Eruptive pseudoangiomatosis is an uncommon skin disease of unknown etiology that is increasingly reported in children. The condition may be preceded by a prodrome comprising fever and respiratory or gastrointestinal symptoms during the days before onset of the skin lesions. The rash is characterized by the appearance of multiple asymptomatic reddish-violaceous papular lesions that present with a specific peripheral whitish halo and that disappear on diascopy. The lesions are found mainly on areas exposed to sunlight and resolve spontaneously without residual marks after 10–15 days.
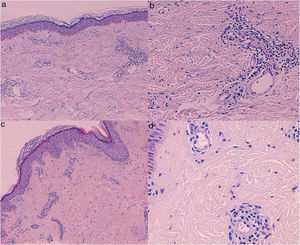
Histopathology usually reveals vascular dilatations with endothelial cells that project toward the vascular compartment, together with a perivascular infiltrate and no signs of vasculitis, capillary proliferation, or extravasated erythrocytes. While not disease-specific, these histological findings are consistent with the diagnosis in a patient with a compatible clinical picture.
We report the case of a 7-year-old girl with no history of interest who was referred to our clinic with an episode of asymptomatic erythematous lesions that had appeared more than 1 week earlier. The lesions affected the face and arms. She had a 2-year history of similar outbreaks. These were self-limiting and had gradually increased in frequency from 3 episodes per year to 1 per month. The episodes were not preceded by systemic symptoms, and no clear triggers were identified.
The patient’s grandmother, who was aged 55 years, had experienced similar episodes, with lesions in the form of self-limiting flares, from the fourth decade of life. The number of lesions increased gradually, and the episodes became more frequent (1–2 per month at the time of consultation). These were located on the face, arms, and thorax. The patient had a history of rheumatoid arthritis diagnosed at age 40 years (after onset of the symptoms) and had received treatment for infiltrating ductal carcinoma at age 53 years (tamoxifen, anti-inflammatory drugs, and low-dose prednisone). Neither of the patients had presented symptoms before onset of the rash or during the rash.
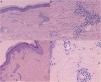
In both patients, examination revealed reddish-wine colored papules measuring 2−3mm in diameter. Most were surrounded by a peripheral hypochromic halo and blanched on diascopy (Fig. 1). The girl’s lesions were located mainly on the cheeks and arms, whereas those of the grandmother were found mainly on the forearms. Histopathology of biopsy specimens from both patients was indicative of eruptive pseudoangiomatosis (Fig. 2).
Skin biopsies (hematoxylin-eosin) from patients 1 (A, B) and 2 (C, D). A, C (×40), Dilation of superficial dermal vessels, with mild dermal edema and perivascular inflammatory infiltrate. Note the absence of vasculitis, capillary proliferation, and erythrocytic extravasation (×200). B, D, Endothelial cells projecting toward the vascular compartment, together with perivascular infiltrate.
The laboratory tests performed in the case of the girl revealed no relevant abnormalities in the complete blood count, biochemistry, coagulation, or complement. The antinuclear antibody titer was negative, as were the results of serology testing for Epstein-Barr virus, cytomegalovirus, Rickettsia conorii, Echinococcus granulosus, parvovirus, and Borrelia burgdorferi. Determination of immunoglobulin G was positive for Coxsackie A and B (IgM was negative).
After 1 year of follow-up, both patients continue to experience periodic skin rashes with no associated symptoms.
Eruptive pseudoangiomatosis was initially described as a childhood rash, although many cases were subsequently reported in adults, whose symptoms differ from those of the classic infant presentation, with no prodrome and slower resolution of the lesions.1,2 The differential diagnosis of this clinical picture is mainly with senile angioma, bacillary angiomatosis, telangiectasia, and insect bites.
Infection was proposed as the most likely cause of the disease; the most frequently associated infection in the literature is that by enteric cytopathic human orphan virus, which might explain the concomitant presentation in relatives1,3,4 and community outbreaks. However, the matter continues to be controversial, since other possible triggers include insect bites,5 drugs, and certain foods. Furthermore, this entity has been associated with immunosuppressive states such as kidney transplant, pemphigus vulgaris, and immunosuppressive agents, although in the case we report, the patient initiated prednisone several years after the onset of eruptive pseudoangiomatosis. Cases of recurrent eruptive pseudoangiomatosis have been reported6–9; in most, the recurrences were scarce and occurred during the year following the first episode, with no systemic symptoms before the recurrences.
The recurrent familial presentation is very infrequent, and only 5 cases in 2 family units have been published in the literature4; all 5 cases involved children or adolescents. In the cases reported, the number of recurrences was low, and these occurred during the 2 years following the initial episode; in one of the families, there was a single simultaneous recurrence in the 3 members. This differs from the cases we report, where the recurrences presented with a frequency of 1–2 episodes per month, and in an adult with more than 10 years since the initial episode. Such an atypical recurrent presentation in 2 family members could indicate greater genetic susceptibility to the development of this process, although we were unable to identify a clear trigger.
In conclusion, we report 2 cases of familial eruptive pseudoangiomatosis with multiple recurrent episodes. Our findings point to the possibility of a greater genetic disposition to this skin rash in the patients we describe. Both cases were characterized by more marked expression of the disease than reported to date.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Harana C, del Boz-González J, Padilla-España L, Rodriguez-Lobalzo S, de Troya-Martín M. Pseudoangiomatosis eruptiva familiar: 2 casos de presentación recurrente. Actas Dermosifiliogr. 2020;111:73–75.