Treatment of mucosal vascular lesions is a challenge for dermatologists, although various approaches have proven efficacy, including surgery, sclerotherapy, intralesional injection of corticosteroids, transfixion, and laser therapy. The aim of this study was to describe the results of treatment with neodymium:yttrium-aluminum-garnet (Nd:YAG) laser in 11 patients with venous malformations and varicosities.
Patients and methodsWe describe the use of variable-pulse Nd:YAG to treat venous malformations or varicosities in the oral or genital mucosa of 8 women and 3 men seen in our hospital over a 1-year period.
ResultsThe following laser parameters were used: wavelength, 1064nm; fluence, 100 to 200J/cm2; spot diameter, 3 to 5mm; and pulse duration, 30 to 65ms. The size of the lesions ranged from 5 to 30mm. In all cases, a clearance of 75% to 100% was achieved in a single session with excellent healing and no significant side effects.
ConclusionsGiven its efficacy and ease of use, Nd:YAG may become a treatment of choice for mucosal vascular lesions. Comparative studies are now required to assess its potential superiority over other treatment options.
El tratamiento de las lesiones vasculares en las mucosas supone un reto para el dermatólogo; diversos tratamientos han probado su eficacia: cirugía, escleroterapia, inyección intralesional de corticoides, transfixión y láser. El objetivo de este trabajo es describir los resultados del tratamiento de 11 malformaciones y ectasias venosas de mucosas con láser Nd:YAG.
Pacientes y métodosPresentamos 11 pacientes, 8 mujeres y tres varones con diferentes dilataciones y malformaciones venosas en la mucosa oral y genital tratados con láser Nd:YAG de pulso variable durante un año en nuestro centro.
ResultadosLos parámetros utilizados fueron una longitud de onda de 1.064nm, una fluencia entre 100 y 200J/cm2, un tamaño de campo entre 3 y 5mm y un tiempo de pulso entre 30 y 65ms. El tamaño de las lesiones era de 5mm la menor de ellas y de 30mm la mayor. En todos ellos se produjo un aclaramiento del 75-100% de las lesiones con una sola sesión, con excelente cicatrización y sin efectos adversos significativos.
ConclusionesPara el tratamiento de lesiones vasculares en las mucosas el láser Nd:YAG se posiciona como un tratamiento de elección por su eficacia y facilidad de uso, aunque son necesarios futuros estudios comparativos que demuestren su superioridad frente a otras técnicas.
Treatment of mucosal vascular lesions is a challenge for dermatologists, yet no consensus on the technique of choice has been reached. If the lesions are large, cause functional discomfort, or bleed frequently, treatment is essential. Several options are available,1 including surgery, sclerotherapy, transfixion, intralesional injection of corticosteroids, and laser therapy, although no clear best option has been established, and few studies compare the various techniques available.1-3
Hemoglobin has absorption peaks at different wavelengths depending on oxidation state and how deep it lies in the tissue.1,2 Unlike other lasers, such as potassium titanyl phosphate (KTP) laser or pulsed dye laser, which use absorption peaks with shorter wavelengths (418, 542, and 577nm),1 the variable-pulse neodymium:yttrium-aluminum-garnet (Nd:YAG) vascular laser has a wavelength of 1064nm and uses deoxyhemoglobin absorption peaks ranging from 800nm to 1000nm.1-4 These characteristics make it an ideal choice for venous lesions, given its affinity for deoxyhemoglobin, its ability to penetrate tissue, and its minimal invasiveness; therefore, this device may prove to be the technique of choice for the treatment of mucosal vascular lesions, especially venous dilations and malformations.1,2,4,5
We present our experience using a variable-pulse Nd:YAG laser to treat 11 patients with different types of venous dilation and malformations on the oral and genital mucosa at our center over 1 year.
Patients and MethodsWe present a cross-sectional observational study of a series of 11 patients, all of whom had mucosal venous dilations and malformations. Treatment was administered from June 2008 until September 2009.
Before treatment, we took a full clinical history, which included allergy, concomitant conditions, and current treatments. No patients were receiving treatment with nonsteroidal anti-inflammatory drugs, anticoagulants, or antiplatelet agents. All patients signed an informed consent form, which explained the procedure and possible side effects.
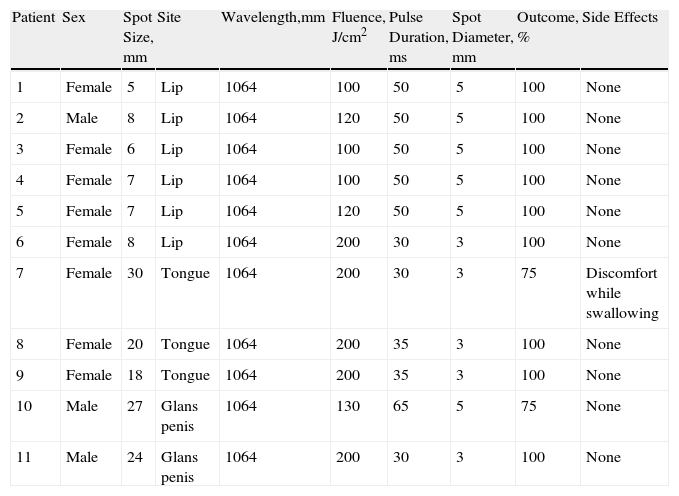
The laser used was a cooled dual system, which made it possible to apply KTP laser light (532nm) or Nd:YAG laser light (1064nm). The system comprises a sapphire crystal that serves to support the handpiece and remains at <15°C thanks to a coolant (distilled water) circulating along the laserscope (GEMINI, IRIDEX Corporation, California). We used only Nd:YAG laser light (1064nm) on our patients. The laser parameters applied were as follows: fluence, 100-200J/cm2; pulse duration, 30 to 65ms; and spot diameter, 3-5mm (Table 1).
Patients With Mucosal Venous Malformations Treated With Nd:YAG.
| Patient | Sex | Spot Size, mm | Site | Wavelength,mm | Fluence, J/cm2 | Pulse Duration, ms | Spot Diameter, mm | Outcome, % | Side Effects |
| 1 | Female | 5 | Lip | 1064 | 100 | 50 | 5 | 100 | None |
| 2 | Male | 8 | Lip | 1064 | 120 | 50 | 5 | 100 | None |
| 3 | Female | 6 | Lip | 1064 | 100 | 50 | 5 | 100 | None |
| 4 | Female | 7 | Lip | 1064 | 100 | 50 | 5 | 100 | None |
| 5 | Female | 7 | Lip | 1064 | 120 | 50 | 5 | 100 | None |
| 6 | Female | 8 | Lip | 1064 | 200 | 30 | 3 | 100 | None |
| 7 | Female | 30 | Tongue | 1064 | 200 | 30 | 3 | 75 | Discomfort while swallowing |
| 8 | Female | 20 | Tongue | 1064 | 200 | 35 | 3 | 100 | None |
| 9 | Female | 18 | Tongue | 1064 | 200 | 35 | 3 | 100 | None |
| 10 | Male | 27 | Glans penis | 1064 | 130 | 65 | 5 | 75 | None |
| 11 | Male | 24 | Glans penis | 1064 | 200 | 30 | 3 | 100 | None |
Abbreviation: Nd:YAG, neodymium:yttrium-aluminum-garnet.
The procedure was performed in the operating room. All patients received 2% mepivacaine before treatment. Slight darkening of the area was observed during the procedure, with peripheral clearing and contraction of the target tissue due to laser-induced necrosis. Patients were followed up at 24hours, 1 week, 1 month, and 6 months.
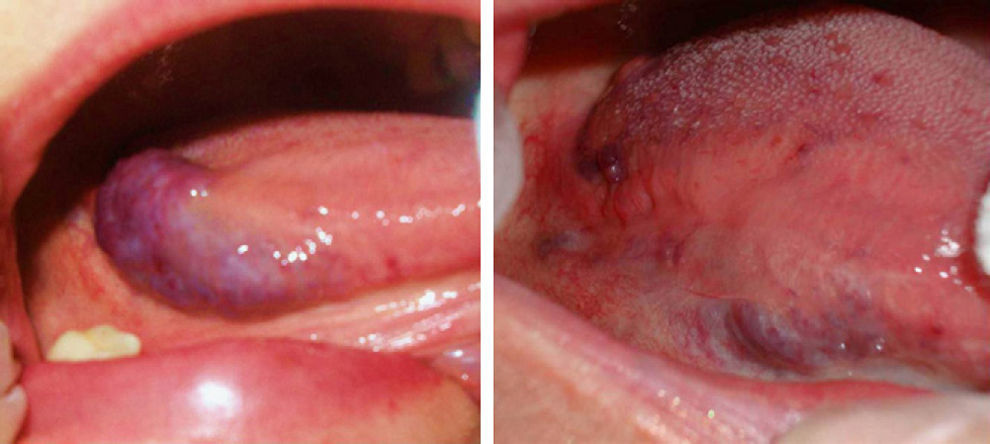
ResultsThe vascular lesions were situated on the oral or genital mucosa, as follows: 6 cases of venous ectasia on the lip, 3 venous malformations on the tongue, and 2 venous malformations on the glans penis. None of the lesions had been previously treated using other techniques. Our patients were aged 14 to 89 years (mean, 54 years; median, 62 years). The results of treatment of the vascular malformations are shown in Figs. 1-5 (patients 7 to 11 in Table 1). The size of these lesions is specified in Table 1. The vascular dilations on the lip were all less than 10mm; the venous malformations on the tongue and glans penis were larger, ranging from 18mm (smallest) (Fig. 3) to 30mm (largest) (Fig. 1).
Patients with several vascular malformations or larger malformations, such as patients 7, 8, and 11, underwent complementary tests. Patient 7 (Fig. 1) underwent Doppler ultrasound, which revealed a low-flow vascular lesion with no further abnormalities. Two of the patients with multiple lesions—patient 8 (Fig. 2) and patient 11 (Fig. 5)—underwent imaging studies. Patient 8 had vascular malformations on the tongue, thigh, and genitals. Doppler ultrasound revealed these malformations to be low-flow vascular malformations, which responded very favorably to Nd:YAG laser treatment.
Of particular interest, patient 11, who presented blue rubber bleb nevus syndrome, is in follow-up in the dermatology, pediatric, digestive, and maxillofacial surgery departments. The patient has undergone several studies—imaging, Doppler ultrasound, magnetic resonance, and endoscopy—which have shown vascular malformations involving the skin and digestive system, as well as lymphangioma on the neck and right thigh. The dual KTP and Nd:YAG laser enabled us to treat venous malformations on both the glans penis and skin lesions at other sites, with excellent results. The remaining lesions were treated with surgery, in the case of lymphangioma (with compatible histopathology findings), or with endoscopic sclerotherapy, in the case of vascular malformations of the digestive system.
The remaining patients had a single venous malformation that was diagnosed based on symptoms.
Only 1 session was necessary in all cases. The results were classified in terms of the degree of clearance of the lesion, which was assessed using symptoms and photographs and according to a consensus of 2 dermatologists. Clearance was classed as none (0%), minimal (25%), medium (50%), partial (75%), or complete (100%) (Table 1). This classification was similar to that used elsewhere to subjectively measure outcome. Clearance was greater than 75% in all cases. Clearance was complete (100%) in 9 patients (81.8%) and partial (>75%) in 2 (patient 7 [Fig. 1] and patient 4 [Fig. 4]); however, these patients did not wish to undergo further interventions, as they were satisfied with the outcome.
As for adverse effects, patient number 7 (Fig. 1), who was treated for a bulky lesion on the middle third of the tongue, had edema and inflammation in the area and secondary discomfort on swallowing. Both resolved satisfactorily after 1 week's therapy with amoxicillin-clavulanic acid and anti-inflammatory agents. No adverse effects were observed in the remaining cases, except for minimal edema that did not require treatment.
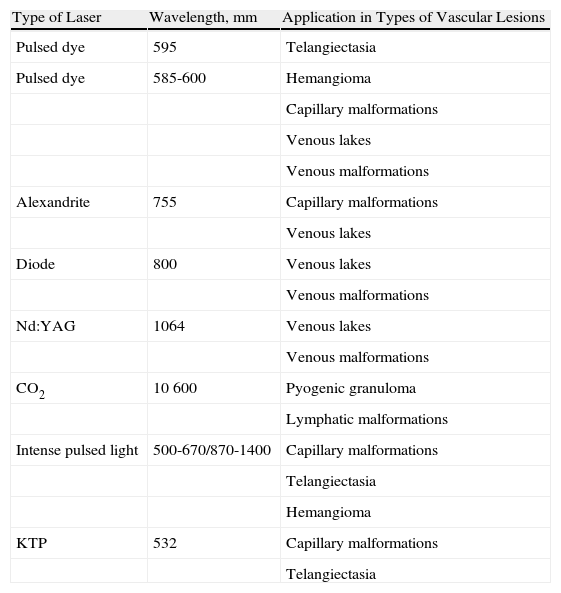
DiscussionVenous malformations are usually present from birth, although they can become clinically more evident and lead to aesthetic and functional discomfort with time. Vascular conditions can be treated with several types of laser and intense pulsed light (Table 2).1
Types of Laser for the Treatment of Different Vascular Lesions.
| Type of Laser | Wavelength, mm | Application in Types of Vascular Lesions |
| Pulsed dye | 595 | Telangiectasia |
| Pulsed dye | 585-600 | Hemangioma |
| Capillary malformations | ||
| Venous lakes | ||
| Venous malformations | ||
| Alexandrite | 755 | Capillary malformations |
| Venous lakes | ||
| Diode | 800 | Venous lakes |
| Venous malformations | ||
| Nd:YAG | 1064 | Venous lakes |
| Venous malformations | ||
| CO2 | 10 600 | Pyogenic granuloma |
| Lymphatic malformations | ||
| Intense pulsed light | 500-670/870-1400 | Capillary malformations |
| Telangiectasia | ||
| Hemangioma | ||
| KTP | 532 | Capillary malformations |
| Telangiectasia |
Adapted from Astner et al.1
Abbreviations. KTP, potassium titanyl phosphate; Nd:YAG, neodymium:yttrium-aluminum-garnet.
Given that it does not involve surgery, causes minimal discomfort, and has few side effects, laser treatment has become the approach of choice for previously untreatable vascular lesions, such as the capillary malformation port wine stain. Initially, this lesion was treated with argon or ablative lasers (eg, CO2 or erbium-doped yttrium aluminum garnet). These lasers were not very specific for the wavelengths of hemoglobin and left a permanent scar, as they had to damage the surrounding dermis in order to damage the blood vessel.5 Vascular lesions soon began to be treated using more specific approaches, such as pulsed dye laser, KTP laser, or Nd:YAG laser.6
Variable pulse Nd:YAG lasers have numerous applications in clinical practice, for example, treatment of telangiectasia and reticular veins and venules of the leg, photorejuvenation, treatment of poikiloderma of Civatte, and treatment of vascular lesions, especially low-flow and deep lesions, such as venous malformations.7
This type of laser was first used in the 1990s by maxillofacial surgeons,4,8 otorhinolaryngologists, plastic surgeons, and dermatologists2,7,9 to treat angioma, capillary malformations, and venous malformations at different sites, with favorable results. In 75% of cases, most lesions clear totally with 1 to 3 sessions.4,7-13 This procedure is gaining ground over the other, more invasive techniques used to date (surgery, transfixion,14 or sclerotherapy), which have more severe adverse effects.
All published case series report that the adverse effects with Nd:YAG lasers are minimal. In order to reduce the side effects associated with increased temperature and tissue necrosis, as well as the subsequent edema induced by this laser, the system includes a contact cooling circuit in the handpiece that maintains the temperature below 15°C throughout the procedure. Nevertheless, after treatment with Nd:YAG lasers, patients can experience edema, inflammation, or discomfort on swallowing, all of which can be managed with oral antibiotics or anti-inflammatory agents, as was the case with 1 of our patients. The larger the lesion, the greater the tissue necrosis caused by treatment and the more intense the subsequent edema; therefore, more than 1 session is sometimes necessary for the lesions to clear. It is important to bear this in mind, since the airway could be compromised in patients with venous malformations of the oral cavity.
Combinations of Nd:YAG and pulsed dye laser have also proven successful for venous malformations and dilations in the oral mucosa.11,12,15,16 This type of laser causes a shift in the absorption spectrum of oxyhemoglobin, as the pulsed dye component enables it to form methemoglobin, thus exponentially increasing absorption from the Nd:YAG laser light and producing a deep thermal effect at much lower doses.12,16 Published cases reveal the need for several sessions; however, this could be because the lesions treated were larger than those in our study.
No comparisons between the different types of laser in the treatment of mucosal vascular lesions are available to give an indication of whether one is superior to the others. Nor have any studies compared Nd:YAG laser techniques with other techniques, such as surgery or sclerotherapy.
We present a series of 11 patients with mucosal venous malformations treated with a single session of Nd:YAG laser light. The results were excellent in all cases, and no significant adverse effects were observed. Our study is subject to the limitations of observational studies and does not have a control group, thus restricting the validity of its findings.
In summary, Nd:YAG lasers are increasingly used to treat different types of low-flow (venous) vascular lesions, such as venous malformations or vascular dilations in the form of venous lakes. The treatment is fast, safe, and relatively easy to learn and does not cause bleeding. Postoperative problems and discomfort are minimal, as is potential residual scarring. Therefore, Nd:YAG lasers are the approach of choice in the treatment of mucosal vascular lesions.
Conflict of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Nuño-González A, et al. Tratamiento de malformaciones vasculares de mucosas con láser Nd:YAG de pulso variable. Actas Dermosifiliogr.2011;102:717-721.