To the Editor:
We present the case of a 66-year-old man with a past history of ischemic heart disease, systemic hypertension, and type 2 diabetes mellitus, who consulted for the appearance 8 months earlier of multiple lesions on the left side of the scrotum. The lesions had progressively increased in number and size.
On physical examination there were numerous, sessile, erythematous-purpuric unilocular papules of vascular appearance that only affected the left side of the scrotum and did not cross the midline. In some areas the lesions grouped together to form clusters. In addition, bluish cords were observed, which indicated dilatation of superficial blood vessels (Fig. 1).
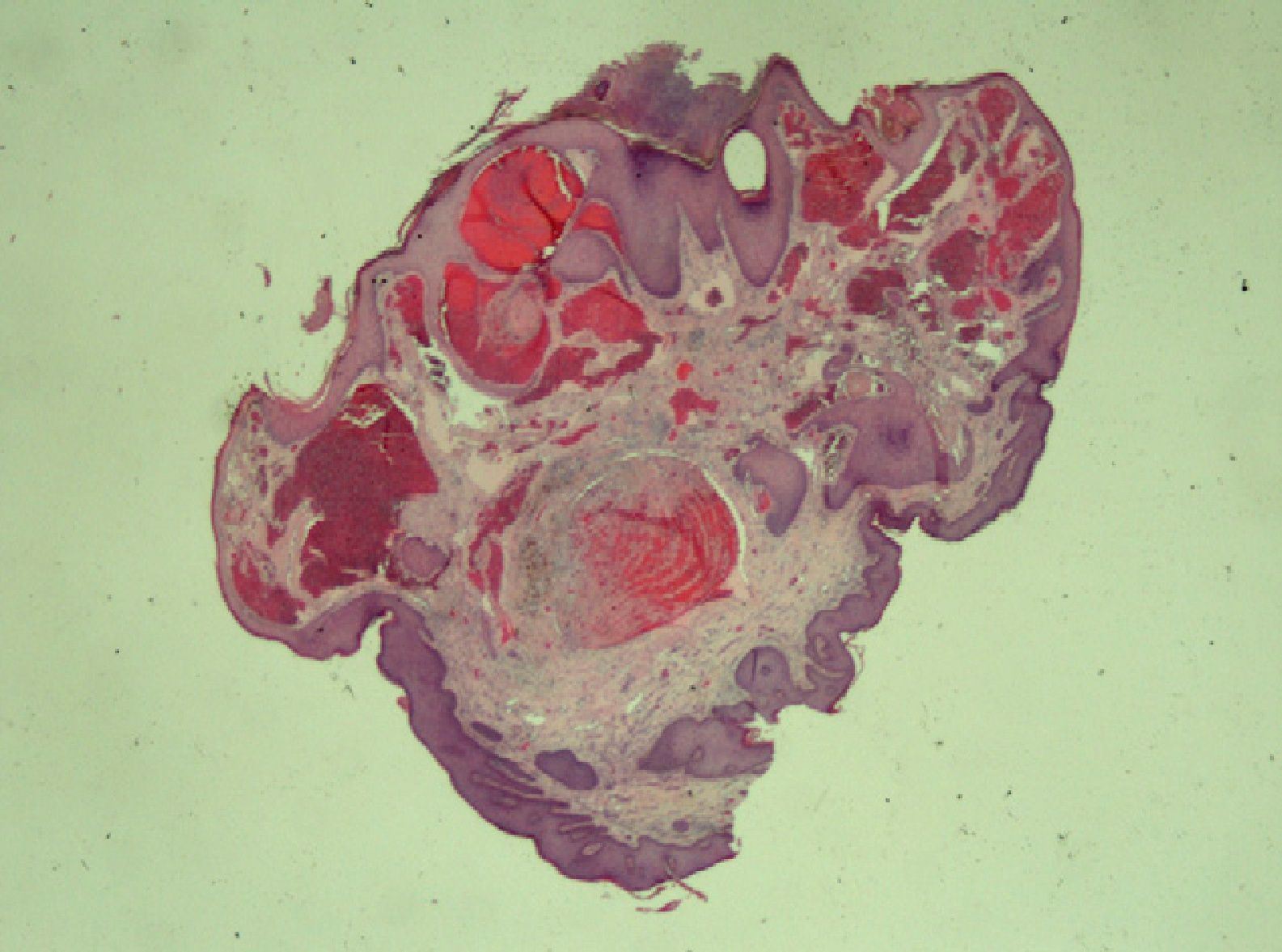
Several lesions were biopsied. All revealed the presence of dilated vascular lumens in the papillary dermis in intimate contact with the epidermis, which was hyperplastic and hyperkeratotic. There was evidence of thrombosis and recanalization of some of the blood vessels (Fig. 2).
Histological appearance of a lesion, showing a pedunculated papule with grossly dilated blood vessels. Signs of thrombosis and recanalization can be seen. Acanthosis and hyperkeratosis are present in the epidermis. Some vessels appear to be included within the epidermis. Hematoxylin-eosin, original magnification ×40.
We were able to obtain a small blood sample from the dilated scrotal vessels, which allowed us to compare the levels of cortisol in the scrotal blood with those of the general circulation. The cortisol concentration in the scrotal blood was 20.6 μg/dL, considerably higher than that of the general circulation (15.3 μg/dL; normal range, 6.2-19.4 μg/dL).
The urology department confirmed the presence of a grade II varicocele on the left side of the scrotum.
Fordyce first described this type of angiokeratoma in 1896 in a 60-year-old man with bilateral varicocele. They are the most common form of angiokeratoma. They typically arise on the scrotum bilaterally, although they have been reported at other sites, such as the vulva1 and on the body of the penis.2
The etiology and pathogenesis of scrotal angiokeratomas have not been clarified. It has been suggested that increased venous pressure could favor their appearance, and this would explain the association with varicocele.1,3 However, a study by Orvieto et al.4 found no association between varicocele and angiokeratomas. A limitation of that study was that the maximum age of inclusion was 55 years and the data were obtained by means of a questionnaire. Some authors consider that alterations of the blood vessel wall must be present for angiokeratomas to develop, though this may not be the only factor.1
Varicocele more commonly affects the left testicle. This is attributed to anatomical differences in the venous drainage of the testicles. While the right testicular vein (also known as the internal spermatic vein) follows an oblique trajectory to drain directly into the inferior vena cava, the vein from the left testicle ascends vertically to the left renal vein, which means it is 8 to 10cm longer than the vein on the right side. This leads to greater resistance to venous drainage on the left side. Varicocele is associated with testicular dysfunction, and sterility can develop due to the associated testicular hyperthermia.5 Another factor that could be important is retrograde blood flow from the left renal vein,5,6 although the results of relevant studies are contradictory.6,7
In our patient, higher cortisol levels were detected in the testicular region than in the general circulation. As the testicles do not produce cortisol, these values would support the hypothesis of retrograde flow in this patient. The suprarenal glands secrete various hormones, including estrogens and adrenomedullin, a potent vasodilator.6 Retrograde blood flow in cases of varicocele could lead to higher hormone levels in the testicles than in the general circulation; this situation would favor vascular dilatation and, thus, the appearance of angiokeratomas.
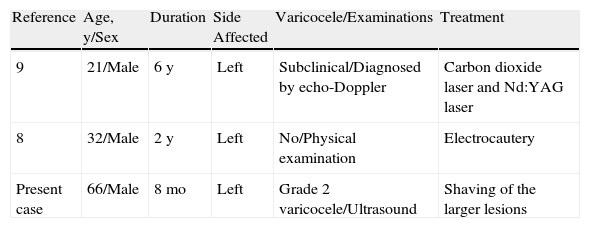
Unilateral angiokeratomas are very rare; we have only found 2 reports describing this situation.8,9 The details of those cases are shown in Table 1. Although the patient described by Pande et al.8 did not present a clinically evident varicocele, it is recognized that up to 60% of varicoceles are not detected on physical examination and require ultrasound study for diagnosis10; we cannot therefore rule out the possible presence of a subclinical varicocele.
Cases of Unilateral Angiokeratomas of Fordyce.
| Reference | Age, y/Sex | Duration | Side Affected | Varicocele/Examinations | Treatment |
| 9 | 21/Male | 6 y | Left | Subclinical/Diagnosed by echo-Doppler | Carbon dioxide laser and Nd:YAG laser |
| 8 | 32/Male | 2 y | Left | No/Physical examination | Electrocautery |
| Present case | 66/Male | 8 mo | Left | Grade 2 varicocele/Ultrasound | Shaving of the larger lesions |
Abbreviation: Nd:YAG, neodymium:yttrium aluminum garnet.
There are anastomoses between the left and right testicular circulations.5 If hormone levels do influence the development of angiokeratomas, these connections could explain the appearance of bilateral lesions, while unilateral disease may be due to abnormalities of the anastomoses. Another possible explanation would be the presence of mosaicism, which, in association with other factors such as increased pressure and high hormone levels, would cause angiokeratomas to develop only in genetically susceptible areas.
In summary, we have presented a patient with unilateral angiokeratomas of Fordyce in whom we detected higher cortisol levels in the scrotal circulation than in the systemic circulation. Studies with a larger number of patients are required to determine whether retrograde blood flow with high concentrations of suprarenal hormones could play a role in the etiology and pathogenesis of these angiokeratomas.
Please cite this article as: Piqué-Duran E, et al. Angioqueratoma de Fordyce unilateral. Actas Dermosifiliogr. 2013;104:163–4.