Blue nevus is a benign pigmented melanic lesion formed of intensely pigmented dendritic melanocytes located in the dermis. It is included in the group of dermal dendritic melanocytic proliferations, characterized by the presence, at least in part, of oval or spindle-shaped cells and dendritic cells.1,2 The clearly visible, characteristic bluish color is produced by a Tyndall effect, due to the reflection of blue light by melanin in the dermis.1 The lesion may be congenital or acquired, and a number of clinical and histological variants exist, the most frequent being the common and cellular variants.1,2 We present a patient with a common blue nevus at a unusual site.
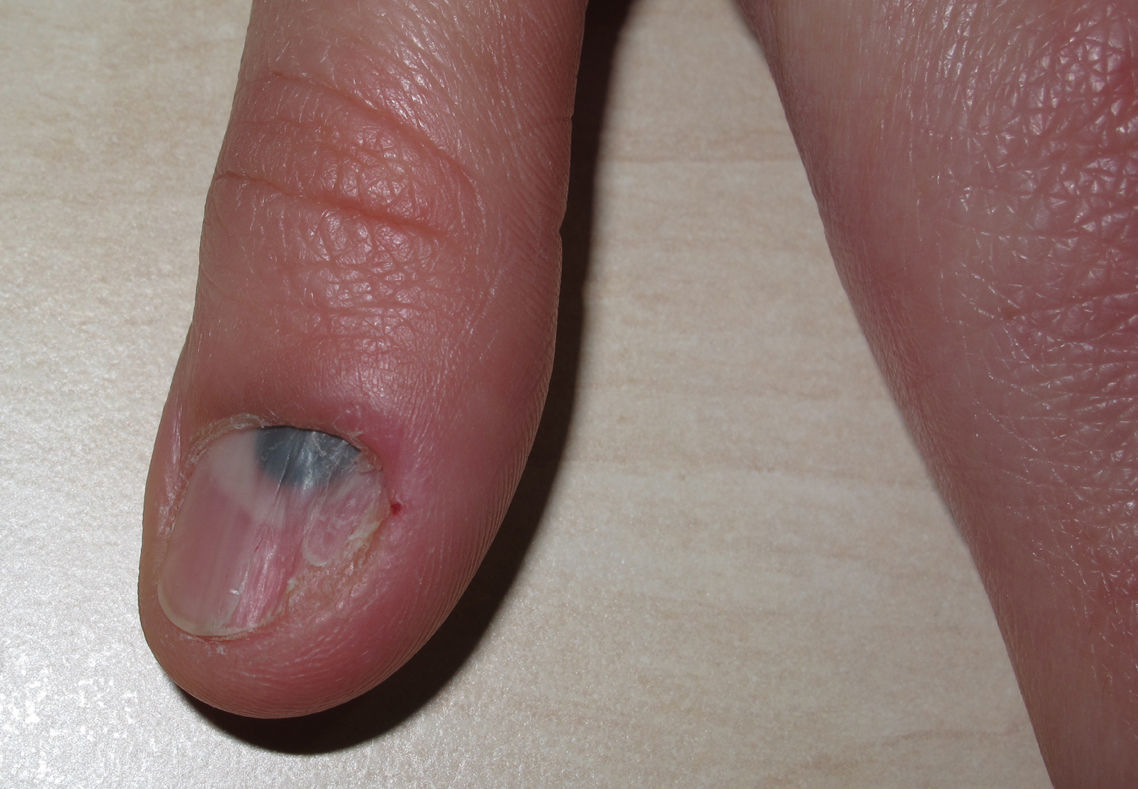
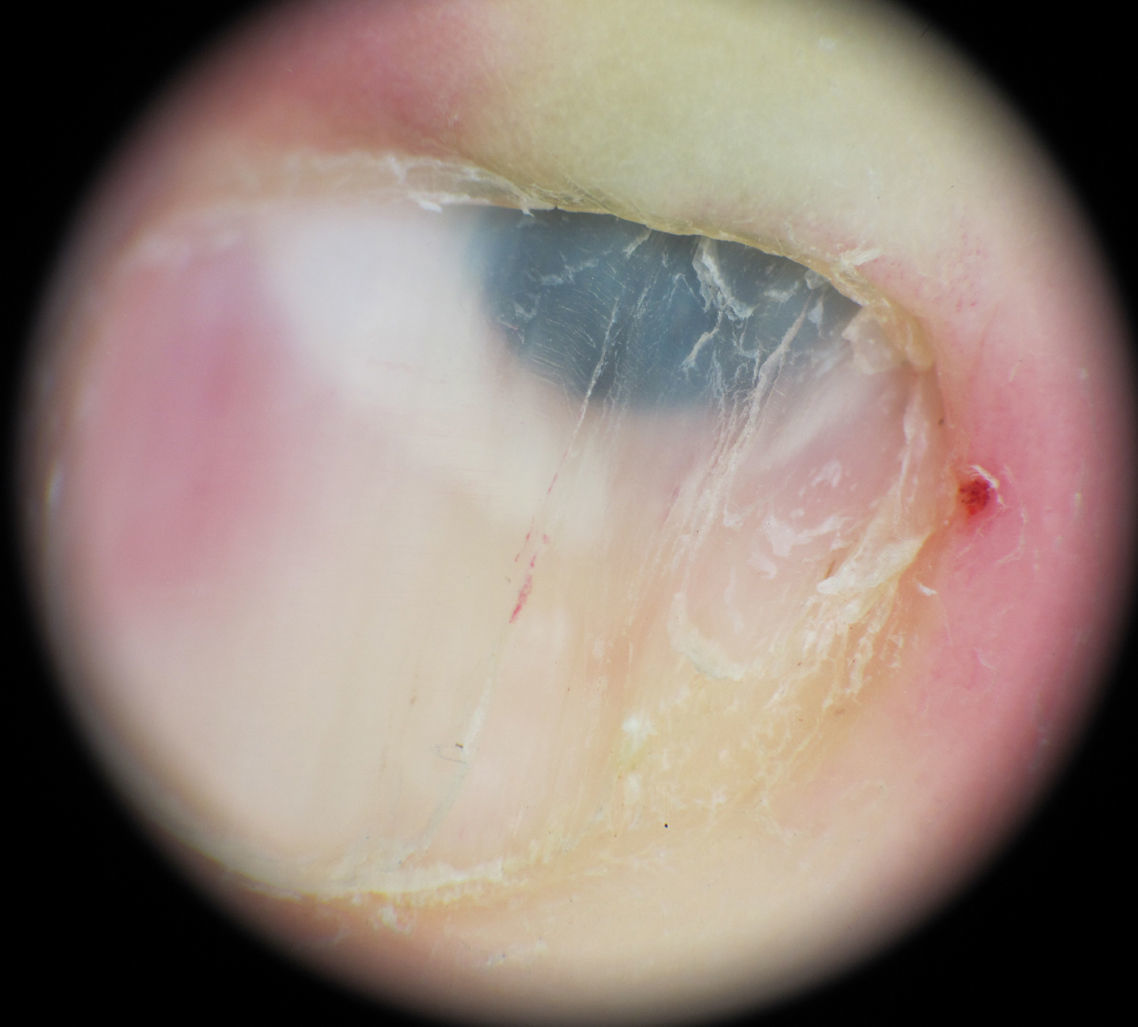
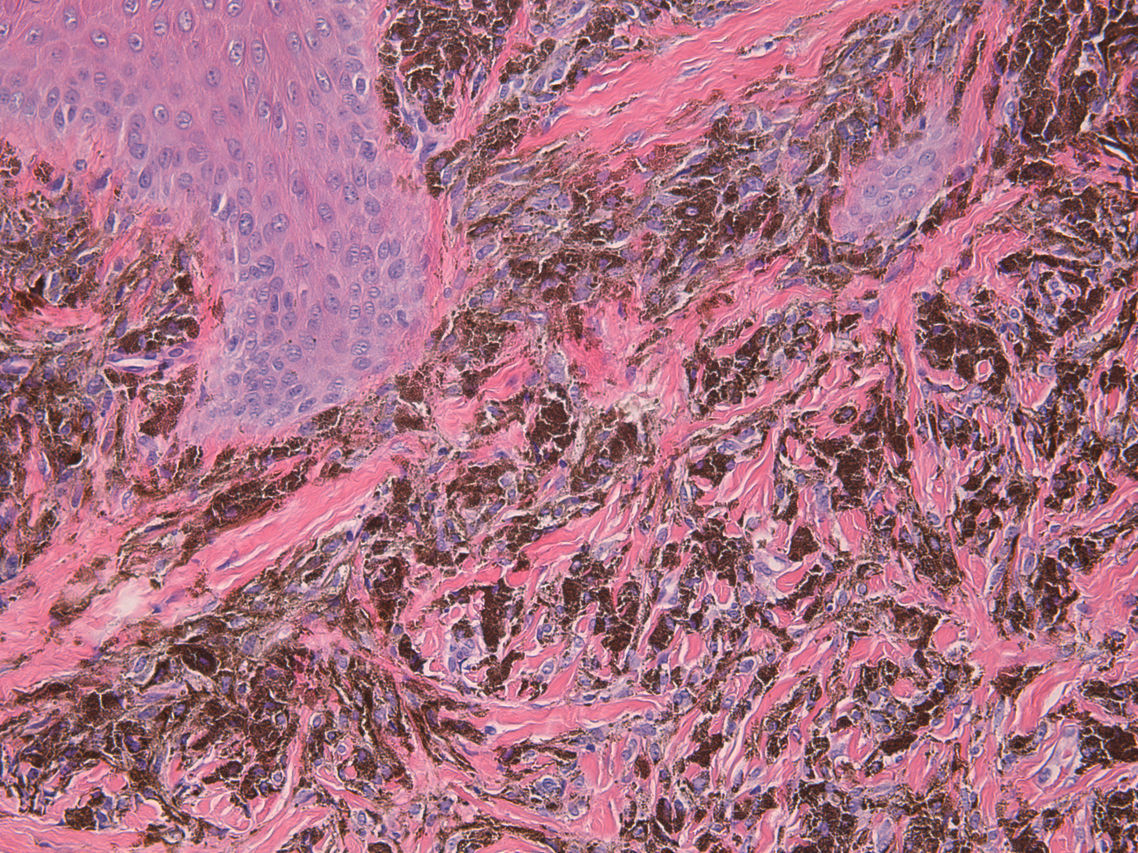
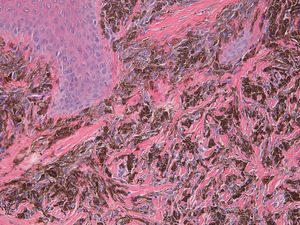
A woman aged 35 years was seen for evaluation of a dark spot that had been present under the nail of the first finger of her left hand for approximately 5 years. Examination revealed a semicircular, dark-blue macule of 5mm in diameter in the proximal subungual region. Canaliform dystrophy was present across the mid segment of the nail, with dystrophy and fragility of the left border. Hutchinson sign was not observed (Fig. 1). On dermoscopy, a circumscribed, steel-blue colored area with a homogeneous blue pattern was observed, with no other specific dermoscopic structures (Fig. 2). The lesion was excised and histology revealed irregular epidermal hyperplasia with no increase in melanocytes in the basal layer; a proliferation of irregularly arranged, spindle-shaped melanic cells separated by broad bands of dense collagen was present in the papillary and reticular dermis, and abundant melanophages were observed. The melanic cells presented an intensely pigmented cytoplasm that sometimes obscured the nuclear morphology. The nuclei were round, with small or absent nucleoli, with no atypia or mitoses (Fig. 3).
Common blue nevus is a benign neoplasm characterized by a proliferation of elongated, spindle-shaped bipolar cells in the dermis or submucosa. The melanocytes present dendritic projections with a variable melanin content. Abundant melanophages are present between the collagen bundles. No cellular atypia or mitoses are observed.1 These lesions can arise on any area of the body surface, most frequently on the limbs or face and more rarely at other sites, such as the oral mucosa, conjunctiva, mucosa of the nose and paranasal sinuses, bronchi, esophagus, stomach, vagina, uterus, penis, prostate, or lymph nodes.1
The first description of a subungual blue nevus with its histological findings was published by Vidal et al.3 Nine more cases have been published since that time.4,5 No characteristic pattern has yet been defined, as congenital and acquired lesions have been described on the fingers and toes, on the first or other digits, of the common or cellular variants, with or without longitudinal melanonychia, with or without Hutchinson sign, and stable or showing progressive growth. Seven of the nevi were observed in women and 3 in men. In some cases, the nevus provoked changes in the nail plate, such as clubbing6 or linear erosions.7 We have now described the eleventh case. Our patient was also a woman, and the nevus was an acquired lesion present on the first finger of her left hand, stable in time, with no Hutchinson sign, and no melanonychia striata, but with longitudinal canaliform dystrophy and lateral fragility of the nail plate; histologically, the lesion was the common variant of blue nevus.
Although the clinical and pathological findings made diagnosis simple in this case, the rarity of blue nevus at this site can lead to diagnostic error, as melanoma is more common in the subungual region, accounting for 0.7% to 3.5% of all melanomas.8 This diagnostic confusion is more likely in those cases in which the blue color is clinically or dermoscopically less clear, as blue nevi have been described as bluish-white, black, brown, or polychromatic.2 Furthermore, melanoma can be difficult to diagnose when it has no pronounced epidermal component, with atypical melanocytes scattered through the epidermis and abundant melanophages in the dermis. If, in addition, the malignant component regresses, only an intense bluish or grayish dermal pigmentation may persist, which could lead to an erroneous diagnosis of blue nevus. Yang et al.9 published 2 cases of subungual melanoma in which the histopathological findings were indistinguishable from blue nevus, but which, after identification of lymph-node metastases, were reinterpreted as subungual melanoma with regression. In these situations, we should remember the rule proposed by Levit et al.8 to aid diagnosis of subungual melanoma, similar to the well-known ABCDE rule: A for age (most common between the fifth and seventh decades of life) and race (Asian and black or native American), B for band (brown-black melanonychia broader than 3mm, with irregular borders), C for changes (rapid changes in size, or dystrophy), D for digit (1digit more suspicious than several), E for extension (in reference to Hutchinson sign), and F for family (relating to a family or personal history of melanoma or dysplastic nevus).
In conclusion, although subungual blue nevus is very rare, it should always be taken into account to avoid diagnostic error that could lead to irreparable clinical consequences for the patient.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fachal C, Pérez-Pérez LC, Allegue F, Calviño S. Nevus azul subungueal. Actas Dermosifiliogr. 2018;109:88–90.