We present the case of a woman aged 59 years with a history of left renal agenesis. She came to outpatients with a 2-month history of persistent painful lesions on both hands. She had been treated with oral corticosteroids (deflazacort, 30mg, in a tapering regimen) and topical methylprednisolone aceponate with no improvement. On examination, indurated red-violaceous papulonodular lesions were observed on the dorsum of the fingers and on the palms of both hands (Fig. 1A).
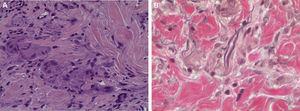
Histology revealed a dermal granulomatous lesion with no areas of necrobiosis and with numerous multinucleated giant cells showing elastophagocytosis, suggestive of annular elastolytic giant cell granuloma (AEGCG) (Fig. 2, A and B).
After making the diagnosis and because of the lack of response to corticosteroid therapy, treatment was started with dapsone, 100mg/d, leading to complete resolution of the lesions after 4 months of treatment, with no recurrence after a year of follow-up (Fig. 1B).
AEGCG is a rare granulomatous disease characterized by the appearance of annular lesions with elevated borders formed of erythematous papules that spread centrifugally to leave an atrophic central area. Histologically, dermal granulomas formed of histiocytes and multinucleated giant cells are observed in close association with degenerated elastic fibers and elastophagocytosis. The lesions are usually asymptomatic, although mild pruritus or pain can develop, and they tend to persist for months or years, after which spontaneous remission typically occurs. The first case was described in 1975 by O’Brien,1 who coined the term actinic granuloma as the lesions arose in sun-exposed areas. In 1979, Hanke et al.2 proposed the term annular elastolytic giant cell granuloma to describe a case of lesions of identical characteristics localized in areas not exposed to the sun; this is now the most widely accepted name for the condition.
The etiology is unknown, although, based on the preference for sun-exposed areas or areas with a history of burns, and no involvement of areas in which elastic fibers are absent, such as scars and striae distensae,3 the most widely held hypothesis is that UV radiation, the increased temperature, and other still-unknown factors can modify the antigenicity of elastic fibers, giving rise to an immune response with the formation of a granulomatous infiltrate.4
The number of lesions varies from a single lesion to widespread forms with systemic involvement.5 An association has been reported with diabetes mellitus and with solid and hematologic tumors, and some authors recommend screening for occult malignancy in these patients. Variants of the disease exist, including the papular,6 reticular, and exanthematous forms.7
The differential diagnosis includes other granulomatous diseases, both infectious, due to fungi and mycobacteria, and inflammatory, such as granuloma annulare, necrobiosis lipoidica, sarcoidosis, and annular lichen planus. AEGCG can be clinically indistinguishable from any of these diseases, and histology is the gold standard for confirming the diagnosis.
Little scientific evidence is available on the treatment of AEGCG, and the self-limiting nature of the disease, with a tendency to spontaneous disappearance of the lesions, makes it difficult to establish the efficacy of the different therapeutic regimens. Recommendations are based on isolated case reports or case series in which different therapeutic agents have been used with variable efficacy.8 These agents include topical or systemic corticosteroids, topical calcineurin inhibitors, phototherapy, cryotherapy, antimalarial drugs, retinoids, ciclosporin A, tranilast, methotrexate, fumaric acid esters, pentoxifylline, clofazimine, and dapsone. We have only found 1 case report, dating from 1997, of a patient treated with dapsone with a good response.9
Dapsone (4,4-diaminodiphenyl sulfone) is a synthetic sulfone with a dual antimicrobial–anti-inflammatory mechanism of action. Since its incorporation into dermatology in the mid-twentieth century, its therapeutic indications have broadened. It is used mainly in the inflammatory neutrophilic and eosinophilic dermatoses, though there are also anecdotal reports of therapeutic success in many other entities, including AEGCG.10 The starting dose in adults is 50 to 100mg/d; this can be increased to 300mg/d to achieve the therapeutic objective, afterwards returning to the minimal effective dose.
In conclusion, we have presented a case that is interesting for 2 reasons: the atypical site of the lesions in an area not exposed to the sun, and being the second reported case with an excellent response to dapsone.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: García MTM, Rodríguez JJP, de Zulueta Dorado T, Sánchez JC-M. Granuloma elastolítico anular de células gigantes en área no fotoexpuesta con respuesta a dapsona. Actas Dermosifiliogr. 2016;107:531–533.