Langerhans cell histiocytosis (LCH) is a rare, clonal disorder of immature Langerhans cells that can involve various organs and especially the skin, bone, lungs and pituitary gland. The disease is most commonly seen in infants, children and is rare in adulthood.1,2 Skin limited Langerhans cell histiocytosis in adults is even less common.2,3
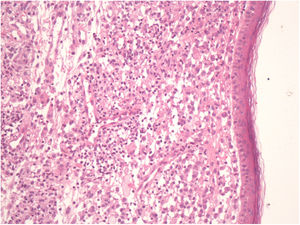
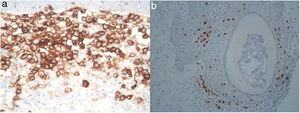
A 73-year-old male patient presented to our clinic complaining of a patch on his back that had appeared about a year ago and gradually enlarged. There was nothing of significance in his medical history. Although he had a 15 pack/year cigarette-smoking history, he had stopped smoking 30 years prior to his diagnosis. The dermatologic examination revealed xanthoma-like plaques on his back, that had composed with the accumulation of yellow-orange papules on an erythematous background, and erythematous papules (Fig. 1). Skin biopsy was taken for differential diagnosis of diffuse plane xanthoma. Histopathological examination revealed dense clusters of Langerhans cells with an eosinophilic cytoplasm, grooved or lobular nucleus; histiocytes with abundant pale cytoplasm, multinucleated giant cells and lymphocytes in the dermis (Fig. 2). Langerhans cells stained the positive for CD1a, CD207 (langerin) and S100 (Fig. 3a-3b). The diagnosis of LCH skin involment was confirmed with histological and immunohistochemical analysis of skin biyopsy. BRAFV600E mutation was been detected in skin tissue sample.
Computed tomography (neck, thorax, abdomen, pelvic), also pituitary magnetic resonance scan failed to demonstrate systemic involvement. The patient was diagnosed with LCH skin involvement. He was referred to pulmonology, medical oncology, hematology and endocrinology departments and there was no extracutaneous involvement.
Treatment was started with topical corticosteroids and PUVA treatment with oral 8- Methoxypsoralen (8-MOP). The patient had photosensitivity reaction to PUVA after 46 sessions and treatment was changed to UVA with topical 0.1% 8-MOP gel. Phototherapy resulted with healing of the erythematous papules, erosions and thinning of the yellow-orange plaques (Fig. 1). The sixth month follow-up thoracic computed tomography image revealed parenchymal involvement consistent with LCH. Bronchoalveolar lavage investigation showed a large number (90%) of histiocytes and a small number of polymorphonuclear leukocytes. The patient was diagnosed with multi-systemic LCH and started methotrexate treatment, in the first week with a 5mg test dose and then as 20mg per weekly. The patient was stable with methotrexate treatment for 6 months.
The diagnosis of LCH is based on clinical and histopathological evidence with microscopic examination and immunohistochemical features of langerhans cells.1,4 Detection of LC markers CD1a and CD207 (langerin) is essential to confrim diagnosis and evaluation of Birberck granules on electronic microscopy has been using less frequently.4 İn this case CD1a and CD207 were positive with immunohistochemical investigation of the cells, with eosinophilic cytoplasm and grooved or lobular nucleus.
Skin lesions of LCH can be limited to a single anatomic region or generalized, and consist of diffused papules, nodules or plaques, and can mimic seborrheic dermatitis in addition to prurigo nodularis, eczema, psoriasis, candidiasis or intertrigo.1,5 Since skin involvement can be the initial symptom of systemic disease, these patients should be evaluated in terms of multi-organ involvement.6,7 Our patient had atypical lesions, xanthoma-like plaques and erythematous papules on his back and waist.
Clinical evidence of LCH vary based on the affected organ or system, from self- healing disease to chronic recurrences and it may resulted in patient being underdiagnosed.1 Podjasek et al reported a LCH case, followed-up with a misdiagnosis of inflammatory intestinal disease, was diagnosed with skin lesions and had gastrointestinal, lung and liver involvement. Skin biopsy may be valuable for diagnosis of LCH.7 Our case developed lung involvement about 8 months after he was first diagnosed with LCH skin involvement. Additionaly, lung involvement of LCH is more frequently in adults and strongly associated with smoking.4
BRAFV600E mutation has been detected in approximately half of LCH samples. Recently, it is suggested to research BRAFV600E mutation in all samples with difficult cases.4 In our case, we detected BRAFV600E mutation in skin tissue sample.
LCH may affect any organs and revised classification contains 4 subtypes of LCH depending on the number of organs or systems involved, lung involvement and involvement of risk organs (liver, spleen and bone marrow).4 Treatment recommendations are determined according severity of disease.1 The treatments used include topical and systemic steroid treatment, phototherapy, topical nitrogen mustard, azathioprine and methotrexate.1,8 In our case erythematous papules, perilesional erythema and eroded areas resolved with PUVA treatment but the xanthoma-like plaques showed thinning.
LCH in adults is difficult to diagnose as it is rare and skin involvement can vary in appearance. Skin biopsy is significant to diagnose skin involvement. It can be the initial sign of multi-systemic LCH although the condition can rarely be limited to the skin. Close follow-up of adult-onset LCH patients with skin involvement is therefore essential in terms of future potential multi-organ involvement.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Boyuk E, et al. Placas similares a xantomas como forma de presentación de una histiocitosis de células de Langerhans en un paciente en edad adulta. Actas Dermosifiliogr. 2020;111:71–73.