Evaluation of disease severity is considered essential in the optimal management of psoriasis.
ObjectivesTo describe the clinical characteristics and therapeutic profile of patients with moderate to severe psoriasis in Spain and to assess the impact of the disease on the patients’ quality of life.
Materials and methodsThis was an observational, cross-sectional study carried out in 90 dermatology units in Spain in 2009. We included 442 patients diagnosed with moderate to severe psoriasis who had started treatment with systemic agents, phototherapy, and/or topical treatments between 2004 and 2006.
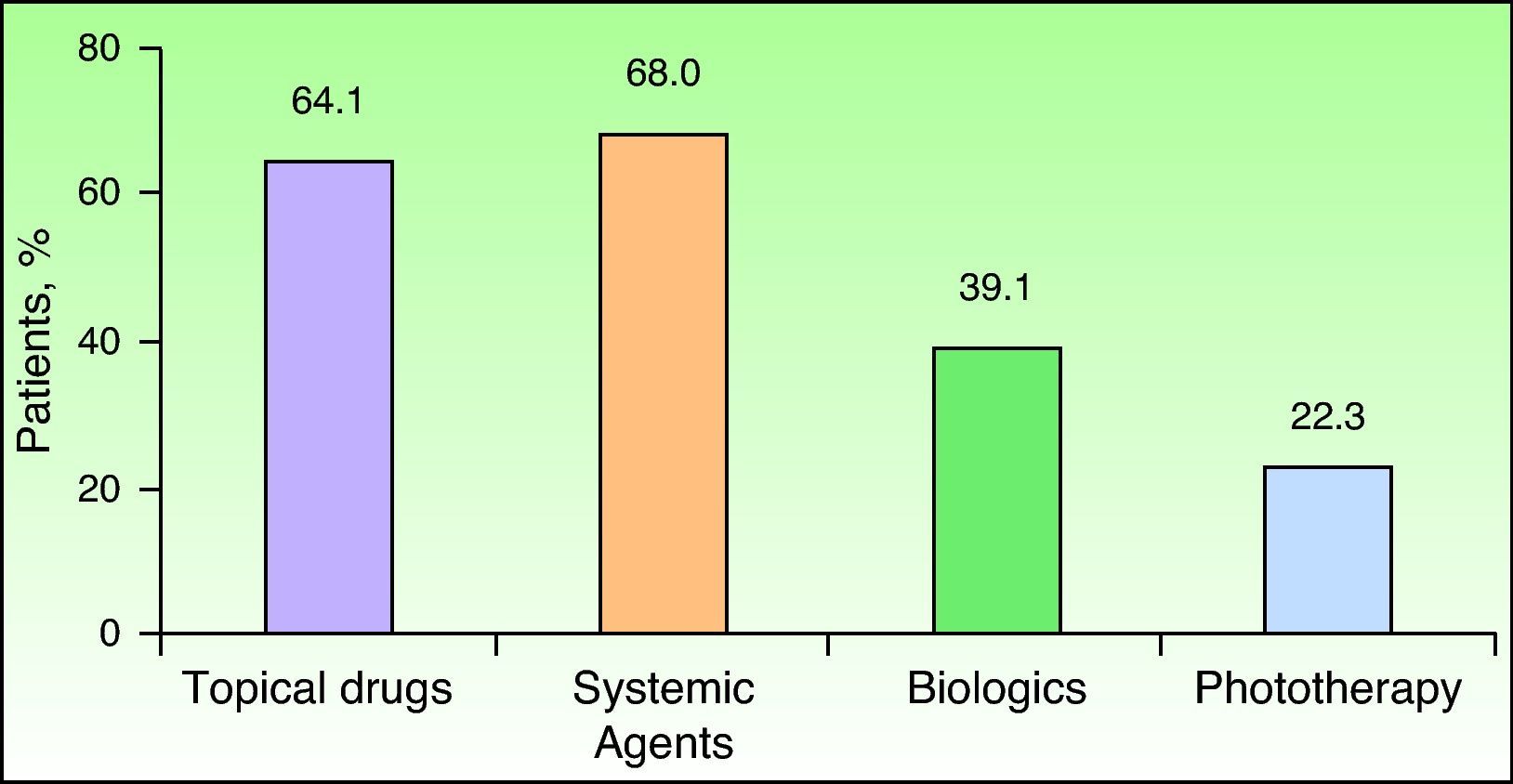
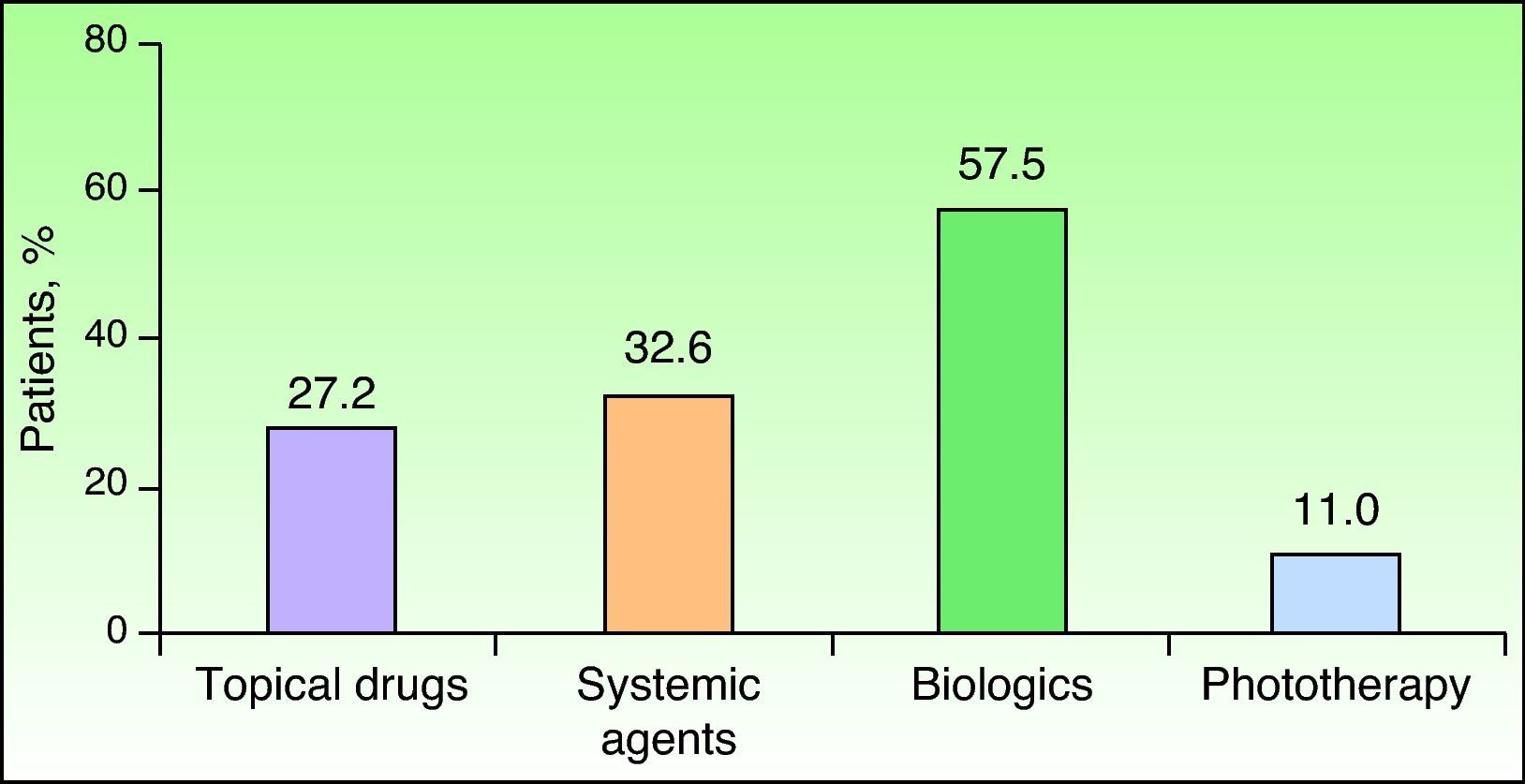
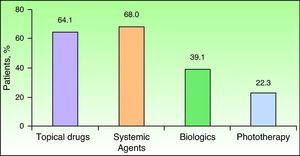
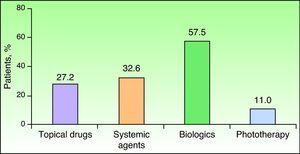
ResultsMore severe psoriasis was significantly associated with the following: longer disease duration; higher prevalence of concomitant disease; greater involvement of the nails, scalp, flexures, palms, and soles; and poorer quality of life. In the 5 years before the start of the study, 68% of the patients had received conventional systemic treatments, 39.1% biologic agents, and 22.3% phototherapy. At present, 57.5% of the patients are being treated with biologic agents, 32.6% with conventional systemic treatments, and 11% with phototherapy.
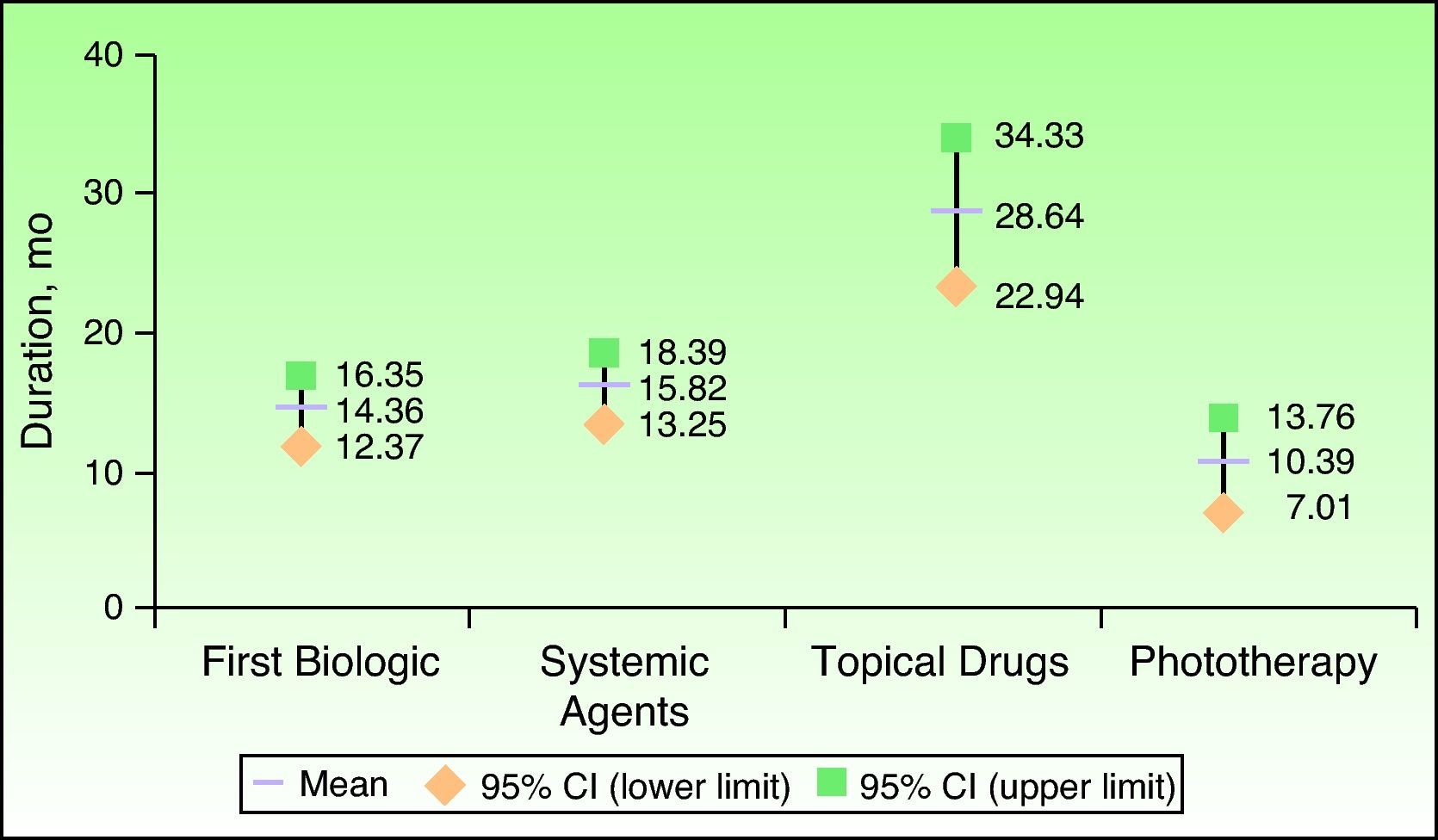
ConclusionsSeverity of psoriasis was associated with a marked impact on quality of life. Regardless of disease severity, psychiatric comorbidity was the strongest predictor of poor quality of life. On average, patients had received other treatments, such as conventional systemic treatments or phototherapy, for more than 2 years before switching to biologic agents for the first time.
La evaluación de la gravedad de la psoriasis se considera esencial en el manejo terapéutico óptimo de los pacientes.
ObjetivosDescripción de las características clínicas y perfil terapéutico de los pacientes con psoriasis moderada a grave en el ámbito español, evaluando su impacto en la calidad de vida de los pacientes.
Material y métodosEstudio observacional, de corte transversal, realizado en 90 unidades dermatológicas en España en 2009. Se incluyeron 442 pacientes diagnosticados de psoriasis moderada a grave que habían iniciado tratamiento con fármacos sistémicos, fototerapia y/o tratamientos tópicos entre 2004 y 2006.
ResultadosLos pacientes con psoriasis más grave presentaron de forma significativa un mayor tiempo de evolución de la enfermedad, mayor prevalencia de enfermedades concomitantes y mayor afectación ungueal, del cuero cabelludo, de las flexuras y de la zona palmo-plantar, así como peor calidad de vida. Durante los 5 años previos al inicio del estudio el 68% de los pacientes recibieron tratamientos sistémicos convencionales, el 39,1% fármacos biológicos y el 22,3% fototerapia. En la actualidad el 57,5% estaban siendo tratados con algún fármaco biológico, el 32,6% recibían fármacos sistémicos convencionales y el 11% fototerapia.
ConclusionesLa gravedad de la psoriasis se asoció en nuestro estudio con una marcada afectación de la calidad de vida. Independientemente de la gravedad de la psoriasis, el mayor predictor de mala calidad de vida fue la comorbilidad psiquiátrica. El tiempo medio de permanencia en otros tratamientos, incluyendo sistémicos convencionales o fototerapia, hasta el cambio a un primer biológico fue superior a los 2 años.
Psoriasis is a chronic inflammatory skin disorder of unknown etiology, although it is thought to be caused by the interaction of multiple genes, the immune system, and certain environmental factors.1 It affects approximately 2% of the world's population, with a similar prevalence in men and women.2 In Spain the estimated prevalence in the general population is between 1.17% and 1.43%, with onset usually occurring in individuals aged between 20 and 50 years.3
Psoriasis has a considerable impact on patients’ lives and affects physical health, psychological state, social relationships, and work.4,5 The disorder is frequently associated with a range of comorbidities, including inflammatory bowel disease, heart disease, and obesity, thus complicating management and negatively impacting mental and emotional health.6 Psoriasis has been reported to have a similar or even greater effect on quality of life than other chronic diseases such as ischemic heart disease or diabetes mellitus.7–9 Quality of life in psoriasis has been reported to be directly related to disease severity7,10 and appears to be influenced, to varying degrees, by a wide range of physical and psychosocial factors.7,9
Given the chronic nature of psoriasis, patients often require long-term treatment, which varies according to multiple factors such as the extent and severity of disease and the presence of psoriatic arthritis or other comorbidities.11 Conventional treatment can be very effective in the short term, but cumulative toxicity is often a problem in the long-term management of psoriasis.12 New biologic agents that act more selectively on key inflammatory components are now considered a therapeutic alternative in this disorder.13
In view of the scant information available on the management of psoriasis in routine clinical practice in Spain, we designed a study to describe the clinical characteristics and treatment of patients with moderate to severe psoriasis in Spain and to assess the impact of the disease on their quality of life.
Material and MethodsWe performed a multicenter, epidemiological, observational, cross-sectional study in which the investigators were dermatology specialists treating patients with psoriasis at hospitals, specialist centers, or private offices. The patients were enrolled consecutively during scheduled visits. All the data required for the study were collected during a single visit, which coincided with enrolment.
The inclusion criteria were an age of 18 years or older and a diagnosis of moderate or severe psoriasis, defined as a Psoriasis Area and Severity Index (PASI) score of 10 or higher and/or a body surface area affected by psoriasis (BSA) of 10% or more. Those enrolled were also required to have started treatment with systemic drugs, phototherapy, and/or topical treatment between 2004 and 2006. Written informed consent was obtained from all patients prior to inclusion and confidentiality of data was guaranteed. The study was approved by the clinical research ethics committee at Hospital Nuestra Señora de Sonsoles in Ávila. Patients were recruited from 90 centers between March and November, 2009. Following enrolment at a scheduled visit, each patient was interviewed and his or her medical record reviewed, with collection of sociodemographic and clinical data, including general clinical information, clinical characteristics specific to psoriasis, and information regarding treatment. Disease severity was also assessed (BSA or PASI) at this visit, as was quality of life using the patient-assessed Dermatology Life Quality Index (DLQI).14 A score of 5 or less on the DLQI was considered to indicate good or satisfactory quality of life while one of 6 or higher was considered to indicate poor or unsatisfactory quality of life.
Statistical AnalysisThe data for all evaluable patients were analyzed. Qualitative variables were described as absolute and relative frequencies while quantitative variables were described using means (SD) and CIs when they were normally distributed, or medians (range and interquartile range [IQR]) when they were not. This analysis was performed for the sample as a whole and for subgroups of patients classified according to disease severity (moderate or severe) and quality of life (good/satisfactory or poor/unsatisfactory). To analyze statistically significant differences between independent quantitative variables, we used the t test for parametric variables and the Mann-Whitney U test for nonparametric variables. The Pearson χ2 test for 2×2 contingency tables and the likelihood ratio test for m×n contingency tables were used for qualitative variables. To investigate factors potentially associated with quality of life, we performed multivariate logistic regression analysis, where the dependent variable was quality of life according to the DLQI (good or poor) and the independent variables were factors identified as significant in the univariate analysis. Estimates were expressed with a confidence level of 95%. SPSS version 17.0 was used for all analyses.
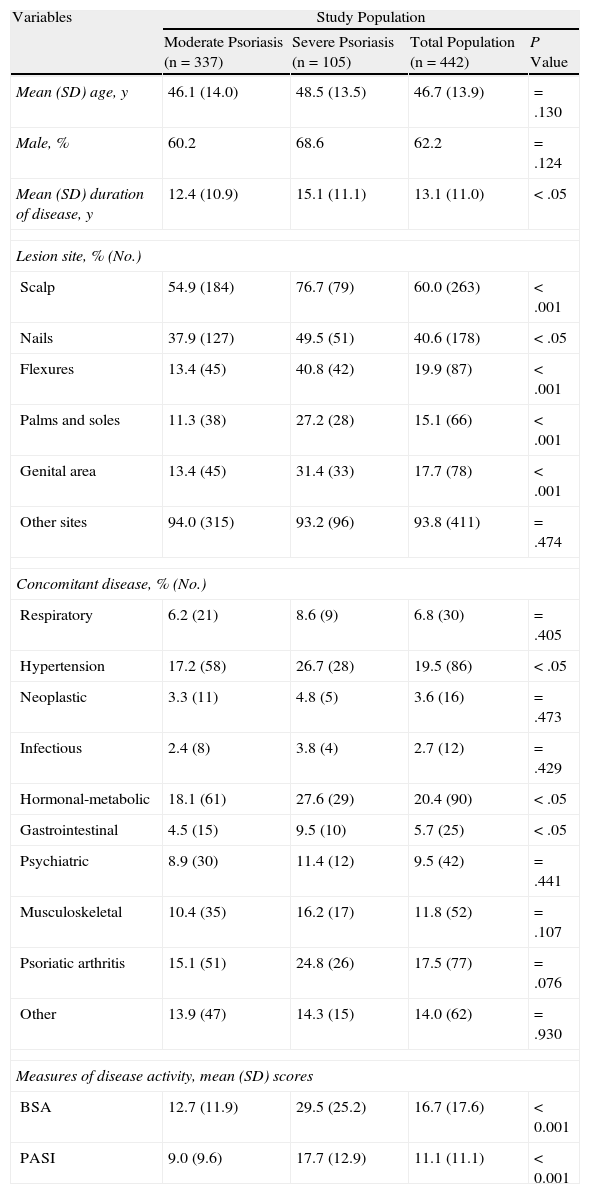
ResultsDemographic and Clinical VariablesA total of 442 evaluable patients were included in the study. The mean (SD) age was 46.7 (13.9) years and 62.2% of the group (n=275) were men. At the time of inclusion, 76.2% of the patients (n=337) had moderate psoriasis while 23.8% (n=105) had severe psoriasis. The mean BSA and PASI scores were, respectively, 12.7(11.9) and 9.0 (9.6) for those with moderate disease and 29.5(25.2) and 17.7(12.9) for those with severe disease (P<.001 in both cases). A family history of psoriasis was reported in 51% of patients (214/420) but no significant differences were detected between those with moderate and severe disease (P=.076). Duration of disease, calculated as the number of years from the time of diagnosis to inclusion of the patient in the study, was significantly longer in the severe disease group (15.1[11.1] years; 95% CI, 13.0-17.3) than in the moderate disease group (12.4 [10.9] years; 95% CI, 11.2-13.6) (P<.05). Of the patients with severe psoriasis, 7.6% were on sick leave; the corresponding proportion in the moderate psoriasis group was significantly lower at 2.4% (P<.05). The prevalence of concomitant conditions, such as hypertension, hormonal or metabolic disorders, and gastrointestinal disorders, was significantly higher in patients with severe disease (26.7%, n=28; 27.6%, n=29; and 9.5%, n=10, respectively) than in those with moderate disease (17.2%, n=58; 18.1%, n=61; and 4.5%, n=15, respectively) (P<.05 in all cases) The percentage of patients who consumed alcohol was higher in the moderate psoriasis group (13.8% vs 9.8% in the severe psoriasis group) but mean consumption was lower (19.6 [23.6] g/d vs 28.6 [30.6g/d]), although the differences were not significant (P=.398). Approximately 30% of the sample were smokers, but the differences between those with moderate and severe disease were not significant (P=.567). The main sociodemographic and clinical characteristics at inclusion in the study are summarized in Table 1.
Sociodemographic and Clinical Characteristics of Patients.
| Variables | Study Population | |||
| Moderate Psoriasis (n=337) | Severe Psoriasis (n=105) | Total Population (n=442) | P Value | |
| Mean (SD) age, y | 46.1 (14.0) | 48.5 (13.5) | 46.7 (13.9) | =.130 |
| Male, % | 60.2 | 68.6 | 62.2 | =.124 |
| Mean (SD) duration of disease, y | 12.4 (10.9) | 15.1 (11.1) | 13.1 (11.0) | <.05 |
| Lesion site, % (No.) | ||||
| Scalp | 54.9 (184) | 76.7 (79) | 60.0 (263) | <.001 |
| Nails | 37.9 (127) | 49.5 (51) | 40.6 (178) | <.05 |
| Flexures | 13.4 (45) | 40.8 (42) | 19.9 (87) | <.001 |
| Palms and soles | 11.3 (38) | 27.2 (28) | 15.1 (66) | <.001 |
| Genital area | 13.4 (45) | 31.4 (33) | 17.7 (78) | <.001 |
| Other sites | 94.0 (315) | 93.2 (96) | 93.8 (411) | =.474 |
| Concomitant disease, % (No.) | ||||
| Respiratory | 6.2 (21) | 8.6 (9) | 6.8 (30) | =.405 |
| Hypertension | 17.2 (58) | 26.7 (28) | 19.5 (86) | <.05 |
| Neoplastic | 3.3 (11) | 4.8 (5) | 3.6 (16) | =.473 |
| Infectious | 2.4 (8) | 3.8 (4) | 2.7 (12) | =.429 |
| Hormonal-metabolic | 18.1 (61) | 27.6 (29) | 20.4 (90) | <.05 |
| Gastrointestinal | 4.5 (15) | 9.5 (10) | 5.7 (25) | <.05 |
| Psychiatric | 8.9 (30) | 11.4 (12) | 9.5 (42) | =.441 |
| Musculoskeletal | 10.4 (35) | 16.2 (17) | 11.8 (52) | =.107 |
| Psoriatic arthritis | 15.1 (51) | 24.8 (26) | 17.5 (77) | =.076 |
| Other | 13.9 (47) | 14.3 (15) | 14.0 (62) | =.930 |
| Measures of disease activity, mean (SD) scores | ||||
| BSA | 12.7 (11.9) | 29.5 (25.2) | 16.7 (17.6) | <0.001 |
| PASI | 9.0 (9.6) | 17.7 (12.9) | 11.1 (11.1) | <0.001 |
Abbreviations: BSA, body surface area affected by psoriasis; PASI, Psoriasis Area and Severity Index.
Those with severe psoriasis had greater skin involvement, nail involvement, and joint symptoms. Specifically, 82.9% (87/105) had skin lesions with marked scaling, 61% (64/105) had nail alterations, and 34.3% (36/105) had joint pain. In the moderate disease group, 54.5% (183/336) had marked scaling, 39.6% (133/336) had nail alterations, and 24.7% (83/336) had joint pain. The differences were statistically significant for the presence of marked scaling and nail involvement (P<.001 in both cases). Patients with severe psoriasis also had greater skin involvement in the following areas: scalp, flexures, palms and soles, and genital area (P<.001 in all cases). In total, 17.5% of the group (77/441) had a diagnosis of psoriatic arthritis at inclusion in the study, but no significant differences in prevalence were detected between those with severe disease (24.6%) and those with moderate disease (15.1%) (P=.076).
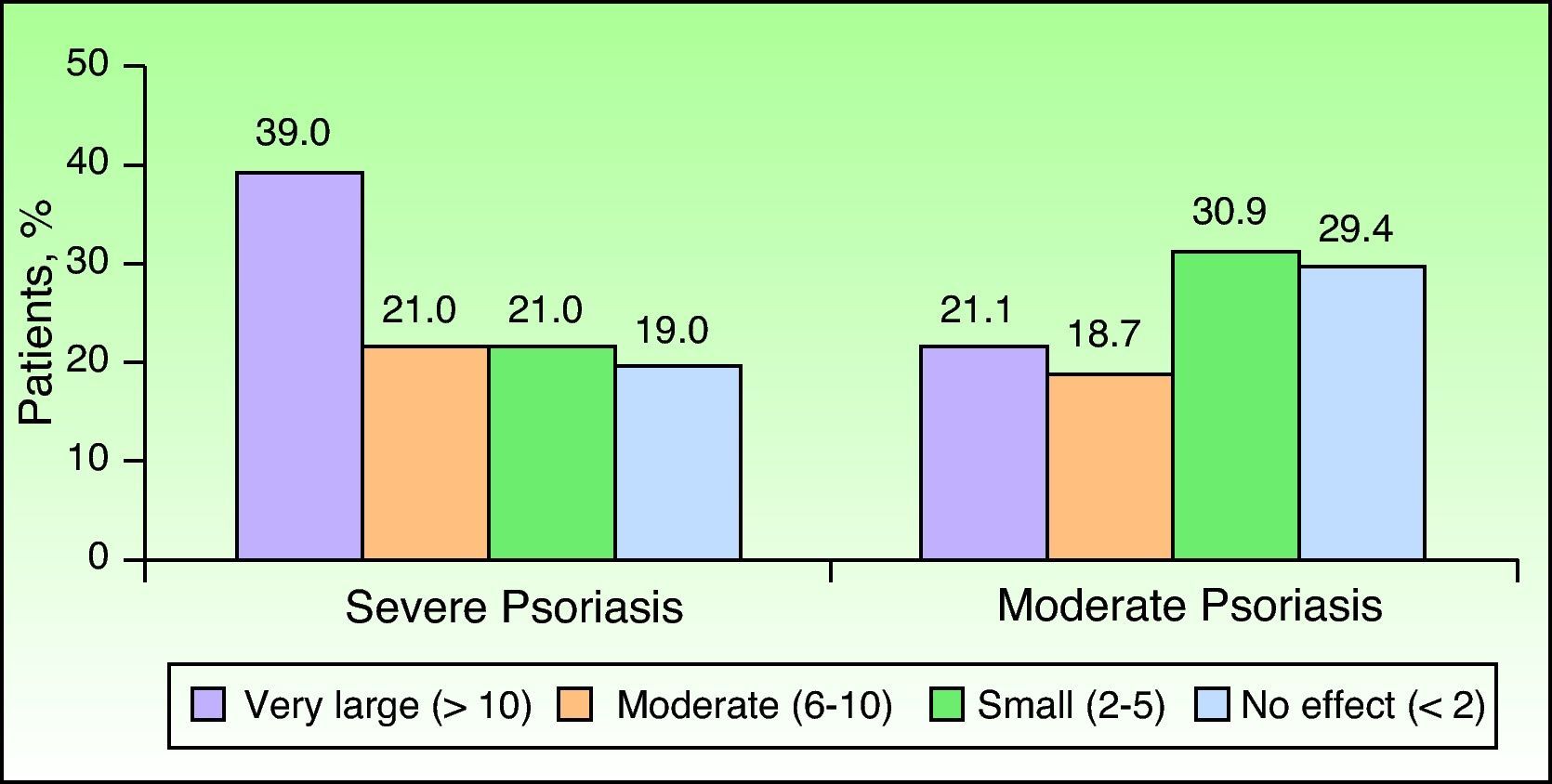
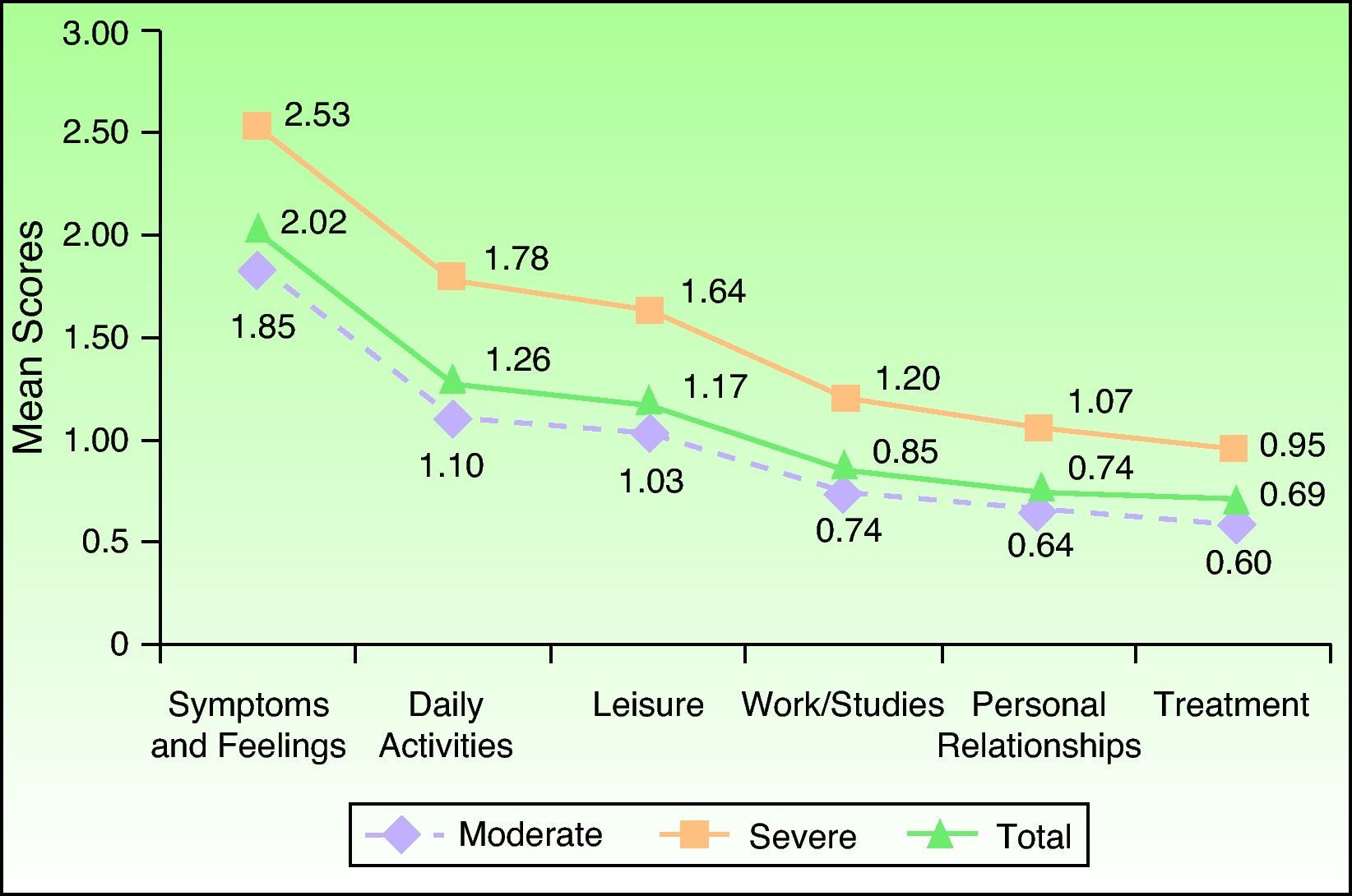
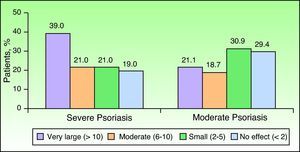
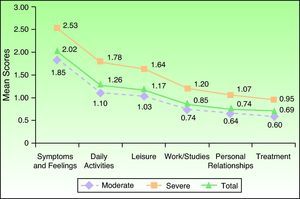
Quality of Life VariablesThe mean DLQI score for the whole group was 6.7 (6.6), with those with severe psoriasis scoring significantly higher (9.2 [7.8]) (worse quality of life) than those with moderate psoriasis (5.9 [6.0]) (P<.001) (Fig. 1). Patients with severe psoriasis also had a significantly higher score in the 6 domains of the DLQI: symptoms and feelings, daily activities, leisure, work/school, personal relationships, and treatment (P<.01 for personal relationships and P<.001 for the rest) (Fig. 2). Sixty percent (63/105) of those with severe disease and 39.8% (134/337) of those with moderate psoriasis had a poor or unsatisfactory quality of life (P<.001).
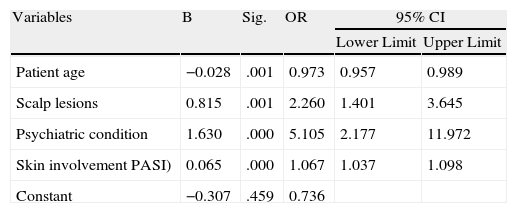
Regardless of psoriasis severity, those with a better quality of life according to the DLQI were significantly older (48.0 [13.9] vs 44.9 [13.8] years, P<.05) and had longer disease duration (14.1 [11.8] vs 11.8 [9.7] years, P<.05) than those with a worse quality of life. Poor quality of life was significantly associated with greater involvement of the scalp (74.1% vs 48.5%) (P<.001), nails (48.7% vs 34.0%) (P<.001), genital area (24.9% vs 11.9%) (P<.001), and flexures (25.9% vs 14.9%) (P<.01), and a higher prevalence of psychiatric comorbidity (15.7% vs 4.5%) (P<.001). Regression analysis of factors significantly associated with quality of life showed that age was a protective factor (odds ratio [OR], 0.973; 95% CI, 0.957-0.989), while scalp involvement (OR, 2.260; 95% CI, 1.401-3.645), psychiatric comorbidity (OR, 5.105; 95% CI, 2.177-11.972), and higher PASI score (OR, 1.067; 95% CI, 1.037-1.098) were associated with a higher odds of low quality of life (Table 2).
Regression Analysis for Factors That Impact Quality of Life in Patients With Moderate to Severe Psoriasis.
| Variables | B | Sig. | OR | 95% CI | |
| Lower Limit | Upper Limit | ||||
| Patient age | −0.028 | .001 | 0.973 | 0.957 | 0.989 |
| Scalp lesions | 0.815 | .001 | 2.260 | 1.401 | 3.645 |
| Psychiatric condition | 1.630 | .000 | 5.105 | 2.177 | 11.972 |
| Skin involvement PASI) | 0.065 | .000 | 1.067 | 1.037 | 1.098 |
| Constant | −0.307 | .459 | 0.736 | ||
Abbreviations: OR, odds ratio; PASI, Psoriasis Area and Severity Index.
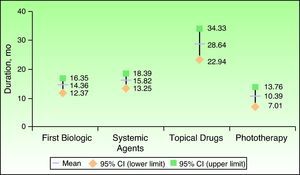
All of the patients enrolled in this study had started systemic treatment, phototherapy, and/or topical treatment for their psoriasis between 2004 and 2006. In the 5 years before the start of the study, 68% had received conventional systemic agents, 64.1% topical treatments, 39.1% biologic agents, 22.3% phototherapy, and 24.6% (n=107) another type of treatment (Fig. 3). The mean duration of treatment was 28.6(37.6) months (95% CI, 22.9-34.3) for topical treatments, 15.8(20.8) months (95% CI, 13.2-18.4) for conventional systemic treatment, 10.4(15.9) months (95% CI, 7.0-13.8) for phototherapy, and 14.4(12.6) months (95% CI. 12.3-16.3) for the first biologic agent received (Fig. 4). The mean time from the start of systemic treatment or phototherapy to administration of the first biologic agent was 28.0 (49.3) months (95% CI, 23.4-33.5). The first biologic agent used in over 90% of the patients was efalizumab or etanercept. The specific percentages were 48.8% (n=83) for efalizumab, 45.3% (n=77) for etanercept, 3.5% (n=6) for adalimumab, and 2.4% (n=4) for infliximab. The mean duration of treatment was 15.6(13.3) months in the case of efalizumab, 13.8(12.1) months in the case of etanercept, 5.5(3.6) months in the case of adalimumab, and 6.6(4.3) months in the case of infliximab. In total, 77.6% (n=132) of the patients who had been treated with a biologic agent before the start of the study did not need to be switched to another biologic agent. Of the 38 patients who did, 73.7% (n=28) switched just once, while 26.3% (n=10) switched twice. All but 4 (0.9%) were being treated for their psoriasis at the study inclusion visit: 57.5% (252/438) were receiving a biologic agent (55.3% [184/438] of those with moderate psoriasis and 64.8% [68/438] of those with severe psoriasis), 32.6% (143/438) were receiving conventional systemic treatment, 11.0% (48/438) were receiving phototherapy, 27.2% (119/438) were receiving concomitant topical treatment; and 10.3% (45/438) were receiving other drugs (Fig. 5).
The findings of the present study highlight the considerable impact that psoriasis has on patient quality of life, the importance of determining disease severity before initiating treatment, and the need for a multidimensional approach to management, as has been mentioned by other authors.15 All the patients in our study had moderate to severe plaque psoriasis, diagnosed according to clinical criteria based on BSA and PASI scores, and they had all started specific psoriasis treatment with systemic agents, phototherapy, and/or topical drugs between 2004 and 2006. The characteristics of our patients are similar to those described in other epidemiological studies of moderate to severe plaque psoriasis in Europe.15–17 In our series, most of the patients had moderate disease (76.2%), there was a predominance of male patients (62.2%), and the mean duration of disease was 13 years. As was to be expected, there was a high prevalence of concomitant disease, and 17.5% of the patients had associated arthritic psoriasis.
Severe psoriasis (present in 23.8% [n=105] of our patients) was significantly associated with longer disease duration and a higher prevalence of concomitant disease, nail alterations, and lesions with marked scaling. The areas most significantly affected were the scalp, flexures, palms and soles, and the genital area. While psoriatic arthritis appears to be more common in patients with more extensive disease,18 it can also run an aggressive course in patients with less severe psoriasis.19 Like other authors,17,20 we did not detect any differences in the prevalence of psoriatic arthritis according to disease severity. We also did not observe any significant differences in the prevalence of severe disease in men compared to women or detect a relationship with smoking, contrasting with reports from an earlier epidemiological study published in Spain.17
Psoriasis is significantly associated with a variety of physical and psychological dimensions that affect patient quality of life, hence the consideration that dermatologists need to manage this disorder from a multidimensional approach.7,9,10,20,21 A recent study of psoriasis patients in hospital and outpatients settings in Spain reported that the disease had a considerable impact on quality of life, particularly with regard to emotional status.21 In our study, 60% of patients with severe psoriasis but just 39.8% of those with moderate disease had a poor or unsatisfactory quality of life; furthermore, in those with severe disease, all 6 domains of the DLQI were significantly affected. Regardless of disease severity, we observed a significant association between poor quality of life and the presence of concomitant psychiatric conditions and greater scalp involvement. Age, by contrast, was a protective factor. Psychiatric morbidity was the strongest predictor of poor quality of life in our patients, with an OR of 5.105, contrasting with PASI score, which was the weakest predictor, with an OR of 1.067. This finding is consistent with those of previous studies.7,15 Our findings with regard to age are consistent with those reported in a systemic review of quality of life in psoriasis in that higher age was correlated with a better quality of life.7 In agreement with other reports,20 we did not detect significant differences in quality of life between patients with psoriasis and psoriatic arthritis and those with psoriasis alone.
In an epidemiological study of severe psoriasis in Spain and Portugal conducted between 2004 and 2005, approximately only half of the patients surveyed were receiving conventional systemic treatment.17 The authors, like others,15 concluded that psoriasis was inadequately treated in many of these patients. One of the most relevant aspects of the present study is that we analyzed the prescribing habits of Spanish dermatologists in a retrospective analysis of up to 5 years (2004-2009). During this period, 68% of the patients in our series had been treated with conventional systemic agents, 39.1% with biologic therapy, 22.3% with phototherapy, and 64.1% with concomitant topical drugs. The mean duration of treatment was approximately 2 years for topical treatment, approximately a year and a half for conventional systemic agents and the first biologic agent received, and less than a year for phototherapy. Although all the patients in our study had moderate to severe psoriasis, just 39.1% had received biologics during this period; this is probably related to the gradual introduction of biologic drugs starting in 2005, which is when efalizumab, infliximab, and etanercept were marketed for the first time. When enrolled in the study in 2009, 57.5% of the patients were on biologic agents, indicating an increasing tendency to use these drugs in moderate to severe psoriasis. Nevertheless, considering the centers that were selected to participate in the study, it should be noted that this figure may possibly be higher than the average for Spain.
Despite the availability of international guidelines on the treatment of psoriasis,22,23 which include recommendations on the use of conventional systemic agents, and despite the fact that these drugs have known beneficial effects, questions remain about the optimal use of these drugs.11,15 Current guidelines, for example, do not recommend how long systemic drugs should be ideally administered before switching to biologics in those cases where it is necessary. In our series, the mean duration of treatment, including conventional systemic treatment and phototherapy, before a switch to the first biologic agent, was over 2 years, providing new data on the therapeutic management of psoriasis in Spanish clinics. New guidelines with recommendations on how long patients should receive systemic treatment before switching to biologic agents would certainly help to improve the management of psoriasis.
When interpreting the findings of the present study and extrapolating them to a national level or drawing comparisons with populations with similar characteristics, it is important to note that certain biases may have been introduced, mostly related to the retrospective design of the study and the selection of participating centers. Nonetheless, the observational nature of the study is its main strength as it allowed us to provide a descriptive analysis of the clinical characteristics and treatment profile of patients with moderate to severe psoriasis in routine clinical practice in Spain.
To conclude, based on our findings, severe psoriasis is significantly associated with longer disease duration; a higher prevalence of comorbidity, nail alterations, and lesions with marked scaling; greater involvement of the scalp, flexures, palms and soles, and genital area; and considerably impaired quality of life. The strongest predictor of poor or unsatisfactory quality of life was the presence of psychiatric comorbidity, regardless of disease severity. The mean duration of treatment, including conventional systemic treatment and phototherapy, before switching to the first biologic agent, was over 2 years.
Conflicts of InterestDr José Manuel Hernánz, Dr Manuel Sánchez-Regaña, and Dr Rosa Izu participated in clinical trials sponsored by Pfizer Spain and received consultancy and speakers’ fees for activities sponsored by Pfizer Spain.
Dr Victoria Mendiola has participated in clinical trials sponsored by Pfizer Spain.
Dr Carmen García-Calvo works in the Medical Department of Pfizer, S.L.
FundingThis study was financed by Pfizer Spain. The authors did not receive fees for contributing to the writing or publication of this manuscript.
Publishing support was provided by UBC Scientific Solutions and financed by Pfizer Spain.
Please cite this article as: Hernánz JM, et al. Evaluación clínica y terapéutica de los pacientes con psoriasis moderada o grave en España. Estudio Secuence. Actas Dermosifiliogr. 2012;103:897–904.