Tufted angiomas are relatively rare benign vascular proliferations, which were previously referred to as progressive capilliary hemangiomas or angioblastomas.1 They appear mainly in patients under 5 years of age, although adult-onset cases have been reported. They present as erythematous-violaceous plaques or nodules affecting the upper trunk and limbs or the neck. Histologic examination is necessary to establish a definitive diagnosis.2 We report the cases of 3 adults with tufted angiomas diagnosed in our hospital in the past 20 years, highlighting the usefulness of topical rapamycin in one case.
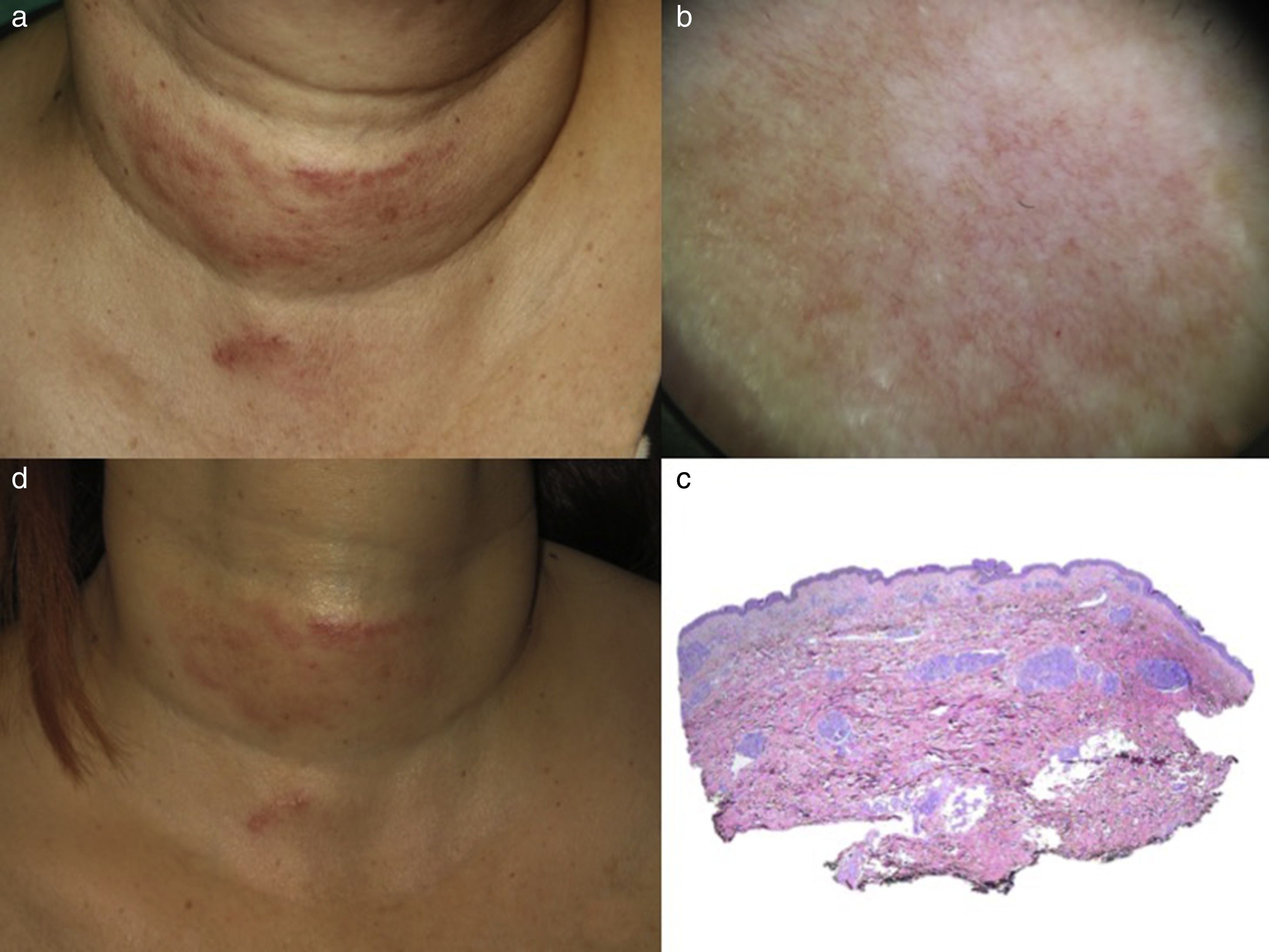
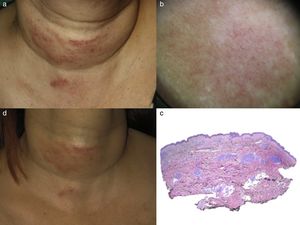
Case ReportsThe first patient was a 51-year-old woman with no past medical history of interest, who presented with a lesion that was vascular in appearance. She reported onset some 9 years earlier. Initially the lesion had been asymptomatic, but in the 6 months before the consultation it had grown and become painful. The clinical presentation was a mottled, erythematous lesion on the front and right side of the neck, characterized by superficial telangiectasias. The slightly indurated lesion was about 7cm wide and we detected no thrill or increase in temperature (Fig. 1A). Dermoscopy revealed an erythematous reticular pattern (Fig. 1B). Histologic examination showed a proliferation of vessels grouped into lobules distributed throughout the reticular dermis in a cannonball pattern (Fig. 1C). These findings led to a diagnosis of tufted angioma. As the lesion was painful, treatment with rapamycin 0.4% was started using a topical preparation comprising rapamycin powder in a cream base. After 5 months of treatment, the lesion was no longer palpable, the coloration had diminished (Fig. 1D), and the patient reported no pain.
A, Clinical image. Erythematous plaque, vascular in appearance, on the anterior region of the neck. B, Dermoscopic image showing an erythematous reticular pattern. C, Groups of vessels forming several lobes distributed in a canonball pattern throughout the reticular dermis (hematoxylin-eosin, original magnification ×2). D, Reduced erythema and infiltration following 5 months of treatment with topical rapamycin.
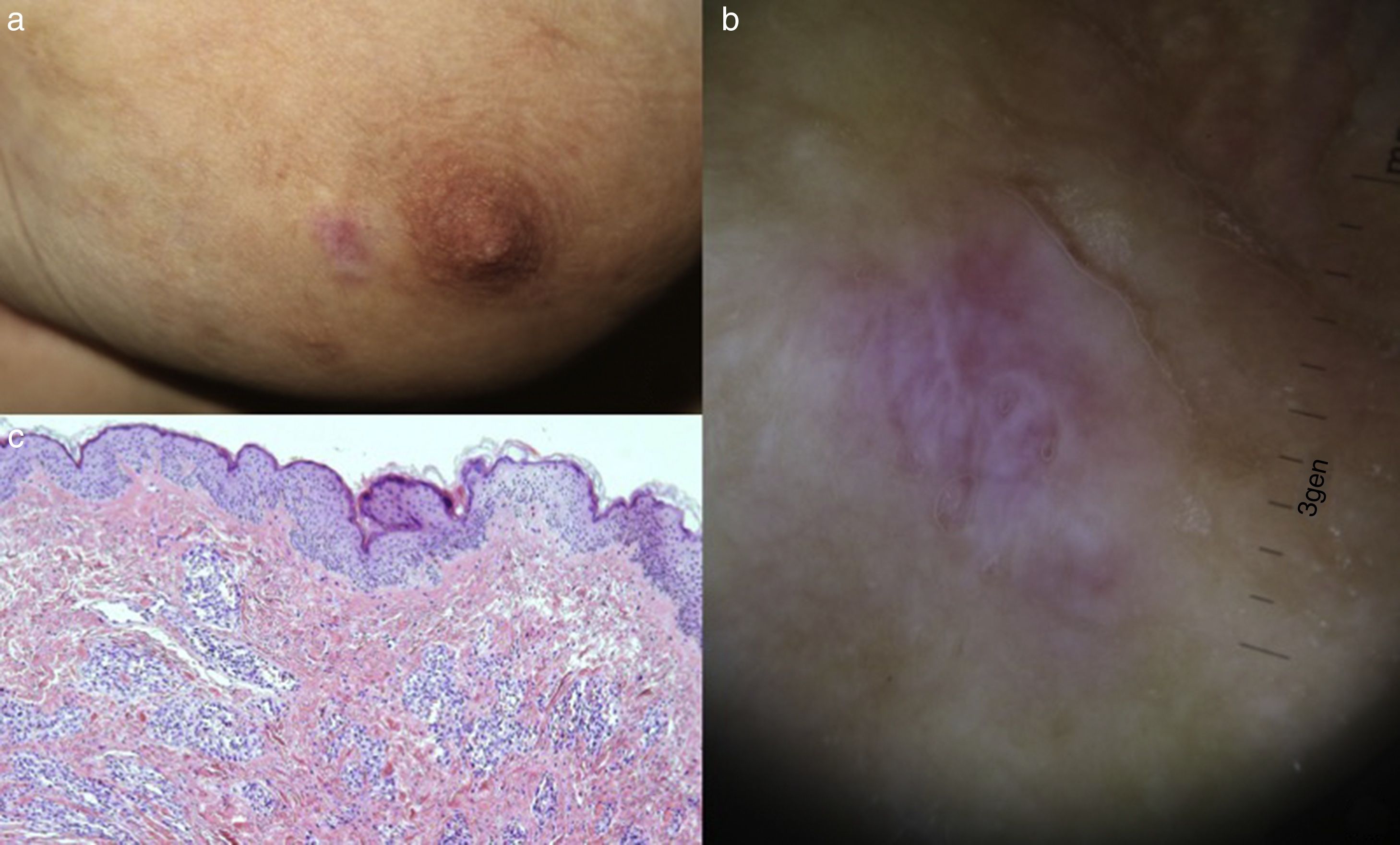
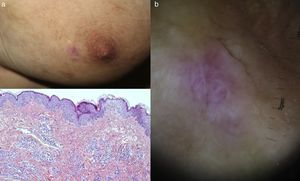
The second patient was a 24-year-old woman with a history of familial Mediterranean fever, who presented with an erythematous-violaceous macular lesion 2cm in diameter, which had first appeared 11 years earlier (Figs. 2A and B). The asymptomatic lesion was located on the left breast. Histologic examination showed clusters of endothelial cells in the reticular dermis, forming lobules that protruded into dilated, thin-walled vascular channels, forming slit-like spaces (Fig. 2C). These findings confirmed the diagnosis of tufted angioma. Given the absence of symptoms, no treatment was prescribed.
A, Erythematous-violaceous macular lesion on the left breast. B, Dermoscopic image showing a pattern of white lines on a pink background. C, Histological image showing endothelial cells grouped into several lobules, which protrude into dilated, thin-walled channels forming slit-like spaces (hematoxylin-eosin, original magnification ×10).
The third patient was a 66-year-old man who presented 17 years ago with a verrucous lesion measuring approximately 2cm in diameter on the anterior face of his right hand. The lesion had appeared some months earlier and bled frequently. Complete surgical excision of the tumor was performed. The diagnosis of tufted angioma was reached on the basis of the symptoms and the histologic findings.
Cases of tufted angioma in adults are very rare, with fewer than 50 cases reported in the literature, of which only one was associated with Kassabach-Merritt phenomenon.3 In general, these tumors are characterized by slow and gradual growth followed by stabilization. Spontaneous regression has also been reported. No differences have been reported between adults and children in the presentation. The morbidity of these lesions is mainly related to the pain caused by the tumor, as was the case in our first patient.
Tufted angioma and kaposiform hemangioendothelioma share certain clinical and histopathologic features and it is thought that the two entities may represent the opposite poles of a spectrum of vascular lesions.4 They also share a common complication known as Kasabach-Merritt syndrome: consumptive coagulopathy with severe thrombocytopenia. This syndrome is rare in adults. The characteristic histologic feature of tufted angioma is the presence of lobular clusters of capillaries forming tufts within the dermis. The differential diagnosis includes several other vascular anomalies.1
Complicated tufted angioma in childhood is treated systemically with vincristine, ticlopidine, and acetylsalicylic acid5; recently, rapamycin has emerged as a very effective alternative.6,7 In uncomplicated cases, Javvaji et al.8 report good results with low dose aspirin. Clinical management in adults is not well established, and the evidence does not support any definite conclusions as to what the first-line therapy should be. The treatment options described in the literature, with variable results, include pulsed dye laser, topical corticosteroids, intralesional interferon-alfa, surgery, and a watch-and-wait approach.3
Of our 3 cases, one was resolved with surgery, another is being followed up, and the third—a painful neck lesion—improved after topical treatment with 0.4% rapamycin ointment.
Oral rapamycin has become the treatment of choice for complicated tufted angioma in children.6,7 There has been no experience to date of the use of topical rapamycin in the treatment of this type of tumor. However, in view of the demonstrated efficacy of rapamycin in the treatment of facial angiofibromas in tuberous sclerosis,8,9 and in isolated cases of lymphatic malformation, we suggest that topical rapamycin may be another option for the treatment of symptomatic tufted hemangioma not associated with coagulopathy.
Conflict of interestsThe authors declare that they have no conflicts of interest.
Please cite this article as: Escudero-Góngora MM, Corral-Magaña O, Gómez C, Martín-Santiago A. Rapamicina tópica: otra opción terapéutica del angioma en penacho en el adulto. Actas Dermosifiliogr. 2018;109:192–194.