Sinusoidal hemangioma (SH) is a rare benign vascular proliferation that usually presents as a solitary subcutaneous lesion in middle-aged, predominantly female patients. Diagnosis is histological. The radiological characteristics of this entity have not been described to date. We present 3 cases of subcutaneous lesions corresponding to SH and describe the corresponding histologic and ultrasound findings.
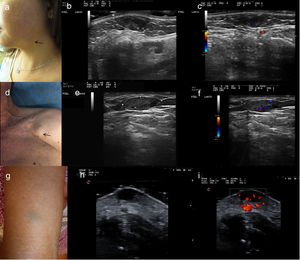
The first patient was a 49-year-old woman who was seen for an asymptomatic lesion in the left mandibular region that had appeared 2 years earlier. Physical examination revealed an elastic, soft-tissue nodule of 1 cm in diameter and mild bluish discoloration of the overlying epidermis (Fig. 1A). Ultrasound was performed using an 18-MHz probe (Esaote MyLab). B-mode showed a well-circumscribed hypoechoic lesion located in the dermis, with internal anechoic areas and intralesional hyperechogenic dots without posterior acoustic shadowing (Fig. 1B). Color Doppler mode showed mild intralesional vascularization (Fig. 1C). Histology revealed thin-walled, interconnected, dilated vascular channels in which pseudopapillary structures were evident, as well as areas of calcification and recanalized vascular thrombi (Fig. 2A and B).
A, Clinical presentation of Case 1: a subcutaneous nodule of 10 mm in diameter in the left mandibular region with bluish discoloration of the overlying epidermis. B, Ultrasound examination in B-mode reveals a well-circumscribed, homogeneous hypoechoic lesion in the dermis, with hyperechoic dots without posterior acoustic shadowing. C, Ultrasound examination in color Doppler mode, revealing mild intralesional vascularization. D, Clinical presentation of Case 2: a subcutaneous mass of 20 mm in diameter in the right pectoral region, with no associated alterations in the epidermis. E, Ultrasound examination in color Doppler mode, revealing a well-circumscribed, homogeneous hypoechoic lesion in the subcutaneous cellular tissue. F, Ultrasound examination in color Doppler mode, revealing moderate intralesional vascularization. G, Clinical presentation of Case 3: a subcutaneous lesion of 1 cm in diameter with a slightly greenish-blue overlying epidermis. H, Ultrasound examination in B-mode revealing a well-circumscribed hypoechoic lesion in the dermis. I, Ultrasound examination in color Doppler mode, revealing prominent intralesional and perilesional vascularization.
A and B, Case 1. Histology shows focal calcification inside the lesion and intravascular thrombosis (hematoxylin-eosin [HE], original magnification ×40). C, Case 2. Histology shows a well-circumscribed lobed mass composed of multiple, thin-walled, dilated and interconnected vascular channels that form sinusoidal structures (HE, original magnification ×40). D, Case 3. Histology shows dilated, interconnected vascular channels forming a sinusoidal pattern, with no evidence of calcifications or thrombi (HE, original magnification ×40). E, Case 2. Immunohistochemistry for WT1 (original magnification ×200). F, Case 2. Immunohistochemistry for D2-40 (original magnification ×200).
The second patient was a 72-year-old man who was being followed for nonmelanoma skin cancer in the facial region and the trunk. He was seen for an asymptomatic lesion in the left pectoral area that had appeared more than 6 months earlier. Physical examination revealed an elastic, easily movable lesion in soft tissues of 2 cm in diameter, with no associated alterations in the epidermis (Fig. 1D). Skin ultrasound with an 18-MHz probe (Esaote MyLab) showed a well-circumscribed hypoechoic lesion in the subcutaneous tissue (Fig. 1E). Color Doppler mode revealed intralesional vascularization (Fig. 1F). Histology showed more extensive vascular channels than in the first patient, with no evidence of marked calcification or thrombi (Fig. 2C).
The third patient was a 77-year-old woman with no past history of interest who was seen for a slow-growing, asymptomatic lesion on the dorsal aspect of the right arm that had appeared several years earlier. Physical examination revealed an elastic subcutaneous lesion of 1 cm in diameter and mild greenish-blue discoloration of the overlying epidermis (Fig. 1G). Skin ultrasound with an 18-MHz probe (Esaote MyLab) showed a well-circumscribed lesion of mixed echogenicity, with both anechoic and hypoechoic areas, located in the dermis (Fig. 1H). Color Doppler mode showed prominent intralesional and perilesional vascularization (Fig. 1I). Histology showed interconnected, dilated vascular channels forming a sinusoidal pattern, with no evident calcifications or thrombi (Fig. 2D).
Immunohistochemistry was performed in all 3 cases. All patients were positive for WT1 and CD31 and negative for GLUT1 and D2-40 (Fig. 2E and F).
SH is a very rare vascular proliferation first described by Calonje and Fletcher in 19911 as a variant of cavernous hemangioma. Currently, it is not included in the classification proposed by the International Society for the Study of Vascular Anomalies, although it can be considered a cutaneous vascular anomaly.2 SH typically presents as a usually asymptomatic, subcutaneous nodule with a bluish surface. It most often appears on the extremities, predominantly in middle-aged women. Histologically, SH is characterized by a lobular architecture. The lobes consist of dilated, interconnected, thin-walled vascular channels that form a sinusoidal pattern. The vessels are tightly packed with little stroma, giving rise to a pseudopapillary pattern in tangential sections of the walls, and thromboses and calcifications are typically observed at the center of the lesion.3 In our 3 cases, immunohistochemistry revealed findings similar to those described previously, suggesting that SH is better classified as a vascular tumor than a vascular malformation.4 Descriptions of the imaging characteristics of these tumors are scarce: they are described as solid lesions located in the subcutaneous tissue with slow vascular flow on magnetic resonance imaging and arteriography. A case report by Park et al.2 describes a hypoechoic lesion with no internal Doppler signal located between 2 parallel vessels, which may correspond to an artery and a draining vein, but reports no connection between the tumor and these vessels. This finding was not observed in any of our 3 cases. It has been proposed that the presence or absence of intralesional Doppler signal may be related to the presence of thromboses or areas of ischemia within the vessels that comprise the lesion. In our 3 cases, the tumor with the weakest intralesional Doppler signal had the highest levels of thrombosis, as well as intralesional hyperechogenic dots without posterior acoustic shadowing that correlated with calcifications on histology. Kitamura et al.5 previously described a case of SH with diffusely distributed intralesional hyperechogenic dots, some of which presented posterior acoustic shadowing, corresponding to calcifications on histology. These calcifications had been described earlier by Nakamura and Miyachi.3 Those authors proposed a relationship between the presence of calcifications and time since lesion appearance and low intralesional flow, in agreement with the characteristics of the first case described here. In the second and third cases color Doppler mode revealed intralesional vascularization, a rare finding in these lesions6,7 that histologically corresponds to vascular lumina. No calcifications were observed on histology and hyperechogenic dots were absent on ultrasound.
In conclusion, we present 3 cases of SH and describe the corresponding ultrasound and histological findings. In 2 of the 3 cases we observed marked intralesional vascularization, an uncommon feature in this type of lesion. Although ultrasound allows assessment of lesion vascularization and the relationship with adjacent structures, there are no distinctive ultrasound findings that enable diagnosis, which is fundamentally based on histological findings.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: García-Harana C, et al. Hemangioma sinusoidal: correlación entre hallazgos ecográficos e histológicos en 3 casos. Actas Dermosifiliogr. 2020;111:181–183.



![A and B, Case 1. Histology shows focal calcification inside the lesion and intravascular thrombosis (hematoxylin-eosin [HE], original magnification ×40). C, Case 2. Histology shows a well-circumscribed lobed mass composed of multiple, thin-walled, dilated and interconnected vascular channels that form sinusoidal structures (HE, original magnification ×40). D, Case 3. Histology shows dilated, interconnected vascular channels forming a sinusoidal pattern, with no evidence of calcifications or thrombi (HE, original magnification ×40). E, Case 2. Immunohistochemistry for WT1 (original magnification ×200). F, Case 2. Immunohistochemistry for D2-40 (original magnification ×200). A and B, Case 1. Histology shows focal calcification inside the lesion and intravascular thrombosis (hematoxylin-eosin [HE], original magnification ×40). C, Case 2. Histology shows a well-circumscribed lobed mass composed of multiple, thin-walled, dilated and interconnected vascular channels that form sinusoidal structures (HE, original magnification ×40). D, Case 3. Histology shows dilated, interconnected vascular channels forming a sinusoidal pattern, with no evidence of calcifications or thrombi (HE, original magnification ×40). E, Case 2. Immunohistochemistry for WT1 (original magnification ×200). F, Case 2. Immunohistochemistry for D2-40 (original magnification ×200).](https://static.elsevier.es/multimedia/15782190/0000011100000002/v1_202004140647/S1578219020300068/v1_202004140647/en/main.assets/thumbnail/gr2.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



