An 82-year-old woman with a history of hypertension and atrial fibrillation presented with an asymptomatic raised erythematous lesion on her right leg. The lesion had been first observed more than 6 months earlier. The patient reported that the lesion had grown gradually and did not link it to any other event.
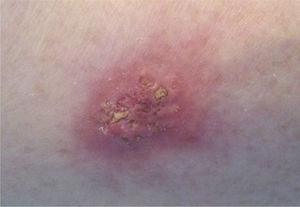
Physical ExaminationPhysical examination revealed a single, oval-shaped nodular lesion 2.5cm in diameter on the right leg. The central area of the lesion was erythematous, indurated, and raised, while the periphery was flat and whitened with a somewhat indistinct border. The central area was perforated and visibly exuded keratotic material (Fig. 1). The lesion was not tender and body temperature was not elevated.
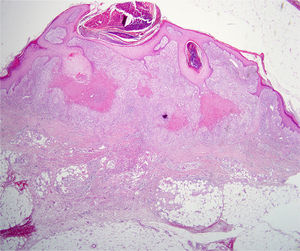
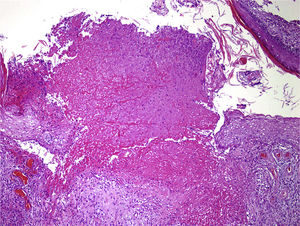
HistopathologyThe lesion was completely excised. Histopathologic examination showed epidermal acanthosis and hyperkeratosis. The superficial and mid dermis contained several granulomas with central areas of necrobiosis surrounded by epithelioid histiocytes, lymphocytes, and multinucleated giant cells. Some of these granulomatous lesions were close to the epidermis and had broken through it, releasing necrobiotic material. Colloidal iron staining revealed mucin deposits (Figs. 2 and 3).
What Is Your Diagnosis?
Diagnosis and DiscussionDiagnosisLocalized perforating granuloma annulare.
Clinical Course and TreatmentAfter excision, direct closure was performed by layers. There were no wound complications and the patient has developed no further lesions.
DiscussionPerforating granuloma annulare (PGA) was first described by Owens and Freeman1 in 1971, but had been previously described as a tuberculoulcerous form of granuloma annulare by Pinkus in 1934 and Civatte2 in 1952.
PGA is a rare form of granuloma annulare, accounting for only 5% of all cases. Most patients are children and young adults; mean age at diagnosis is 30 years, and there is a 1:1.8 male to female ratio.3
The etiology of PGA is still poorly understood. PGA is classified according to the number and location of the lesions. It is termed generalized PGA when it involves the trunk and limbs, disseminated PGA when it only involves the limbs, and localized PGA when there are very few lesions in a single area.4 Localized PGA primarily occurs on the upper limbs and palms.5 About 9% of cases consist of single lesions.3
PGA may sometimes present as reddish papules measuring 1 to 5mm, with umbilication or central crusting.3 In 17% of cases, PGA is associated with diabetes mellitus; the age of onset is higher in this subgroup.5 Other reported associations include human immunodeficiency virus, herpes zoster, tuberculosis, hypothyroidism, lymphomas, rheumatoid arthritis, coronary syndromes, bronchitis, and rhinitis.
Microscopically, PGA is characterized by the presence in the superficial or mid dermis of one or more necrobiotic granulomas containing central areas of mucin, degenerated collagen, and fibrin surrounded by histiocytes, lymphocytes, and multinucleated giant cells. A channel, ulcer, or area of destroyed epidermis can be observed through which necrobiotic material is eliminated. This material is typically covered by a crust or by parakeratotic stratum corneum. Increased presence of mucin is found in 70% of lesions.6
Differential diagnosis includes molluscum contagiosum, primary perforating disorders, bites and stings, keratoacanthoma, pityriasis lichenoides et varioliformis acuta, papulonecrotic tuberculid, and perforating forms of sarcoidosis or necrobiosis lipoidica.
Localized lesions and asymptomatic lesions regress spontaneously in 70% of cases and thus require no treatment. Topical treatments used for PGA include corticosteroids, calcineurin inhibitors, and vitamin E, while systemic treatment may be attempted using dapsone, retinoids, antimalarial agents, pentoxifylline, nicotinamide, tumor necrosis factor inhibitors, or phototherapy. No absolute benefit has been shown for any of these treatments, and there is no clinical trial evidence to support their use.
Please cite this article as: González Fernández D, Vivanco Allende B, Gómez Díez S. Nódulo asintomático en la pierna. Actas Dermosifiliogr. 2015;106:229–230.