A 31-year-old woman, with skin phototype IV and no relevant personal history, presented in our clinic with a painful progressively growing lesion that first appeared 1 year earlier.
Physical ExaminationOf note in the physical examination was the presence of a well-defined subcutaneous mass measuring 3×2.5cm (Figure 1). The lesion was of stony-hard consistency and infiltrated down to deep layers.
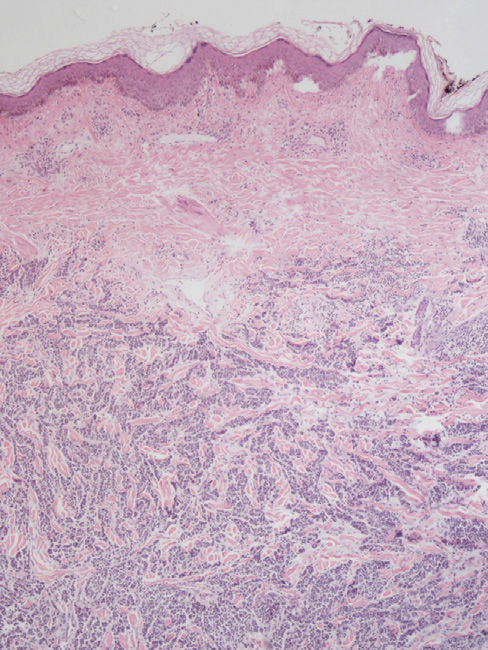
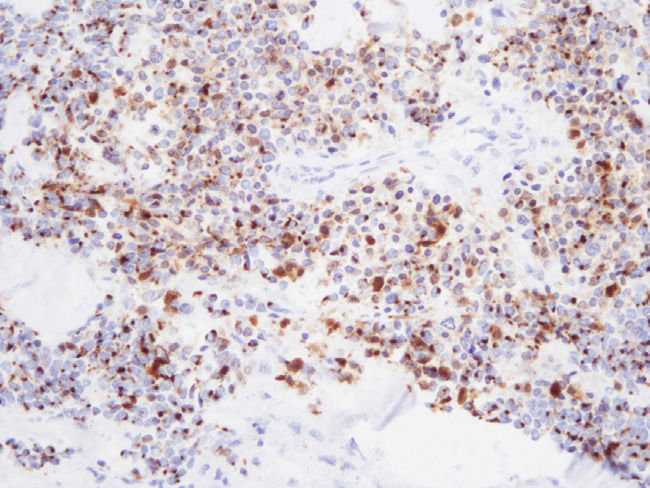
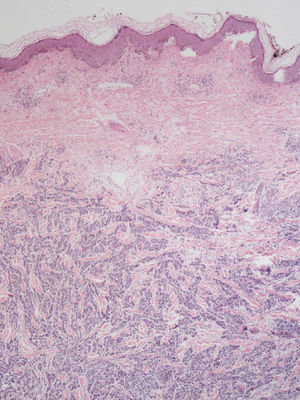
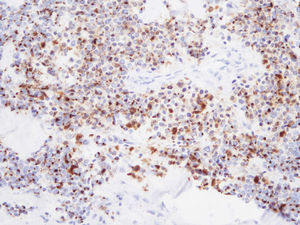
HistopathologyBiopsy was performed and sections were obtained for hematoxylin-eosin staining and immunohistochemical (IHC) staining. Infiltration of the deep dermis and the subcutaneous cell tissue by small, uniform, cells was observed. These cells were arranged in a trabecular structure between a myxoid stroma (Figure 2). At higher magnification, a vesicular nucleus was observed in these cells with a high mitotic index. Large areas of necrosis were observed with abundant apoptotic bodies. IHC study was positive for cytokeratin 20 (CK20) (Figure 3), chromogranin, synaptophysin, and CD56. Focal positivity for myogenin and desmin was also observed.
Additional TestsMagnetic resonance imaging was performed and involvement of the deep layers was ruled out. An oncologic positron emission tomography-computed tomography scan did not detect any evidence of disease spread.
¿What was the diagnosis?
DiagnosisMerkel cell carcinoma (MCC) with rhabdomyoblastic differentiation.
Course and TreatmentThe lesions were completely excised with safety margins. Ipsilateral lymph node dissection was performed. Radiotherapy of the tumor bed and adjuvant chemotherapy were also administered. The patient is currently free of disease 1 year after diagnosis.
CommentMCC is an uncommon primary neuroendocrine carcinoma. It usually appears in patients with a low phototype, elderly patients, immunodepressed patients, and on sun-exposed areas, although it has also been reported at sites such as the crotch or the buttocks.1,2 The most typical presentation is in the form of a rapidly-growing firm nodule with a red-violaceous color, but cases have also been reported with lesions in the form of panniculitis-like subcutaneous plaque.1,2 Aberrant differentiation of MCC is uncommon. The documented subtypes are eccrine, squamous, rhabdomyoblastic, sarcomatous, and leiomyosarcomatous.3
In the pathology study, MCC with rhabdomyoblastic differentiation presents as a small cell tumor that infiltrates down to the subcutaneous tissue. IHC study of the tumor shows results characteristic of neuroendocrine tumors consistent with MCC (QAE 1/2, CK20, chromogranin, synaptophysin, and CD56 positivity), but focal positivity for myogenin and desmin is also present, thus showing the presence of rhabdomyoblastic differentiation.3 The immunophenotype enables differential diagnosis to be established with other types of tumor such as primary cutaneous Ewing sarcoma (negative for CK20, chromogranin, and synaptophysin stains). Although the sarcoma always shows positivity for CD99, it should be remembered that up to 30% of MCC are also positive. Alveolar rhabdomyosarcoma (negative for CK, synaptophysin, and chromogranin), metastasis of small cell lung cancer (negative for CK20 and positive for TFF-1), and malignant amelanotic melanoma with rhabdomyoblastic differentiation (positive for stains characteristic of melanoma) should also be included in the differential diagnosis.4,5
Currently, there is discussion about the association between MCC and Merkel cell polyomavirus (MCP). In 2008, Feng et al. isolated MCP in 8 of 10 samples from patients with typical MCC. However, in 2013, Martin et al.6 presented a series of 12 patients with MCC with divergent differentiation in which MCP was not isolated in any samples, bringing into question the association, at least in MCC with divergent differentiation. In our case, the determination for MCP was also negative.
Treatment consists of excision with safety margins, lymph node dissection, and radiotherapy and chemotherapy. The general prognosis for MCC is poor, with 70% survival at 5 years. This survival rate is lower still for aberrant types.
In conclusion, we present the first case in an immunocompetent patient, with no evidence of actinic damage, who developed MCC with rhabdomyoblastic differentiation and who was negative for MCP.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Agut-Busquet E, Yébenes M, Luelmo J. Masa subcutánea pétrea en el brazo de una mujer joven. Actas Dermosifiliogr. 2016;107:149–150.