuvant or definitive treatment for closure of surgical defects of the scalp of more than 5cm diameter that lack periostium. The use of these patches will reduce the need for aggressive surgery in elderly patients with multiple comorbidities, and will enable any tumor recurrence to be detected early.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Martorell-Calatayud A, et al. Parche biosintético de colágeno porcino como herramienta coadyuvante o definitiva en el cierre de defectos del cuero cabelludo sin periostio. Actas Dermosifiliogr. 2012;103:887–96.