The patient was an 81-year-old man with a history of stage A chronic lymphocytic leukemia, ischemic heart disease, and rheumatoid arthritis for which he was taking methotrexate (7.5mg per week), prednisone, and diclofenac.
He consulted because of a painful ulcer on the scrotum that had first appeared a few weeks previously and was treated with topical silver sulfadiazine. One month later, the lesion had worsened, as had the patient's general status, with fever, dyspnea, mucocutaneous pallor, and enlarged axillary and inguinal lymph nodes.
Physical ExaminationPhysical examination revealed an ulcer on the scrotum. It measured 2×4cm and had slightly infiltrated borders and a fibrin-covered base (Fig. 1).
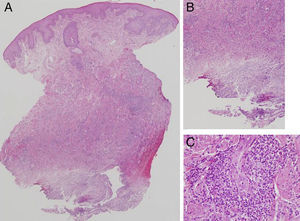
HistopathologyHistopathology of the skin biopsy specimen revealed minimal hyperkeratosis in the epidermis and, at a deeper level, an area of geographic necrosis surrounded by an intense mixed inflammatory component comprising mainly lymphocytes and monocytes with plasma cells, histiocytes, and eosinophils. No granulomatous infiltrations were observed (Fig. 2).
Additional TestsLaboratory analysis revealed pancytopenia, impaired renal function, and increased lactate dehydrogenase and C-reactive protein levels. Culture of exudates from the ulcer and tissue were negative.
What is Your Diagnosis?
DiagnosisCutaneous ulcer secondary to methotrexate.
Clinical Course and TreatmentMethotrexate was suspended, and intravenous folic acid was administered.
The complete blood count values gradually returned to normal, with progressive resolution of the ulcer. One month later, the ulcer had re-epithelialized completely (Fig. 3).
CommentMethotrexate is a synthetic analog of folic acid that is used as a chemotherapy agent and for the treatment of inflammatory diseases.1
The most common adverse reactions include gastrointestinal discomfort, joint and muscle pain, and general malaise, which are usually dose-dependent and can be attenuated with folic acid. More severe side effects, such as liver and blood disorders, can also be observed.1
Relatively common cutaneous adverse effects include stomatitis and mouth ulcers, which are usually early markers of toxicity. Other skin disorders, such as photosensitivity, exanthema, vasculitis, erythema, scaling, and toxic epidermic necrolysis,2,3 are rare and appear at high doses of methotrexate.
Skin ulcers, unlike mucosal ulcers, are an uncommon side effect2,4 that has been reported mainly in patients with psoriasis.2 They are exceptional in patients with no history of this psoriasis, and few cases have been reported in the literature.5,6 Cutaneous ulcer with pancytopenia is considered a sign of drug toxicity.5
A literature review by Pearce and Wilson7 between 1967-1996 revealed that only 17 patients had experienced this side effect.
Lawrence et al.8 divided these skin ulcers into 2 types: type I ulcers, which present as necrosis of the psoriatic plaques, and type II ulcers, which are found on skin not affected by psoriasis but by previous disorders or concurrent conditions such as stasis dermatitis.1,2 Direct toxicity seemed to be the underlying mechanism in both types.2,8
The results of the histopathology study are usually nonspecific, although there have been reports of changes resulting from epidermal dysmaturation and eccrine squamous syringometaplasia.3
The main risk factors associated with methotrexate-induced ulcers include changes in dose, concomitant therapy with nonsteroidal anti-inflammatory drugs (NSAIDs), renal failure, concomitant infections, outbreaks of pustular psoriasis, and advanced age.7 The occurrence of this and other adverse effects stresses the need for long-term follow-up in patients receiving methotrexate, even at low, stable doses. Medication, especially NSAIDs, and renal failure can boost the toxicity of methotrexate.
We report a new case of skin ulcer secondary to treatment with methotrexate accompanied by pancytopenia in a patient not diagnosed with psoriasis. The pathogenic mechanism seemed to be multifactorial, and age, lack of folic acid, NSAIDs, and renal impairment all seemed to play a role.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Arango-Duque LC, Blanco-Barrios S, Fernández-López E. Úlcera en el escroto. Actas Dermosifiliogr. 2014;105:515–516.