Glomus tumors of the skin are neoplasms derived from dermal glomus cells. These are modified smooth muscle cells and form part of the glomus body, a neuromyoarterial structure that serves to regulate blood flow to the skin.1 These tumors are usually classified according to the predominant cell type or vessels. Thus, tumors are denoted glomus tumors when there is high cellularity, the most frequent variety; glomangiomas when a vascular pattern predominates; and glomangiomyoma if abundant smooth muscle is present.2,3 Generally, solid glomus tumors are painful acquired nodules, whereas glomangiomas usually present as multiple lesions and are congenital or onset occurs at a young age. Not infrequently, they may be hereditary, and so are considered as a different entity. They are denoted glomuvenous malformations and a relation to a mutation on chromosome 1p21-22 has been found,4 in a gene that encodes glomulin.5 We report the case of a solitary glomus tumor with a distinctive clinical presentation, in form of a telangiectatic macule.
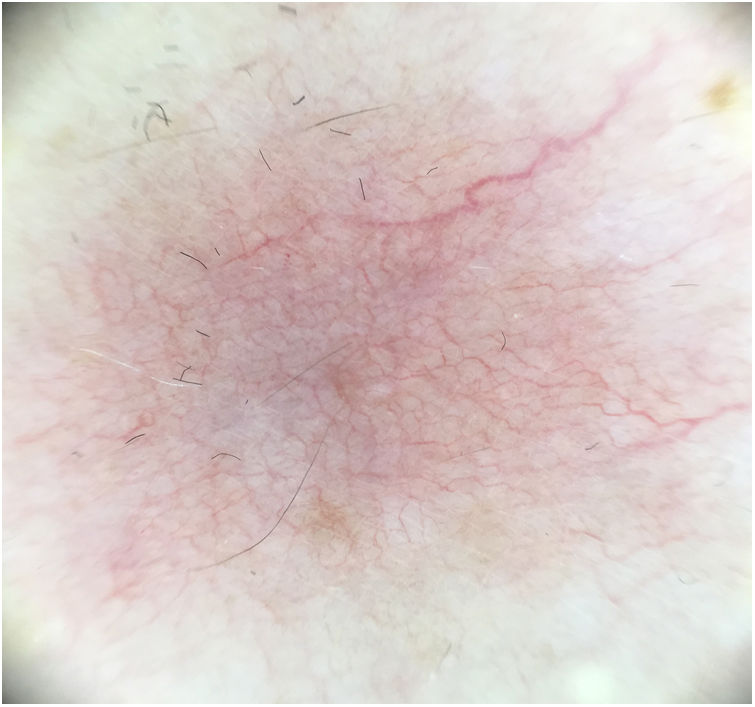
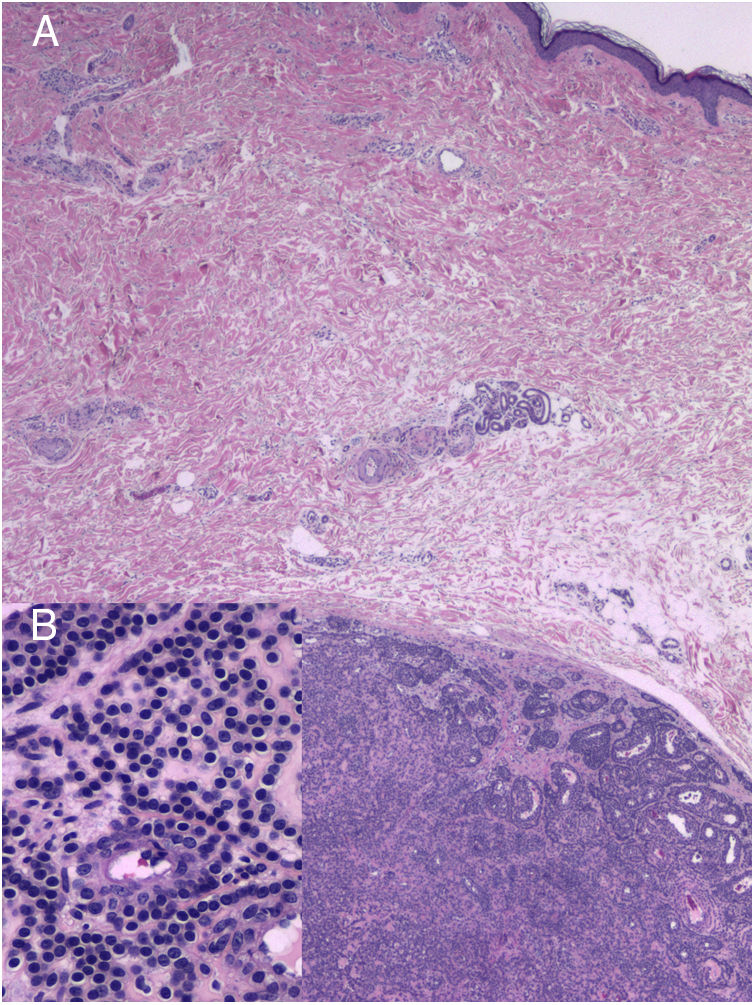
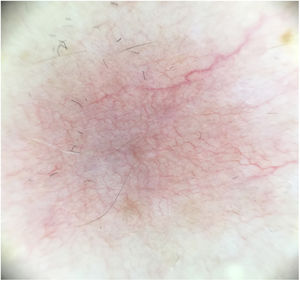
A 60-year-old woman with no medical history of interest was assessed for a painful lesion on the internal face of the left thigh. The lesion had been present for 2 years and had appeared spontaneously, with no apparent relationship with prior trauma. The patient reported pain on touch and pressure, but not spontaneously or with changes in temperature. She did not report any similar lesions in family members. Examination showed a macule with telangiectatic appearance, measuring 1.5cm in diameter, which was painful to palpation, and no other indications of dermal or epidermal involvement (Fig. 1). Dermatoscopy showed a small blue-grey poorly delimited structure immersed in an extensive fine network with a reticular configuration (Fig. 2). The lesion was resected, and histopathological study showed a solid, well-delimited nodule, measuring 6mm, located in the hypodermis, formed of monomorphic, rounded cells with oval nuclei, without atypia, that surrounded dilated vessels with thin walls. The cells expressed actin in smooth muscle and endothelial markers in vessels. In the papillary dermis, vessels were observed with dilated lumens, but without glomus cells nearby (Fig. 3). The diagnosis was of a solitary glomus tumor.
Solitary glomus tumor, given its origin in the glomus body, can appear anywhere on the skin, but it is much more frequent at sites where these structures are more numerous, that is, fingers and particularly the subungual region. They have also been reported ectopically in internal organs, where normally these structures do not appear. Solitary glomus tumors are thus divided into digital and extradigital.1,3
The characteristic symptomatic triad of these tumors is spontaneous pain, painful hypersensitivity to touch or pressure, and pain triggered by cold; these symptoms therefore enable rapid diagnostic suspicion in the event of pain in the fingers or subungual region.1,3 However, extradigital solitary glomus tumors do not usually present with the full range of symptoms, particularly pain triggered by cold,1,3 and so diagnosis at these sites is usually delayed 6 or 7 years, with multiple visits to the clinic and even psychological repercussion.1,3 Extradigital solitary glomus tumors usually present as erythematoviolaceous or bluish macules or papules, subcutaneous nodules, or even without clinical findings. In our patient, we could not palpate the nodule, although this was in principle accessible, because of the intense pain with the merest of brushes of the area with the telangiectatic macule. Imaging studies, such as magnetic resonance imaging1 and high-frequency ultrasonography,6 can help with diagnosis prior to histopathology. In ultrasound imaging, solitary glomus tumors appear as a well-delimited, hypoechoic oval or rounded lesion in the dermis, occasionally known as the stalk sign (presence of a hypoechoic vascularized prolongation that connects the lesion to adjacent tissues).6,7 In addition to these findings in B mode, Doppler mode provides additional signs: lesions generally well vascularized, with prominent vessels within, but without forming true vascular lakes, and predominantly arterial flows in pulsed Doppler studies, without clearly visualizing an arteriovenous shunt.7
This form of presentation as a telangiectatic macule is exceptional and is not clearly reflected in the literature of solid solitary glomus tumors. Schiefer et al.1 mentioned a small, painful, telangiectatic lesion that served as a guide to detect a solitary glomus tumor measuring 6mm on the subcutaneous cell tissue. There is also a rare clinical-pathological variant of glomangioma with a certain resemblance. In 1998, Requena et al.8 reported a plaque-like telangiectatic glomangioma as a new entity based on the telangiectatic appearance and its acquired nature. In 2013, Farias et al.9 reported another case of plaque-like telangiectatic plaque glomangioma. Apart from the clinical appearance of telangiectatic macula, they also have other features in common with those of our patient's lesion: they are solitary, acquired, painful lesions that occur in women. In 2007, Monteagudo et al.10 published another case of solitary glomangioma as a telangiectatic plaque in a 41-year-old women. The lesion was very similar but for the fact that it was congenital and asymptomatic. Unlike our case, these 3 lesions were larger and, histopathologically, they were glomangiomas.
We are unsure of the etiopathogenesis of these telangiectasias. We do not know whether they are induced by the tumor or are a reactive phenomenon, but in all cases, we believe that this is not a coincidence. Differential diagnosis could be considered with those processes that can present a telangiectatic appearance, such as mastocytosis; elastotic hemangioma; post-traumatic or drug-induced telangiectasias; angioma serpiginosum; collagen vasculopathy; generalized essential telangiectasia; acquired capillary malformation (Fegeler syndrome); those processes considered as reactive cutaneous angiomatoses, such as reactive angioendotheliomatosis, diffuse dermal angiomatosis, acroangiodermatitis, intravascular reactive histiocytosis, glomeruloid reactive angioendotheliomatosis, and angipericytomatosis11; as well as Kaposi sarcoma. However, the clinical presentation of a single painful lesion and the histopathology enable diagnosis to be established beyond doubt.
We describe an unusual presentation for solitary glomus tumor, with the appearance of a telangiectatic macule. It would be important to take into account such a presentation when assessing local and unexplained pain in extradigital regions so as not to delay diagnosis and to avoid the associated physical and psychological discomfort.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Allegue F, González-Vilas D, Fachal C, Zulaica A. Mácula telangiectásica como forma de presentación de un tumor glómico solitario. Actas Dermosifiliogr. 2020;111:434–436.