BASCULE Syndrome (Bier anemic spots, cyanosis, and urticaria-like eruption) is a vasomotor dermatosis characterized by the triad of Bier anemic spots, cyanosis, and urticarial lesions. Few cases have been described in the literature, mainly in pediatric patients. Its diagnosis is clinical. Although it is a benign and transient disorder, in adolescents it may be associated with chronic orthostatic intolerance syndrome, and screening is advised. Currently, there is no effective treatment.
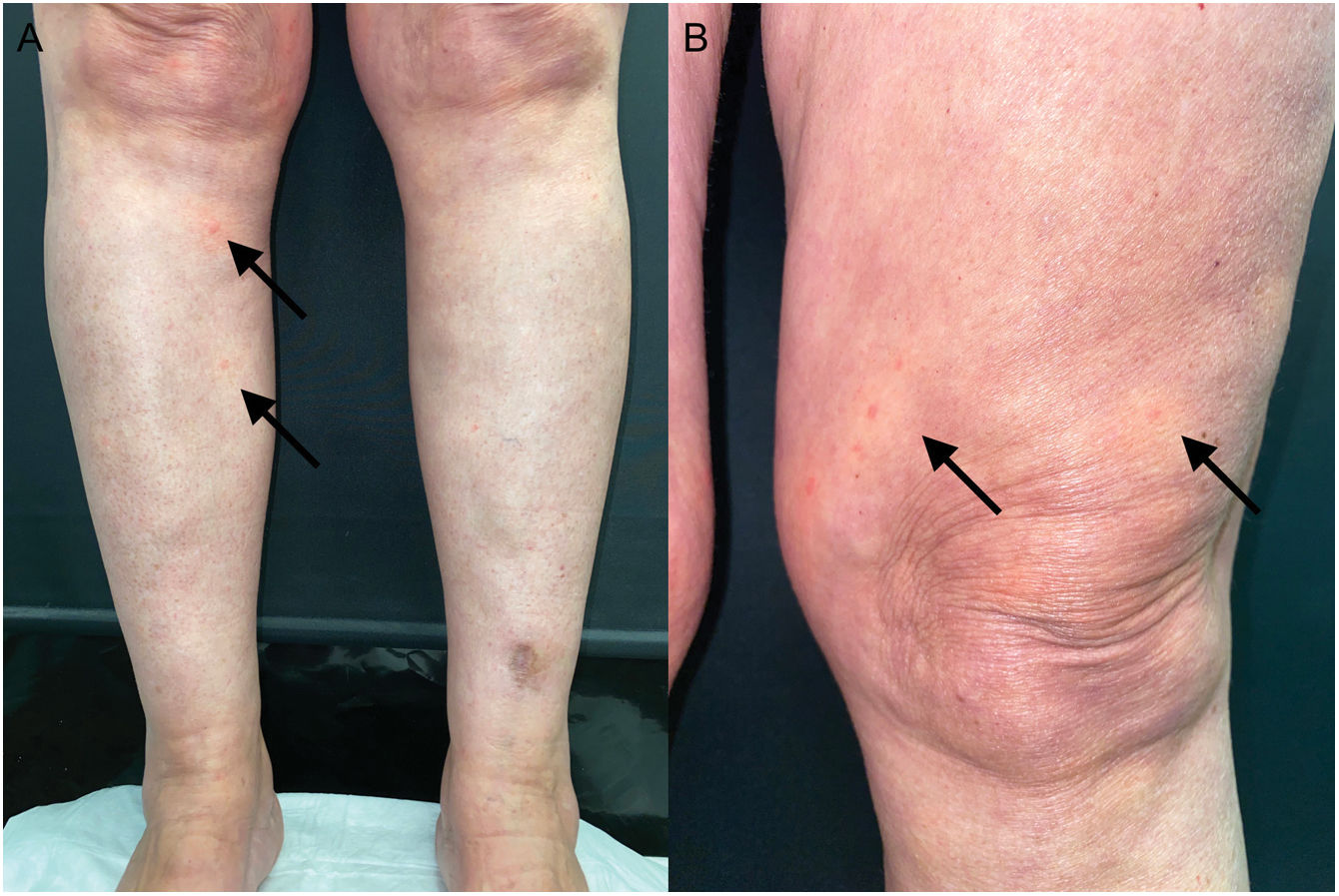
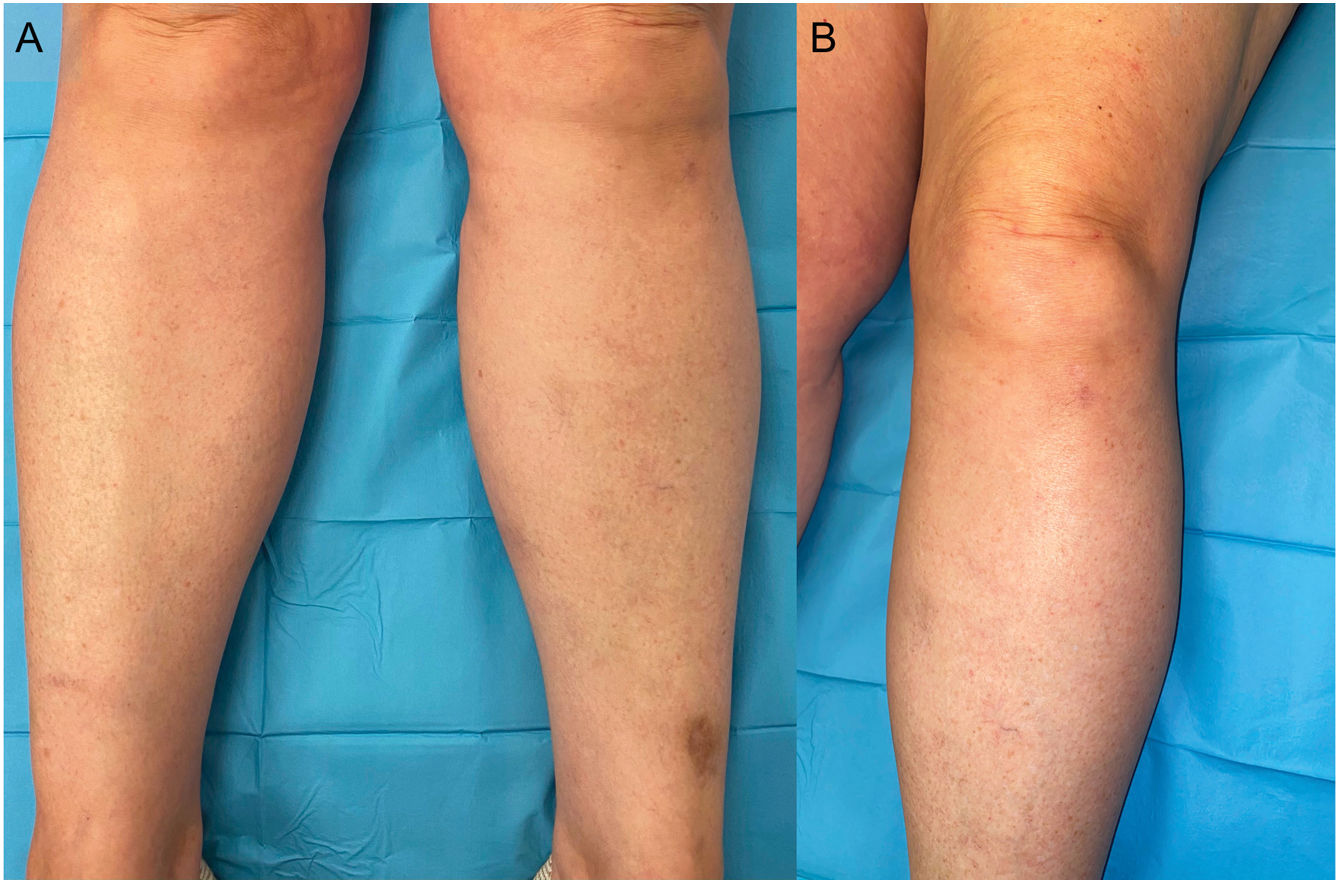
A 58-year-old woman with a history of breast cancer in remission referred to our dermatology department due to pruritic lesions on the lower extremities following prolonged standing, occurring for the past 4 years. The most recent flare-up began 3 months ago, coinciding with the cessation of smoking and an upper respiratory tract infection of unknown etiology. Physical examination while seated was unremarkable, but after standing for a few minutes, hypochromic macules centered by an erythematous-orange papule on a cyanotic base were observed up to the thighs (Fig. 1). Upon returning to a seated position, the lesions disappeared spontaneously (Fig. 2). Additionally, she reported a sensation of instability following abrupt postural changes.
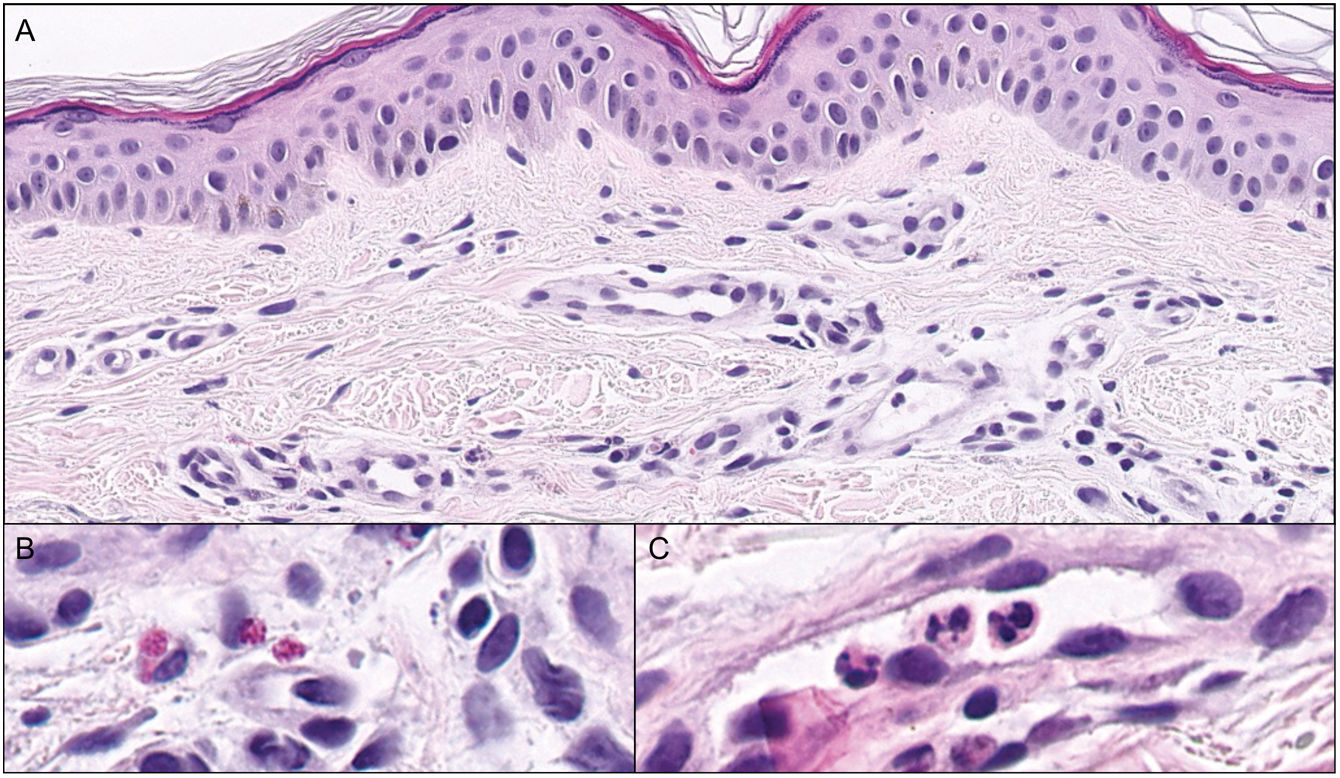
Histology of a central papule showed urticarial dermatitis with dilated capillaries in the superficial dermis, along with occasional intravascular eosinophils and neutrophils (Fig. 3). Lab test results ruled out the existence of autoimmune and thyroid abnormalities. Upon suspicion of BASCULE syndrome, blood pressure (BP) and heart rate (HR) were measured in seated and standing positions, without meeting the criteria for orthostatic intolerance.
Postural measures were recommended, and bilastine 40mg/12h was administered. Due to the persistence of the lesions, the patient discontinued pharmacological treatment. The lesions had resolved spontaneously at the 3-month follow-up
BASCULE syndrome is a vasomotor disorder first described in 2016 by Bessis et al. in 4 pediatric patients.1 It is a rare condition, with only 21 cases in the largest review by Baurens et al, all in pediatric population.2
The clinical triad begins with cyanosis, followed by the appearance of Bier spots, and finally, urticarial papules on the lower extremities, with or without upper extremity involvement, after a few minutes of standing. The most common associated symptom is pruritus, followed by pain, edema, and paresthesias. Other triggers described in children under 1 year old include defecation, crying, or manual compression.1,3–5 For our patient, we did not find a relationship with smoking cessation, although a case following SARS-CoV-2 infection has been described.5 Viruses such as SARS-CoV-2 exhibit vascular tropism, infecting both pericytes and endothelial cells, causing dysfunction and promoting increased vasoconstrictive, pro-inflammatory, and prothrombotic tone. These can damage the cutaneous microcirculation and might be involved in its pathogenesis.6 Characteristically, the clinical presentation disappears in less than 30minutes without leaving residual lesions behind upon sitting or releasing compression, except for edema, which may persist for a few days.1–3 The pathophysiology of this condition remains unclear. Bier spots and cyanosis result from excessive arterial vasoconstriction secondary to local hypoxia resulting from venous stasis and lack of a veno-arterial reflex in dermal vessels, while the mechanisms involved in the appearance of urticarial lesions remain unknown to this date.1 Baurens et al. measured serum tryptase before and after the appearance of lesions in a patient without finding significant differences, potentially excluding systemic mast cell activation as a cause. Nonetheless, its cutaneous involvement cannot be excluded.2
Diagnosis is clinical, although some authors recommend screening for autoimmune, thyroid, and vascular diseases.1,2 The histology is nonspecific, showing dilation of superficial dermal vessels and eosinophils in 30% of biopsies, as seen in our patient.1,3,7 It is important to recognize its association with various forms of chronic orthostatic intolerance, including orthostatic hypotension syndrome with or without tachycardia, initial orthostatic intolerance, and syncopal episodes. Therefore, tilt table testing is recommended even in asymptomatic patients.2,7–9 Currently, there is no effective treatment, with different regimens of high-dose antihistamines being described with variable results, along with non-pharmacological measures, such as physical exercise, abundant hydration, increased sodium intake, and compression stockings.2,8–10 However, it is a condition with a favorable prognosis, with spontaneous resolution of lesions being common.
We present the first case clinically and histologically consistent with BASCULE syndrome with adult-onset ever reported in the literature. We also highlight the possible involvement of the infectious process as a trigger. This is a underreported syndrome, with a clinical diagnosis that does not require additional tests except for orthostatic intolerance screening.
Conflicts of interestNone declared.