Melanoma is the most serious type of skin cancer and is caused by a combination of endogenous and exogenous risk factors. Here were describe the clinical and anatomical characteristics of melanoma along with the endogenous and exogenous risk factors in 120 patients diagnosed with cutaneous melanoma in a health care area of the province of Santa Cruz de Tenerife in Spain.
Patients and methodsA descriptive, cross-sectional study was undertaken in patients diagnosed with melanoma between January 1999 and July 2005 in the health care area served by Hospital Universitario de Canarias. Data were collected on demographic characteristics, phenotype, sun exposure, sun protection, and actinic damage.
ResultsMelanoma was most commonly diagnosed in women (62.5%) and lesions were most frequently located on the trunk. The most frequent tumor subtype was superficial spreading melanoma (63.3%) and 51.5% of patients were classified as having skin phototype II. Intermittent sun exposure was reported by 81.8% of patients and 50% had a moderate cumulative sun exposure (50-120h/y). Multiple melanomas were present in 3.3% of patients. In 43% of patients, the time to diagnosis of melanoma was more than 24 months.
ConclusionsA substantial percentage of melanomas were associated with actinic damage. Differences were observed in the level of sun exposure according to melanoma subtype. The most common causes for concern were growth and color changes in the lesion, and a substantial number of patients waited for some time between observing these changes and consulting a doctor.
El melanoma es la forma más grave de cáncer cutáneo, y está ocasionado por una combinación de factores de riesgo endógenos y exógenos. En el presente trabajo se describen las características anatomoclínicas, factores de riesgo endógenos y exógenos en 120 pacientes diagnosticados de melanoma cutáneo en el área sanitaria norte de la provincia de Santa Cruz de Tenerife.
Pacientes y métodoSe realizó un estudio descriptivo transversal sobre los pacientes diagnosticados de melanoma en el área sanitaria que cubre el Hospital Universitario de Canarias, entre enero de 1999 y julio de 2005. Se obtuvieron los datos referentes a las características epidemiológicas, fenotipo, hábitos de exposición solar, fotoprotección y daño actínico.
ResultadosLos melanomas se diagnosticaron con más frecuencia en mujeres (62,5%). La localización anatómica más frecuente fue el tronco. El tipo anatomoclínico más frecuente fue el melanoma de extensión superficial (63,3%). El 51,5% de los pacientes presentaban un fototipo II. El 81,8% de los pacientes refirió una exposición solar intermitente y el 50% manifestaron una exposición solar acumulada moderada (50-120 horas/ año). El 3,3% de los pacientes presentaron melanomas múltiples. El tiempo de evolución del melanoma fue elevado (el 43% refiere lesiones de más de 24 meses de evolución).
ConclusiónUn gran porcentaje de melanomas se asocia a daño actínico. Se observaron diferencias entre la intensidad de la exposición solar y el tipo anatomoclínico. El motivo de alarma más frecuente fue el crecimiento y el cambio de color, y un porcentaje importante de pacientes consultaron tardíamente tras la aparición de los signos de alarma.
Melanoma is generally considered to be a disease of white-skinned individuals.1 Its occurrence is influenced not only by endogenous risk factors but also by environmental determinants such as exposure to the sun.
Melanoma has also been associated with a global increase in tumors arising from actinic damage, including actinic keratosis, basal cell carcinoma, and squamous cell carcinoma.2 The presence of actinic keratosis has recently been associated with an increased risk of melanoma, especially in the head region.3 Sun exposure is thought to be one of the main modifiable environmental risk factors for melanoma. It is thought that total sun exposure, recent sun exposure, occupational exposure, and intermittent or recreational exposure differ in their impact on melanoma risk.4
The aim of this study was to describe the endogenous risk factors (phototype, skin and eye color, number of melanocytic nevi, presence of dysplastic nevi, and individual or family history of melanoma), exogenous risk factors (type and degree of cumulative sun exposure, history of sunburn, and sun protection behavior), and reason for consultation in patients diagnosed with cutaneous melanoma in the northern health care region of Santa Cruz de Tenerife, Spain between 1999 and 2005.
Material and MethodsWe undertook a cross-sectional descriptive study of patients diagnosed with melanoma in the northern health care area of the province of Santa Cruz de Tenerife between 1999 and 2005. A total of 120 patients with cutaneous melanoma (incident cases) were evaluated. Data were obtained on epidemiological variables previously described in the literature as associated with cutaneous melanoma.
Data were collected on the following variables:
- 1.
Tumor type: lentigo maligna melanoma (LMM), acral lentiginous melanoma (ALM), superficial spreading melanoma (SSM), and nodular melanoma (NM)
- 2.
Tumor site
- 3.
Breslow thickness, ulceration, and regression
- 4.
Phototype according to the Fitzpatrick classification
- 5.
Type of sun exposure (constant or occupational versus intermittent or recreational), eye color, hair color, history of actinic damage, degree of cumulative sun exposure, and history of burns caused by ultraviolet radiation.
Sun exposure was classified according to the period of the patient's life in which it occurred (0-10 years, 10-18 years, >18 years) and the degree of exposure: no exposure, low exposure (<50hours per year), moderate exposure (50-120hours per year), and intense exposure (>120hours per year). The number of times sunburn occurred was also recorded for each phase of the patient's life. In addition, use of sun protection was evaluated. Personal and family history of melanoma, presence of dysplastic nevi, and total number of nevi were recorded for each patient. The reason for consultation for melanoma was recorded along with the time since appearance of the lesion in months and the time elapsed between observation of warning signs and consultation.
Statistical AnalysisCategorical variables were expressed as frequencies and percentages and continuous variables as means (SD). Proportions were compared by χ2 test or Kruskal-Wallis test.
The mean age of men and women was compared by t test, assuming a normal distribution of the frequencies.
Statistical analysis was carried out using the statistical packages SPSS 12.0 (Chicago, Illinois USA) and StatXact v: 5.0.3 (Cambridge, Massachusetts, USA).
Two-tailed tests were used and statistical significance was set at P<.05.
ResultsTables 1–3 show data on the epidemiological and histological characteristics, tumor type, and site of melanoma observed in our patients.
Epidemiological and Histological Characteristics.
| Characteristic | No. of patients (total=120) | % |
| Sex | ||
| Male | 45 | 37.5 |
| Female | 75 | 62.5 |
| Age | ||
| <40 y | 27 | 22.5 |
| 40-60 y | 46 | 38.3 |
| >60 y | 47 | 39.2 |
| Site | ||
| Head and neck | 23 | 19.2 |
| Trunk | 46 | 38.3 |
| Upper limbs | 26 | 21.7 |
| Lower limbs | 25 | 20.8 |
| Tumor type | ||
| LMM | 10 | 8.3 |
| SSM | 76 | 63.3 |
| ALM | 8 | 6.7 |
| NM | 17 | 14.2 |
| Not classified | 9 | 7.5 |
| Ulceration | ||
| Yes | 20 | 16.5 |
| No | 100 | 83.5 |
| Regression | ||
| Yes | 14 | 11.7 |
| No | 106 | 88.3 |
Abbreviations: ALM, acral lentiginous melanoma; LMM, lentigo maligna melanoma; NM, nodular melanoma; SSM, superficial spreading melanoma.
Anatomical Site and Tumor Type.
| Site | Total | LMM | SSM | ALM | NM | Not Classified | ||||||
| No. | (%) | No. | (%) | No. | (%) | No. | (%) | No. | (%) | No. | (%) | |
| 120 | 100 | 9 | 7.5 | 76 | 63.3 | 8 | 6.7 | 17 | 14.2 | 10 | 8.3 | |
| Head | ||||||||||||
| Total head | 23 | 19.2 | 9 | 100 | 4 | 5.3 | 0 | 0 | 7 | 41.2 | 3 | 33.3 |
| Scalp | 5 | 4.2 | 2 | 22.2 | 1 | 1.3 | 2 | 11.8 | ||||
| Face | 14 | 11.7 | 6 | 66.7 | 2 | 2.6 | 4 | 23.5 | 2 | 22.2 | ||
| Neck | 3 | 2.5 | 1 | 1.3 | 1 | 5.9 | 1 | 11.1 | ||||
| Not specified | 1 | 0.8 | 1 | 11.1 | ||||||||
| Trunk | ||||||||||||
| Total trunk | 46 | 38.3 | 0 | 0 | 37 | 48.7 | 0 | 0 | 5 | 29.4 | 4 | 44.4 |
| Anterior | 13 | 10.8 | 10 | 13.2 | 2 | 11.8 | 1 | 11.1 | ||||
| Posterior | 30 | 25 | 24 | 34.3 | 3 | 17.6 | 3 | 33.3 | ||||
| Not specified | 3 | 2.5 | 3 | 3.9 | ||||||||
| Upper limbs | ||||||||||||
| Total upper limbs | 26 | 21.7 | 0 | 0 | 17 | 22.4 | 3 | 37.5 | 4 | 23.5 | 2 | 22.2 |
| Upper arm | 11 | 9.2 | 6 | 7.9 | 1 | 12.5 | 3 | 17.6 | 1 | 11.1 | ||
| Forearm | 11 | 9.2 | 8 | 10.5 | 1 | 12.5 | 1 | 5.9 | 1 | 11.1 | ||
| Hands | 3 | 2.5 | 2 | 2.6 | 1 | 12.5 | ||||||
| Not specified | 1 | 0.8 | 1 | 1.3 | ||||||||
| Lower limbs | ||||||||||||
| Total lower limbs | 25 | 20.8 | 0 | 0 | 18 | 23.7 | 5 | 62.5 | 1 | 5.9 | 1 | 3.9 |
| Thigh | 3 | 2.5 | 3 | 3.9 | ||||||||
| Lower leg | 12 | 10 | 9 | 11.8 | 1 | 12.5 | 1 | 5.9 | 1 | 3.9 | ||
| Foot | 9 | 7.5 | 5 | 6.5 | 4 | 50 | ||||||
| Not specified | 1 | 0.8 | 1 | 1.3 | ||||||||
Abbreviations: ALM, acral lentiginous melanoma; LMM, lentigo maligna melanoma; NM, nodular melanoma; SSM, superficial spreading melanoma.
Phototype II was the most common skin type, observed in 51.5% of patients, followed by phototype III in 37.9%. Phototype III was most common in men and phototype II in women. Most patients (52.5%) had brown eyes and 16.8% had green eyes. Dark eyes were more common in men than women (P=.025). Brown hair was most common (52.5% of patients), followed by black (24.8%), blonde (20.8%), and red hair (2%).
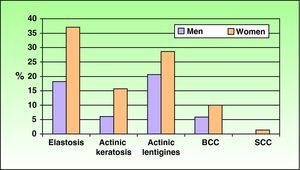
Solar elastosis was the most common form of actinic damage and was present in 37.1% of women and 18.2% of men (P=.041) (Fig. 1).
Sun exposure was reported as intermittent in 81.8% and chronic in 18.2% of patients.
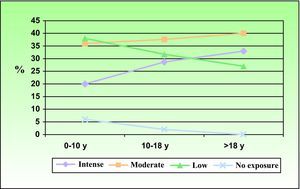
Figure 2 shows cumulative sun exposure during the different periods of the patient's life. A substantial proportion of patients had moderate or intense exposure during childhood and adolescence. Intense sun exposure was reported by a larger proportion of women (41.2%) than men (15.6%) (P=.034).
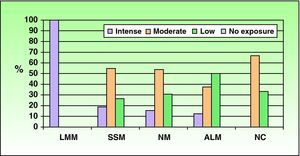
Significant differences were also observed in total cumulative sun exposure according to tumor type (P=.047), with intense sun exposure more frequent in patients with LMM (100% of patients) and moderate exposure in those with SSM (54.7% of patients) and NM (53.8% of patients) (Fig. 3).
A large proportion of patients had never used sunscreen. During the period between 10 and 18 years of age, 18.8% of male patients routinely used sun protection compared with 2.9% of female patients (P=.037).
Most patients had no history of sunburn (40%) or reported between 1 and 3 episodes of sunburn per year in almost all periods of their life (49%).
Multiple melanomas were present in 4 patients (3.3%): 3 patients with 2 melanomas and 1 patient with 3. All cases of multiple melanoma occurred in women. One of the patients with multiple melanomas had a family history of melanoma. The second melanoma in all cases had a shallower Breslow thickness than the first. The total number of nevi was less than 50 in 68.5% of patients, 50 to 100 in 19.6%, 100 to 150 in 7.6%, and more than 200 in 4.3%. Dysplastic nevi were observed in 5.7% of patients.
Eight patients (7.1%) had a family history of melanoma, and this was more common in women than men.
Melanomas occurred on medium-sized or small congenital nevi in 7.5% of cases. The percentage of patients with melanomas on congenital nevi was slightly higher in women (8%) than men (6.7%).
The time since appearance of melanoma was long in this study, with 43% of patients reporting lesions that had appeared more than 24 months previously and only 1.2% of lesions having appeared within the last 1 to 3 months. In 43.75% of patients, no more than 3 months had passed between observing warning signs and consulting the doctor. In a notable percentage of patients, however, consultation was very late, with delays of 6 to 12 months in 29.7% and of 12 to 24 months in 5%. The patients who consulted late (after 6 months or more) had a mean age at diagnosis of 53 years and most were women (69%). The most common reason for consultation was the growth of the lesion (52.3%), followed by changes in color. Change in shape and bleeding were the least common causes of consultation (16.5% and 12.8%, respectively). The frequency of consultation due to changes in the color of the lesion varied according to the site of melanoma (P=.043), with color change mainly leading to consultation in patients with melanoma on the lower limbs (58.2%). Differences were also observed for bleeding of the lesion at different sites (P=.045), with bleeding mainly leading to consultation when the lesion was located on the head (31.6%).
DiscussionOur finding of a higher frequency of melanoma in women than men coincides with the results of other studies.5,6 The mean age at diagnosis was similar to that reported in the literature (around 50 to 60 years), as was the finding that men were older than women.5,7,8 The most common site of melanoma reported in the literature is the trunk, but the second most frequent site varies according to the study, in some cases the lower limbs7 and in others the head and neck.5,6 In our study, the most common site was the trunk, and we obtained similar percentages for the lower and upper limbs; the least common sites were the head and neck. The most common anatomical sites described in the literature are the lower limbs in women and the trunk in men,7 a finding that was confirmed in our study. The most common tumor type reported in the literature is SSM,5,7 as observed in our study. Tumor type is also linked to anatomical site. SSM was more common on the trunk and the lower limbs,8 whereas LMM and NM are found most often on the face.9 We also observed significant differences in the types of tumor found at different anatomical sites (P<.001), with NM the most frequent type on the head, followed by LMM. On the trunk and upper limbs, the most frequent melanoma type was SSM followed by NM, and on the lower limbs it is SSM followed by ALM.
Our data on phenotypic characteristics were similar to those of some studies undertaken in Spain, where the most common phototype in patients diagnosed with melanoma was type II followed by phototype III.6 However, a study by Nagore et al5 found that the most common phototype in all groups of patients with melanoma was type III-IV. In our study, the majority of patients had dark hair (brown) and brown eyes, which is similar to the findings of other Spanish studies.5
Melanoma has been linked to the worldwide increase in tumors caused by actinic damage, including actinic keratosis, basal cell carcinoma, and squamous cell carcinoma. In the study by Nagore et al,5 which included patients diagnosed with primary cutaneous melanoma, actinic keratosis was observed in 30.5% of patients with melanoma located on chronically sun-exposed skin, whereas the percentage was lower in patients with melanoma located on intermittently exposed or unexposed skin (8.3% and 11.3%, respectively). Solar lentigines were present in 92.7% of patients with melanoma on chronically sun-exposed areas, in 86.2% of patients with melanoma on intermittently exposed skin, and in 76.7% of patients with melanoma in unexposed areas.5 In our study, we observed a similar percentage of patients with actinic keratosis (12.6%) to that of the group of patients with melanoma on intermittently exposed or unexposed skin in the study by Nagore et al. Actinic lentigines were present in 26% of patients, a much lower percentage than observed in any of the groups of patients included in the study by Nagore et al.5 Solar elastosis was the most common form of actinic damage in our study, with a higher percentage of sun damage observed in women. This differs from the results of some other studies, in which there was a higher frequency of sun damage in men.10
Our findings on sun exposure in patients with melanoma were similar to those of other studies, where most patients reported intermittent rather than continuous sun exposure. For instance the study by Gómez et al6 found that 74% of patients had intermittent sun exposure and 26% had constant sun exposure. In the study by Nagore et al,5 intermittent sun exposure was reported by 96.7% of patients with melanoma located on intermittently exposed skin, 77.8% of patients with tumors located on chronically exposed skin, and 71.9% of patients with melanoma on an unexposed site.
In our study, the use of sunscreen prior to diagnosis of melanoma was less common than that observed in other studies. Gómez et al6 found that 43.1% of patients used sunscreen regularly prior to diagnosis, 23.1% used it occasionally, and 33.8% never used it. In our study, less than 15% of patients used sunscreen prior to diagnosis of melanoma. This may be explained by the mean age of our patients (around 50 years), since the use of sunscreen has only been promoted in recent years. We found similar rates of sunburn to those observed in other studies, where most patients reported never having been burnt or only having been sunburnt on between 1 and 5 occasions.5Patients with a history of melanoma have an increased risk of developing a second melanoma.2 A study by Ferreres et al11 assessed the risk of multiple primary melanoma in 934 patients diagnosed with melanoma in the Mediterranean population and found that multiple melanomas occurred in 2.6% of cases (similar to our finding of 3.3%). Unlike in our study, where all cases of multiple melanoma occurred in women, they found a slightly higher frequency in men (52%). Similar to our results, Ferreres et al. found that 80% of patients with multiple melanoma had 2 melanomas and 16% had 3. As in our study, all reports in the literature show the second melanoma to have a shallower Breslow thickness than the first.11–13
The percentage of patients with more than 50 nevi was slightly lower than that reported in the literature for patients with melanoma. This may be because of the characteristics of the population in the health care area analyzed, where patients are darker skinned and less likely to have nevi. The percentage of melanomas on small or medium-sized congenital nevi was higher than that described in the literature, where most melanomas are reported to arise from giant congenital nevi.14,15
A study by Schmid-Wendtner et al16 to analyze the delay in diagnosis of cutaneous melanoma in 233 patients found that close to a third of patients (29.2%) waited more than 12 months after observing changes in a pigmented lesion before they consulted a doctor. Those findings are similar to the results obtained in our study, where approximately 30% of patients waited between 6 and 12 months before consulting a doctor. The mean age of those patients at diagnosis was 53 years and most were women (69%). In addition, in the study by Schmid-Wendtner et al,16 the most commonly reported warning signs were changes in the color and size or thickness of the lesion, as found in our study. These findings highlight the importance of campaigns to promote early diagnosis, informing citizens of warning signs in pigmented lesions (asymmetry, irregular borders, color changes, diameter of more than 6mm, and changes in the growth of a pigmented lesion) and encouraging patients to carry out periodic self-examination.17
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fagundo E, et al. Estudio de las características fenotípicas y exposición a radiación ultravioleta en pacientes diagnosticados de melanoma cutáneo. Actas Dermosifiliogr.2011;102:599-604.