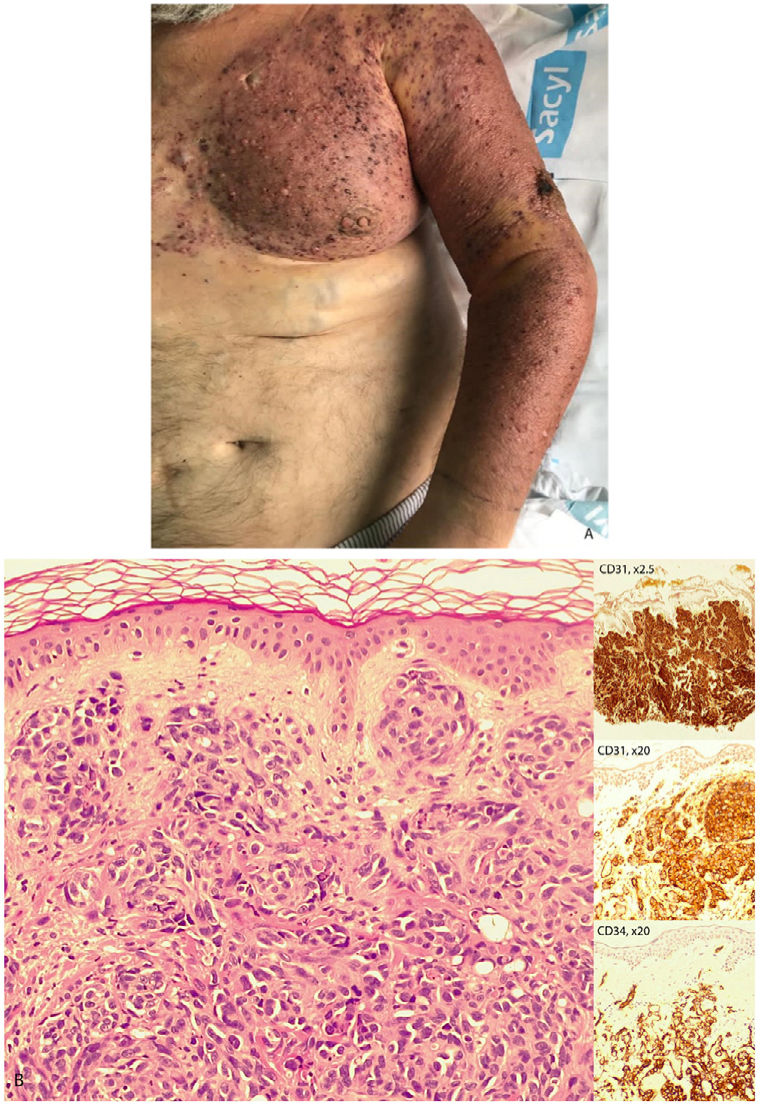
A 58-year-old man, with a seven-year history of chronic lymphedema in the left upper limb secondary to the obstruction of the vascular access for hemodialysis, presented to the Emergency Department with an exacerbation of the edema accompanied by pain, without any other clinical symptoms. The arm was indurated, warm, and exhibited numerous infiltrated erythematous-violaceous papules and plaques (Fig. 1A). Analytically, there was a slight elevation in acute phase reactants. Following an ultrasound, he was hospitalized for suspected bacterial cellulitis. In the absence of response to antibiotic treatment, he was evaluated by the dermatologist, who performed a skin biopsy suspecting a cutaneous angiosarcoma. The histological examination (Fig. 1B, hematoxylin-eosin, ×20) revealed an infiltrative malignant neoplasm, positive for vimentin, CD31 (inset), and CD34 (inset), and negative for cytokeratins, confirming the diagnosis.
Cutaneous angiosarcoma associated with chronic lymphedema is a well-documented entity in the context of breast cancer (Stewart-Treves syndrome). However, its association with other etiologies causing lymphedema is less known, which contributes to diagnostic delay. The case we describe underscores this issue, as the initial diagnostic approach was oriented towards more common complications in hemodialysis patients, such as vascular or infectious diseases. The role of the dermatologist is noteworthy, who, in the face of clinical suspicion, should perform an early skin biopsy.