Diagnosis of pigmented lesions can be complex. While dermoscopy has increased diagnostic accuracy for melanoma, dermatologists are commonly faced with pigmented lesions that are equivocal or difficult to evaluate. Reflectance confocal microscopy (RCM) is a noninvasive diagnostic tool comprising a low-potency coherent laser that is projected through a system of lenses, making it possible to see 2-dimensional structures in vivo with cellular-level resolution and a depth of approximately 300μm (superficial dermis). Diagnosis of melanoma using RCM is based on identification of pagetoid cells in the epidermis, atypical nests at the dermal–epidermal junction, nonedged dermal papillae, cells with atypical nuclei, neoangiogenesis, and inflammatory infiltrate in the superficial dermis.1 Two recent meta-analyses estimated that RCM would be more sensitive and specific than dermoscopy for diagnosis of melanoma.2,3
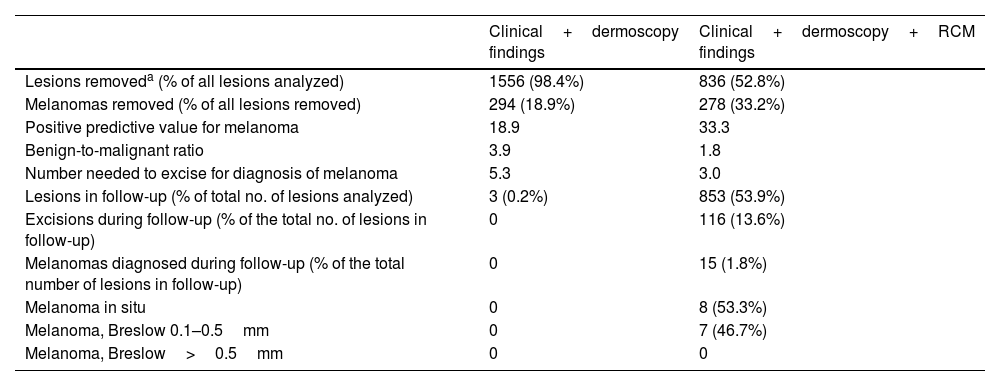
The findings from the first clinical trial of RCM to date were published in June 2022. The study population comprised 3165 patients with equivocal/unclear pigmented lesions, and mean follow-up was 9.6 months.4 Patients were randomly assigned 1:1 to clinical examination and dermoscopy with or without RCM. Depending on the findings, the authors decided to remove the lesion or follow the patient up. Compared with the non-RCM group, data for the RCM group revealed a higher positive predictive value for melanoma in the lesions removed (33.3 vs. 18.9), a lower benign-to-malignant ratio (1.8 vs. 3.7), and a 43.4% reduction in the number needed to excise for diagnosis of melanoma (3.0 vs. 5.3). None of the lesions under follow-up in the group without RCM proved to be malignant, although melanoma was detected during follow-up in 1.8% of patients in the RCM group. The Breslow depth of these tumors did not exceed 0.5mm (Table 1). The study also revealed that the medical team's experience in the use of RCM was correlated with higher diagnostic accuracy.
Comparison of Pigmented Lesions Followed Up in Groups With and Without Reflectance Confocal Microscopy.
| Clinical+dermoscopy findings | Clinical+dermoscopy+RCM findings | |
|---|---|---|
| Lesions removeda (% of all lesions analyzed) | 1556 (98.4%) | 836 (52.8%) |
| Melanomas removed (% of all lesions removed) | 294 (18.9%) | 278 (33.2%) |
| Positive predictive value for melanoma | 18.9 | 33.3 |
| Benign-to-malignant ratio | 3.9 | 1.8 |
| Number needed to excise for diagnosis of melanoma | 5.3 | 3.0 |
| Lesions in follow-up (% of total no. of lesions analyzed) | 3 (0.2%) | 853 (53.9%) |
| Excisions during follow-up (% of the total no. of lesions in follow-up) | 0 | 116 (13.6%) |
| Melanomas diagnosed during follow-up (% of the total number of lesions in follow-up) | 0 | 15 (1.8%) |
| Melanoma in situ | 0 | 8 (53.3%) |
| Melanoma, Breslow 0.1–0.5mm | 0 | 7 (46.7%) |
| Melanoma, Breslow>0.5mm | 0 | 0 |
Abbreviation: RCM, reflectance confocal microscopy.
According to these results, which constitute the highest-quality evidence available to date, incorporating RCM in the diagnostic algorithm for equivocal/unclear pigmented lesions would reduce the frequency of excision by almost half. This in turn could reduce the surgical waiting list and prioritize patients with melanoma. Furthermore, it would reduce iatrogenic effects and decrease costs. In this sense, a retrospective analysis of costs compared data from the University Hospital of Modena, where RCM is performed in the case of equivocal pigmented lesions, with data from other centers in the region that do not use RCM. With a number needed to excise of 6.25 vs. 19.41, respectively, the estimated saving was approximately €262000 per million persons per year with RCM when indirect costs were excluded.5 However, it is important to consider the false negatives generated by RCM, which delayed excision of 15 melanomas in the clinical trial, although none was higher than stage IA. The difference in the proportion of lesions analyzed using histology between both groups could lead to information bias and underdiagnosis of melanomas, especially in the RCM group. Therefore, affected patients should be regularly assessed and clinical studies with long follow-up periods should be performed to evaluate the impact on survival.
RCM complements dermoscopy, thus increasing diagnostic accuracy in melanoma and potentially reducing costs. However, the technique is limited in terms of its availability and generation of false negatives.