Pityriasis versicolor (PV) is a common superficial fungal infection caused by yeasts of the genus Malassezia. In clinical terms, it generally presents on the trunk as round or oval macules that vary in color from hypopigmentation to blackish.1 Its symptoms are easily recognizable, with several atypical forms reported, including the variant with atrophic lesions.2
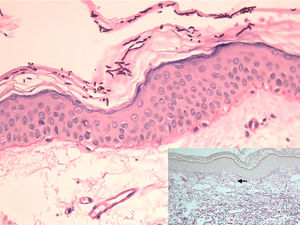
A 28-year-old man with plaque psoriasis treated with topical corticosteroids consulted for the appearance of cutaneous abnormalities that he perceived as being different from his psoriasis lesions. The physical examination revealed several circular areas on the back and the extensor surface of the upper right limb. The areas measured 0.5cm to 4cm and were depressed and atrophic in appearance (Fig. 1). Some were hypopigmented, whereas others were slightly pink; some had mild desquamation, whereas others were similar to typical psoriasis lesions (Fig. 2). The Wood lamp examination did not reveal fluorescence. The skin biopsy revealed laminated hyperkeratosis in the epidermis, with flattening of the rete ridges and an edematous appearance with vascular dilations in the dermis that was more evident in the papillary dermis. The vessels were surrounded by a discreet lymphocytic infiltrate. Periodic acid–Schiff staining revealed abundant short, septate hyphae and spores between the layers of keratin. Orcein staining revealed diminished elastic fibers in the papillary dermis and fragmentation thereof in the superficial reticular dermis (Fig. 3). Direct examination of the lesions revealed the presence of yeasts and pseudomycelium.
Epidermis with abundant hyphae and spores in the stratum corneum and flattening of the rete ridges (periodic acid–Schiff, original magnification ×200). The inset shows diminished fine elastic fibers in the papillary dermis (arrow) and fragmented elastic fibers in the superficial reticular dermis, as well as vascular ectasia (orcein stain, original magnification ×100).
The patient was prescribed itraconazole 200mg/d for 7 days combined with topical flutrimazole at night for 1 month. The topical corticosteroid was replaced by calcitriol ointment for treatment of his psoriasis. Although improvement was slow, the patient had fully recovered at 6 months, with no new lesions after 1 year of follow-up.
Atrophying or atrophic PV is an uncommon presentation of this condition.2–10 It manifests clinically as depressed erythematous or hypopigmented areas with discreet desquamation located mainly on the trunk, generally the back and shoulders. The lesions are usually numerous, tend to group together, and measure a few millimeters to several centimeters, although they are generally uniform on the same patient. The diagnostic suspicion can be confirmed by direct examination, which reveals accumulations of yeasts and short hyphae; if these occur together, they have the typical “spaghetti and meatballs” appearance. Skin biopsy may help in atypical cases such as the present one. The most characteristic and differentiating histopathological findings of the atrophic variant include an epidermis with flattened rete ridges and, especially, reduction and fragmentation of the dermal elastic fibers.5,9 The differential diagnosis includes processes that induce skin atrophy, that is, anetoderma, morphea/atrophoderma, mycosis fungoides, sarcoidosis, and corticosteroid-induced atrophy.6,9,10
The mechanism by which species of Malasezzia can induce atrophy in the skin remains unclear. Since many of the patients reported were being treated with topical corticosteroids2–7 or systemic corticosteroids,8 atrophy was associated with the atrophogenic effect of the drugs.3–7 The fungal infection is thought to alter the epidermal barrier, thus increasing absorption of corticosteroids in the PV lesions and inducing local cutaneous atrophy. However, in corticosteroid-induced atrophy, in addition to epidermal atrophy and vasodilation, we can see atrophy of skin adnexa and reduction and fragmentation of dermal collagen, whereas in atrophic PV, we do not see alteration of collagen but alteration of the elastic fibers.5,6,9,10 We did not find collagen abnormalities in the case we report, suggesting the possibility of another pathogenic mechanism, given that cases not associated with corticosteroids have been reported.9,10 Crowson and Magro9 proposed that this form of PV appeared through a type 1 helper T-cell immune response to Malassezia antigens, in which histocytes recruited and activated by interferon-ϒ would generate the elastases responsible for the dermal elastolysis observed. Flattening of the rete ridges, on the other hand, is mediated by cytokines, such as tumor necrosis factor α and interleukin 1β, which can inhibit the nuclear factor κB pathway of keratinocytes to induce apoptosis and hinder proliferation thereof.9 In parallel, the reduced thickness and loss of hair in areas of PV has also been related to this mechanism.11 Furthermore, a type 2 helper T cell response, which could favor fungal overgrowth, has been implicated, together with the type 1 response, in the pathogenesis of atrophic PV.10
Treatment of this variant of PV is standard,10 although it has been suggested that longer regimens may be necessary and even that oral and topical approaches should be combined.5 Obviously, corticosteroids should be withdrawn.5 As a rule, the atrophy disappears; therefore, compared with other atrophying diseases, atrophying PV has a good prognosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Allegue F, Fachal C, González-Vilas D, Zulaica A. Pitiriasis versicolor atrófica. Actas Dermosifiliogr. 2018;109:455–457.