Herpesvirus infections are not uncommon in hematologic patients. Our first patient, diagnosed with chronic lymphatic leukemia, presented extensive genital herpes infection refractory to treatment with aciclovir and with a partial response to foscarnet, which had to be withdrawn due to systemic adverse effects. The second patient, diagnosed with follicular Hodgkin lymphoma, presented hypertrophic herpes infection refractory to treatment with aciclovir but that responded to intralesional cidofovir and topical imiquimod. As in other immunocompromised patients, herpesvirus infection in hematologic patients can present atypical manifestations, as well as resistance to treatments that are activated by the viral thymidine kinase. A high level of clinical suspicion is therefore needed to make an early diagnosis, together with extensive knowledge of the different treatments available.
Las infecciones por virus herpes presentan una frecuencia no desdeñable en pacientes hematológicos. El primer caso corresponde a una paciente con leucemia linfática crónica con un herpes genital extenso refractario a aciclovir, con respuesta parcial a foscarnet que hubo que suspender por efectos secundarios sistémicos. El segundo caso es el de una paciente con un linfoma de Hodgkin folicular que presentaba un herpes hipertrófico refractario a tratamiento con aciclovir, que respondió a cidofovir intralesional e imiquimod tópico. Los pacientes hematológicos, al igual que otros enfermos inmunodeprimidos, pueden presentar manifestaciones atípicas de infección por virus herpes, así como resistencia a los tratamientos que actúan por medio de la timidina quinasa viral. Esto hace necesario tener una alta sospecha clínica para poder alcanzar un diagnóstico precoz, y conocer los diferentes tratamientos alternativos disponibles.
Infections by viruses in the Herpesviridae family are highly common in patients with hematologic diseases. Most of the infections seen in routine clinical practice are caused by viruses in the Alphaherpesvirinae subfamily, which includes herpes simplex virus (HSV) types 1 or 2 and the varicella zoster virus. Both the diagnosis and treatment of these infections are challenging because atypical presentations are common, as is resistance to the usual drugs (aciclovir, valaciclovir, and famciclovir). We report 2 cases of drug-resistant HSV-2 infection with unusual presentations in patients with hematologic diseases.
Case 1An 84-year-old woman with a history of arterial hypertension, type 2 diabetes mellitus, high cholesterol levels, and chronic lymphocytic leukemia was being followed but was not currently under treatment for the leukemia. She had received intravenous (iv) aciclovir for perianal and vulvar ulcers secondary to HSV-2 infection in 2015 and showed partial response. In March 2017 she was admitted with a new flare-up of the lesions. Physical examination revealed a wide area of ulceration with a fibrinous center, a foul-smelling exudate and erythematous borders distributed on the vulva, perianal area, and groin as well as over the lower abdomen and on the internal surfaces of the thighs (Fig. 1). A polymerase chain reaction (PCR) test was positive for HSV-2, and she was started on treatment with iv aciclovir, 10mg/kg every 8hours, and 1%cidofovir cream once daily. After 10days with no improvement, and given evidence of severe hypogammaglobulinemia, we infused a 0.4g/kg dose of immunoglobulins, leaving the other treatments unchanged. The ulcers worsened, suggesting the likelihood of resistance to aciclovir. She was switched to iv foscarnet, 40mg/kg every 8hours, and 5%imiquimod cream thrice weekly. The skin lesions began to improve gradually, but her general condition remained poor, with multiple complications related to foscarnet (low calcium, magnesium, phosphate, and potassium levels refractory to oral and intravenous supplements). She also suffered 2urinary tract infections (one due to Klebsiella pneumoniae and the other to Enterococcus faecium) that resolved with antibiotic treatment. Renal function declined gradually and she experienced several episodes of exacerbated heart failure. It was decided to suspend intensive treatment for the HSV-2 infection and discharge her under treatment with 5%imiquimod cream and oral valaciclovir. Three months later, the patient was brought to the emergency department, where she died due to sepsis arising from a urinary tract infection.
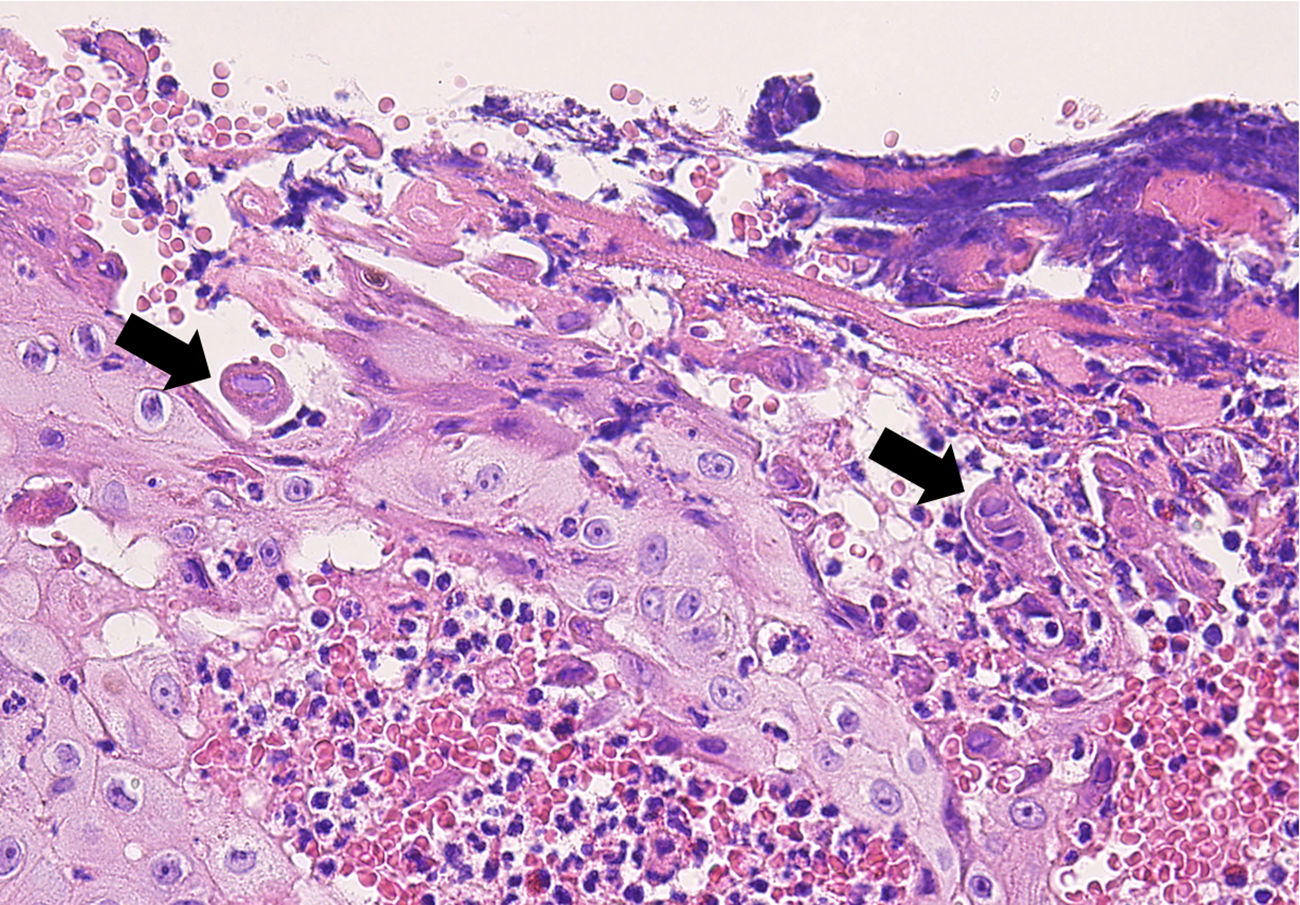
Case 2A 64-year-old woman with a history of follicular Hodgkin lymphoma treated with a bone marrow transplant had also had a prior HSV-2 infection. She complained of an exophytic perianal lesion (Fig. 2A). A biopsy to rule out perianal epidermoid carcinoma showed epidermal hyperplasia with multinucleated giant cells and epithelial cells with gray nuclei and marginal chromatin, consistent with herpesvirus infection (Fig. 3). A PCR test was positive for HSV-2, confirming a diagnosis of hypertrophic perianal herpes infection. She did not improve in 7days on oral aciclovir (400mg/4h), but the growth resolved completely after an intralesional injection of cidofovir (0.3mL) (Fig. 2B). Recurrences were frequent, however, so she was prescribed applications of 5%imiquimod cream 3 times per week. Response was favorable and remained stable 3months after applications began.
Herpesvirus infections are highly frequent in patients with hematologic diseases. The incidence varies from 15% in patients with chronic lymphocytic leukemia to 90% in patients with acute leukemia or those who have received a bone marrow transplant.1 The clinical signs, which arise when a latent virus is reactivated, may take the form of ulcers in the mouth (85%–90%) or genital area (10%–15%); primary infections are unusual in this context.2
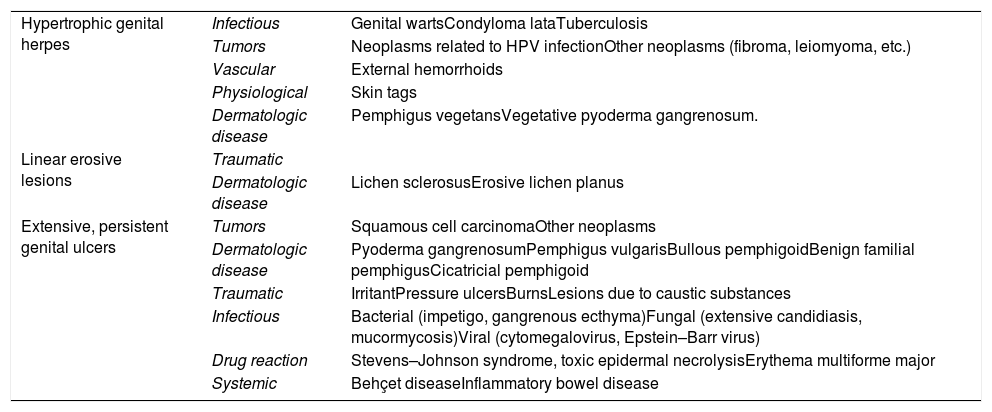
HSV-2 infections may present with chronic or atypical lesions in association with hematologic diseases3 and clinical manifestations vary. Among them are generalized papular rashes, large ulcerations with geographic borders, linear erosive lesions, and vegetative herpes.4 Lesions that progress like warts and can simulate neoplasia or lesions with necrotic plaques have also been reported.5 Thus, a differential diagnosis requires consideration of multiple possibilities (Table 1).
Differential Diagnosis of HSV-2 Infections With Atypical Presentations
| Hypertrophic genital herpes | Infectious | Genital wartsCondyloma lataTuberculosis |
| Tumors | Neoplasms related to HPV infectionOther neoplasms (fibroma, leiomyoma, etc.) | |
| Vascular | External hemorrhoids | |
| Physiological | Skin tags | |
| Dermatologic disease | Pemphigus vegetansVegetative pyoderma gangrenosum. | |
| Linear erosive lesions | Traumatic | |
| Dermatologic disease | Lichen sclerosusErosive lichen planus | |
| Extensive, persistent genital ulcers | Tumors | Squamous cell carcinomaOther neoplasms |
| Dermatologic disease | Pyoderma gangrenosumPemphigus vulgarisBullous pemphigoidBenign familial pemphigusCicatricial pemphigoid | |
| Traumatic | IrritantPressure ulcersBurnsLesions due to caustic substances | |
| Infectious | Bacterial (impetigo, gangrenous ecthyma)Fungal (extensive candidiasis, mucormycosis)Viral (cytomegalovirus, Epstein–Barr virus) | |
| Drug reaction | Stevens–Johnson syndrome, toxic epidermal necrolysisErythema multiforme major | |
| Systemic | Behçet diseaseInflammatory bowel disease |
Abbreviations: HPV, human papillomavirus; HSV-2, herpes simplex virus type 2.
Hypertrophic herpes simplex virus infections usually present as painful exophytic tumors that sometimes form ulcers on the surface, suggesting differential diagnoses of human papillomavirus infection, secondary syphilis, or cancer (epidermoid carcinoma or lymphoma).6 A biopsy usually shows a dense inflammatory infiltrate of plasma cells, lymphocytes and eosinophils, associated with variable degrees of epidermal hyperplasia with multinucleated giant cells that reveal the cytopathic effects of HSV infection (epithelial cells with gray nuclei and marginal chromatin).7 The mechanism underlying this hypertrophic variant is unknown, but one hypothesis is an abnormal immune response mediated by type 2 helper T-cells that trigger overproduction of keratinocytes and fibroblasts.6,8
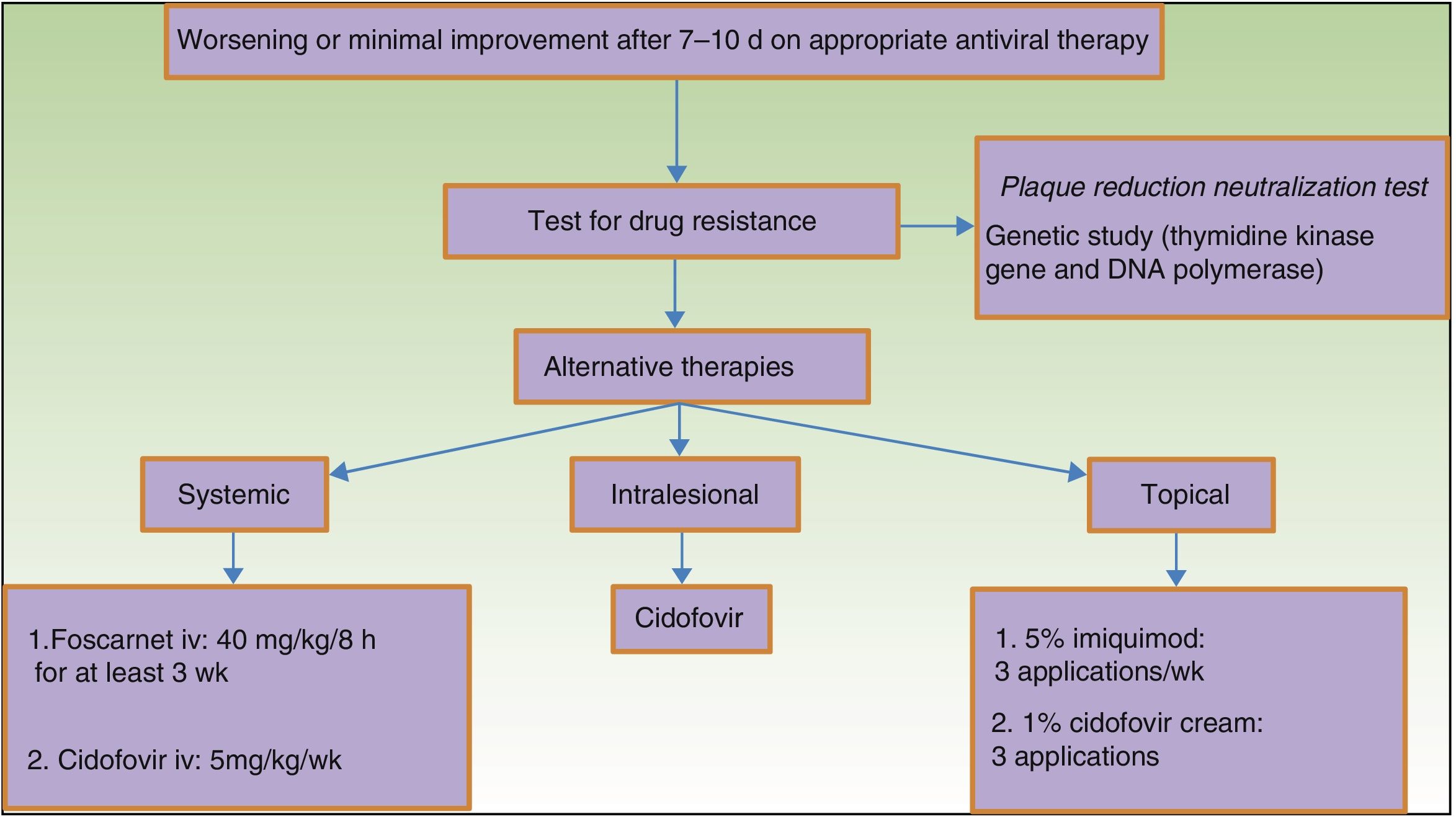
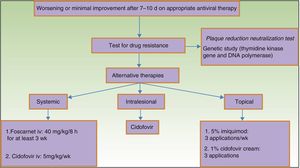
HSV resistance to aciclovir is unusual in immunocompetent individuals (<1%) but common in human immunodeficiency virus-infected individuals9 (5.3%) or those with hematologic diseases.2 Drug-resistant infections are fewer in patients who receive long-term prophylaxis after bone marrow transplants.10 However, if reactivation persists, resistance becomes more common. Responsible for resistance in 95% of cases is diminished activation of aciclovir in infected cells because of lower levels of viral thymidine kinase.2 All aciclovir-resistant strains are also resistant to valaciclovir and ganciclovir, and most are resistant to famciclovir. Intravenous foscarnet and iv or topical cidofovir offer alternatives in such cases because they are not activated by this enzyme. Phenotypic or genotypic HSV resistance to antiviral drugs can be detected with tests11 such as the analysis of genes encoding thymidine kinase and viral DNA polymerase.12 However, as such approaches are not available in most laboratories, clinicians rely on response to therapy to raise suspicion (Fig. 4).
Patients with hypertrophic herpes simplex virus infections have lesions that are often refractory to first-line drugs, suggesting that they are probably harboring resistant strains because less of the drug is reaching the lesion or less is deposited in pseudotumoral tissue.6 Imiquimod antagonizes Toll-like receptors, particularly Toll-like receptor 7, triggering the release of proinflammatory cytokines such as interferon-α, interleukin 6, or tumor necrosis factor. Using 5%imiquimod cream 3times per week has been reported to improve symptoms within a few weeks of application, causing few local side effects.6,13
In conclusion, immune suppression derived from hematologic diseases leads to a high incidence of viral, fungal, and bacterial skin lesions that often present atypically. Clinical suspicion should be high when treating these patients in the interest of early diagnosis and in order to consider all treatment alternatives, given that the viral strains involved are fairly often resistant to first-line drugs.
Ethical DisclosuresProtection of human and animal subjects.The authors declare that no experiments were performed on humans or animals during the course of this study.
Data confidentiality.The authors declare that they followed their hospitals’ regulations regarding the publication of patient information and that written informed consent for voluntary participation was obtained for all patients.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez DN, Cudós ES, Carnero JMR, Pinto PH. Presentación atípica de infección por virus de herpes simple tipo ii (VHS II) refractaria a tratamiento con aciclovir en 2 pacientes hematológicos. Actas Dermosifiliogr. 2019;110:393–397.