During pregnancy, delivery, and postpartum, a series of diagnostic and therapeutic procedures are currently performed which have led to reduced neonatal morbidity and mortality but which have also increased the risk of certain iatrogenic cutaneous and traumatic injuries.1–3
The incidence of fetal puncture due to amniocentesis has declined since the introduction of ultrasound guidance4,5; however, increasing maternal age has led to more frequent use of amniocentesis,6 thus making awareness of fetal puncture a matter of importance for dermatologists, obstetricians, and pediatricians.7
This letter describes the case of a 3-month-old infant who presented several skin dimples as a result of amniocentesis-related puncture. A search of the literature found no other cases of this entity in which a histopathologic study had been performed.5
A male infant aged 3 months with no relevant medical history presented for assessment of a number of skin lesions on the abdomen and left thigh which were first noticed during the first month of life. The infant had no congenital abnormalities and had been born following a full-term pregnancy by unassisted vaginal delivery in cephalic presentation. One of the techniques performed on the mother during gestation and delivery was an amniocentesis in the 18th week which required several punctures.
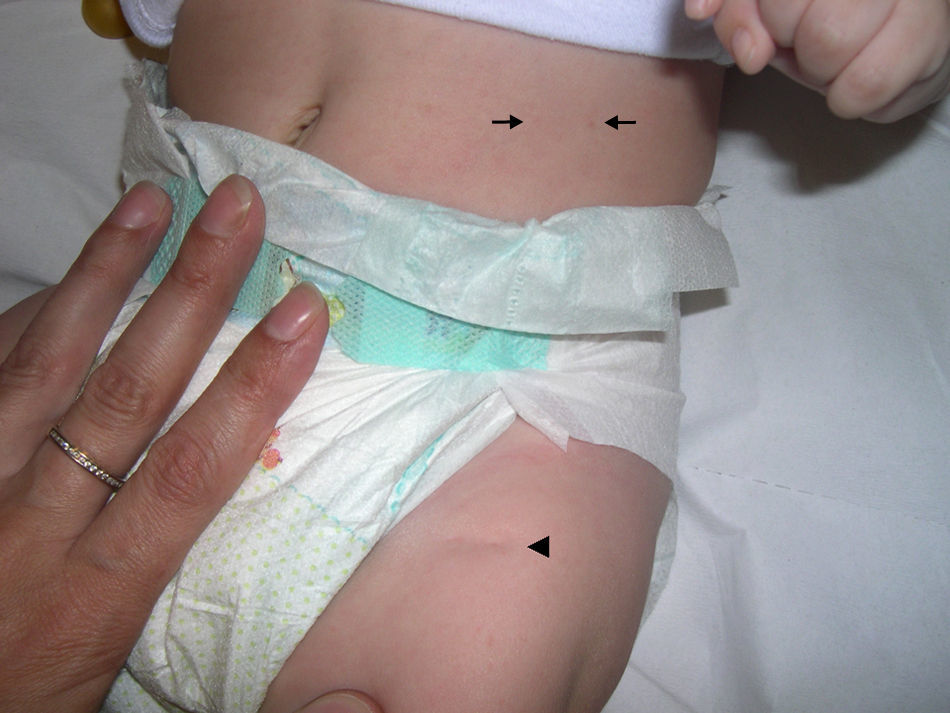
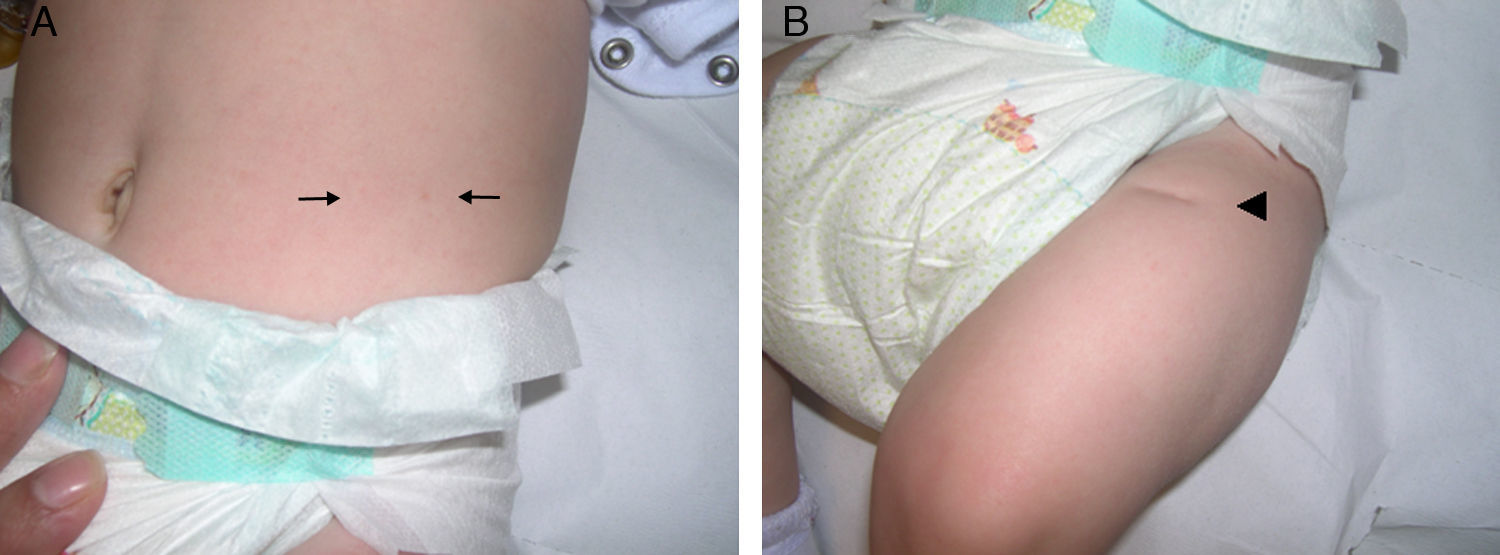
A physical examination revealed 2 dimples measuring 2 mm in diameter on the left side of the abdomen and a linear depression 1.2 cm long on the anterior aspect of the proximal third of the left thigh (Figs. 1 and 2). The patient did not present any other skin lesions, involvement of the oral or genital mucosae, or abnormalities of the hair or nails. The infant's weight and height were normal.
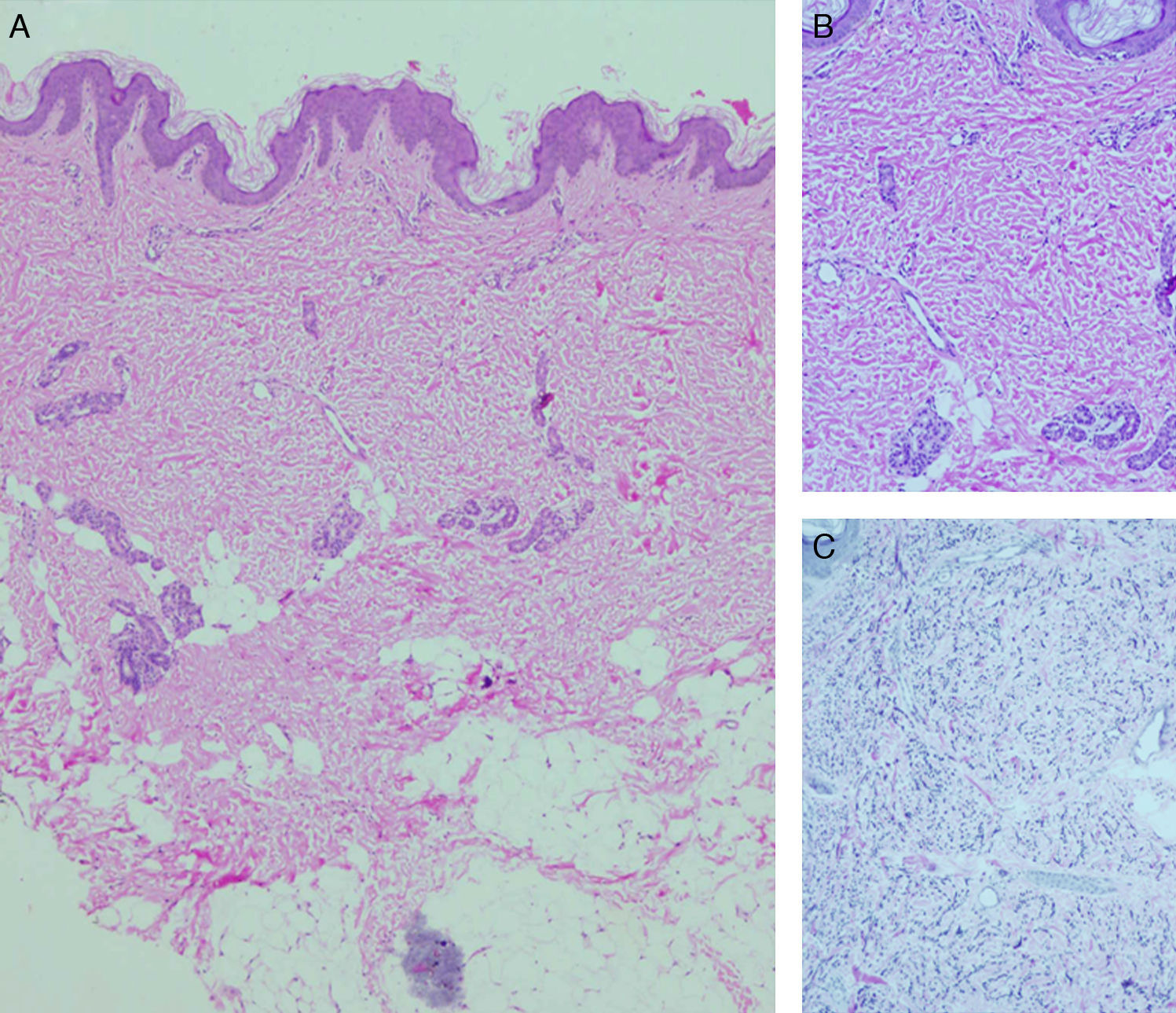
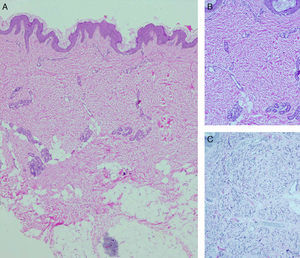
A diagnosis of skin dimpling as a complication of amniocentesis was established. The parents were informed of the benign nature of the skin condition, although they decided to request a biopsy of the thigh lesion so as to rule out other pathologies. The histopathologic study revealed a dermis with collagen bundles having an abnormal morphology and distribution (fine bundles arranged in multiple directions). A reduction and fragmentation of elastic fibers was observed using orcein staining. No abnormalities were seen in the epidermis or the subcutaneous tissue (Fig. 3). The skin lesions remained unchanged over the subsequent 8 months.
A, Low-magnification view, epidermis with 2 scalloped areas and compact, wide dermis with few adnexa (hematoxylin-eosin, original magnification ×20). B, In greater detail, thin collagen bundles in the dermis (hematoxylin-eosin, original magnification ×100). C, Fragmented and reduced elastic fibers in the dermis (orcein staining, original magnification ×100).
Amniocentesis is the most frequently used technique for prenatal diagnosis of genetic alterations. It is usually performed during the second trimester of pregnancy. One of the possible complications of the procedure is fetal puncture, the most frequent manifestation of which is skin dimpling.4 Amniocentesis may also cause injury to underlying structures, such as peripheral nerves, tendons, or the eyeball, and result in ileocutaneous or arteriovenous fistulas.3
Skin dimpling as a complication of amniocentesis presents as punctate depressions or linear scars measuring 1 to 5 mm in diameter. These manifestations may be isolated or multiple; when multiple, they are sometimes grouped and sometimes follow a linear path due to fetal puncture along a single plane. Clearer observation may be achieved by pinching the surrounding skin.8 Skin dimples caused by amniocentesis are present at birth, although some are not clearly visible until weeks or months later; they do not resolve spontaneously.6 The most common site is the thigh, followed by the abdomen, buttocks, and upper limbs. These dimples tend to be found by chance during examination and are not usually the reason for consultation.7 It has been speculated that dimpling results from localized lipoatrophy or a loss of subcutaneous tissue. The histopathologic findings in this case, namely, fine collagen bundles and a reduction in elastic fibers, are consistent with localized depressed scarring secondary to skin retraction caused by a puncture wound.5
The advent of ultrasound guidance during amniocentesis reduced the incidence of skin dimpling from nearly 9% to under 1%.3 However, the unpredictability of fetal movement—especially of the limbs—makes some instances of puncture inevitable.6,8 Several factors increase the risk of this complication, such as performing the technique in the third trimester, when the fetus is of a larger size in proportion to the amniotic cavity; repeated puncture attempts; and lack of obstetrician experience.7,8
The diagnosis, although never absolutely certain, is established by ruling out other associated findings, the location of the dimples, and a history of amniocentesis.5,7 These indicators allow clinicians to rule out other iatrogenic and traumatic injuries resulting from fetal monitoring, amniotomy, episiotomy, venous and arterial puncture, assisted delivery (i.e., vacuum-assisted, forceps, or spatula-assisted), or cesarean section (long but very superficial scalpel related lacerations).2,3,6 Additionally, diagnosis must take into consideration other congenital causes of skin dimpling. These congenital causes can be either dermal sinuses with cutaneous openings or deep cutaneous depressions. Congenital skin dimples are almost always variations of normality and are situated over bony prominences, especially those of the face. They may be familial forms or related to infection, metabolic disorders, or the use of certain drugs during pregnancy; occasionally they are signs of an underlying abnormality, a polymalformative syndrome, or a neurological or bone and muscle disorder.9 Other processes that should be taken into consideration include cutaneous aplasia, focal dermal hypoplasia, amniotic band syndrome, and supernumerary nipples.3,10
In summary, dermatologists should be aware of the presence of skin dimpling as a complication of amniocentesis both to avoid incorrect diagnostic presumption and to limit the number of additional and potentially aggressive tests performed.
Please cite this article as: Monteagudo B, et al. Hoyuelos cutáneos como consecuencia de amniocentesis: hallazgos histopatológicos. Actas Dermosifiliogr. 2013;104:729–31.