Mycosis fungoides (MF), the most common cutaneous T-cell lymphoma, has a different clinical presentation than most malignant skin tumors. Because of its clinical similarity in the early stages to some inflammatory diseases, such as psoriasis and the eczemas with which it is often confused, it is difficult to include MF in the classic tumor-node-metastasis-blood (TNMB) classification system.1 One of the main problems with applying TNMB staging to MF is the objective assessment of the body surface area (BSA) involved: in the early stages, the classification only considers whether the lesions cover <10% (T1) or>10% (T2) of the total BSA; consequently, differences between patients with lesions on 20% of the body and those with lesions on 90%-100% of the body are not reflected in the classification. Similarly, it is difficult to assess the impact of a particular treatment on the course of the disease and/or a possible change of stage because the type and number of skin lesions, plaques, and tumors are not reflected in the current TNMB system.
In clinical practice, physicians assess changes not only in the extent of disease but also in the type of individual lesions and the total BSA involved. There is a tool for this purpose that is not well known to those unfamiliar with the field of cutaneous lymphomas. This tool, known as the Severity-Weighted Assessment Tool (SWAT), uses a continuous scale like that of the Psoriasis Area and Severity Index (PASI) and the Eczema Area and Severity Index (EASI), facilitating a precise assessment of area of skin involvement by type of lesion.2
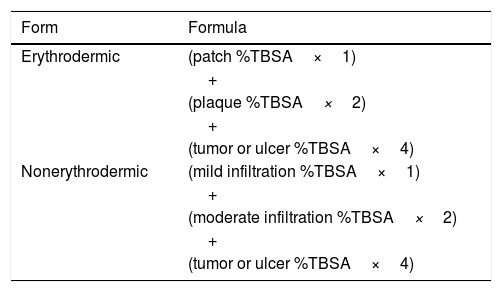
The SWAT, first proposed by Stevens et al.2 in 2002, takes into account the percentage of total body surface area (%TBSA) affected by each type of lesion (patch, plaque, tumor, or ulcer), thus providing a defined, objective, and sensitive measurement of possible changes in the course of the disease in patients diagnosed with MF. The SWAT was subsequently modified (mSWAT)3,4 to give higher scores for tumors and to differentiate between erythrodermic and nonerythrodermic disease (Table 1). The European Organization for Research and Treatment of Cancer (EORTC) has recommended the mSWAT as the first-line method for calculating cutaneous involvement in patients diagnosed with MF and Sézary syndrome.4
The application of this index makes it possible to assign patients a numerical value for the purposes of assessing treatment responses, carrying out comparative studies, and monitoring clinical trials in a quantitative manner, although it is true that the index does not eliminate intraobserver and interobserver variability.4 Despite being an excellent tool that makes it possible to quantify cutaneous involvement in patients with MF, it is not included in the staging system and its prognostic implications have not been demonstrated (although a poor prognosis can be inferred from a high mSWAT score).
A free mobile application called Cutaneous Lymphoma Resource Tools allows clinicians to quickly estimate a patient's mSWAT score during a consultation. Along with the patient's TNMB status, the mSWAT score should be added to the clinical record at each visit to improve follow-up.
Please cite this article as: Combalia A, Estrach T. FR-mSWAT: el «PASI/EASI» de la micosis fungoides. Actas Dermosifiliogr. 2018;109:745–746.