A 56-year-old man with no relevant past history presented with mildly pruritic lesions on the dorsal aspect of both forearms that had first appeared 8 months earlier. The patient reported no history of applying products to the affected area and mentioned no possible triggers.
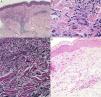
Physical ExaminationPhysical examination revealed large erythematous plaques with slightly raised borders and a central depression affecting the dorsal aspect of both forearms and hands. The lesions had an annular morphology and, interestingly, spared the area covered by the watch on the left wrist (Fig. 1).
Epicutaneous tests from the standard series of the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC) and standard photopatch tests were negative.
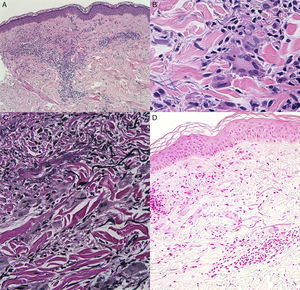
HistopathologyHistologic examination of a punch biopsy specimen taken from the border of one of the plaques revealed an epidermis without significant alterations. A superficial granulomatous and perivascular infiltrate composed of mononuclear cells and multinucleated giant cells was observed in the upper and mid dermis. The cytoplasm of these cells contained numerous fragmented elastic fibers rendered more visible by Verhoeff-Van Gieson staining. Neither collagen degeneration nor the presence of mucin were observed (Fig. 2).
What Is Your Diagnosis?
DiagnosisAnnular elastolytic giant cell granuloma (actinic granuloma).
Clinical Course and TreatmentTreatment was started with medium-strength topical corticosteroids and sun protection. Partial improvement of the lesions was observed after 3 months of application.
CommentAnnular elastolytic giant cell granuloma (AEGCG), also known as actinic granuloma or O’Brien granuloma, is a rare granulomatous disease characterized by the presence of multinucleated giant cells with phagocytosis of anomalous elastic fibers, a process known as elastophagocytosis. AEGCG mainly affects women aged 50 to 70 years with a light skin phototype and signs of chronic actinic damage. The lesions usually begin as erythematous papules that later evolve into annular plaques with raised borders and a minimal atrophic center. The most common sites are sun-exposed areas such as the face, upper chest, and legs.1
The pathogenesis of this entity is unknown, although the possibility of an autoimmune reaction directed against elastic fibers, determining a granulomatous inflammatory response with the formation of granulomas, has been postulated.2 AEGCG has been described in association with various processes, including diabetes mellitus, medication use, hypothyroidism, thyroiditis, lymphomas, polymyalgia rheumatica, and temporal arteritis.
At present, it is not known whether there is a relationship between AEGCG and these processes.
Histopathology shows 3 well-defined zones that reflect this possible pathogenesis. A peripheral zone, outside the borders of the plaques, is characterized by a papillary dermis with actinic elastosis, without the presence of multinucleated giant cells or granulomas. This zone, in which the lesion progresses, contains antigenic elastic fibers that have not yet induced an inflammatory reaction. In an intermediate or active zone—corresponding clinically to the edge of the lesions—fragmented elastic fibers, elastophagocytosis phenomena, and granuloma formation are observed. Finally, a central zone, characterized by the absence of elastic fibers and few inflammatory cells, is the residual postinflammatory zone.3
The main differential diagnosis is granuloma annulare (GA) at sun-exposed sites. In fact, since AEGCG was first described, there has been some debate about whether it is a distinct entity or a variant of GA with elastophagocytosis.4 Although these two processes can be clinically identical, histologic studies support the idea that they are separate entities. In AEGCG, the granulomatous reaction is found mainly in the upper dermis and no mucin is observed, whereas in GA, granulomas are distributed throughout the upper and mid dermis, forming a palisade around an area characterized by degenerated collagen and the presence of mucin.5
Although spontaneous remission has been reported in some cases, AEGCG tends to be chronic and recurring. Multiple treatment options have been described, including sun protection; topical, systemic, or intralesional corticosteroids; chloroquine; dapsone; methotrexate; anti–tumor necrosis factor (TNF) monoclonal antibodies; and low-dose oral retinoids. These treatments have produced variable results.6–8
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rozas-Muñoz E, Mir-Bonafé JF, Serra-Baldrich E. Placas anulares bilaterales en manos y antebrazos. Actas Dermosifiliogr. 2018;109:263–264.