The patient was a 33-year-old white man recently diagnosed with human immunodeficiency virus (HIV) and under treatment with highly-active antiretroviral therapy (HAART), consisting of darunavir, ritonavir, and tenofovir/emtricitabine, for the last 3 months. He was referred with a 2-week history of a single asymptomatic lesion in the mouth that caused occasional bleeding and discomfort when eating.
Physical ExaminationExamination revealed a sessile, exophytic nodule with a fleshy appearance and smooth surface; it measured 8mm in diameter and was located on the inner surface of the lower gum (Fig. 1). The general assessment of the patient confirmed the absence of palpable locoregional lymph nodes or associated skin or mucosal lesions.
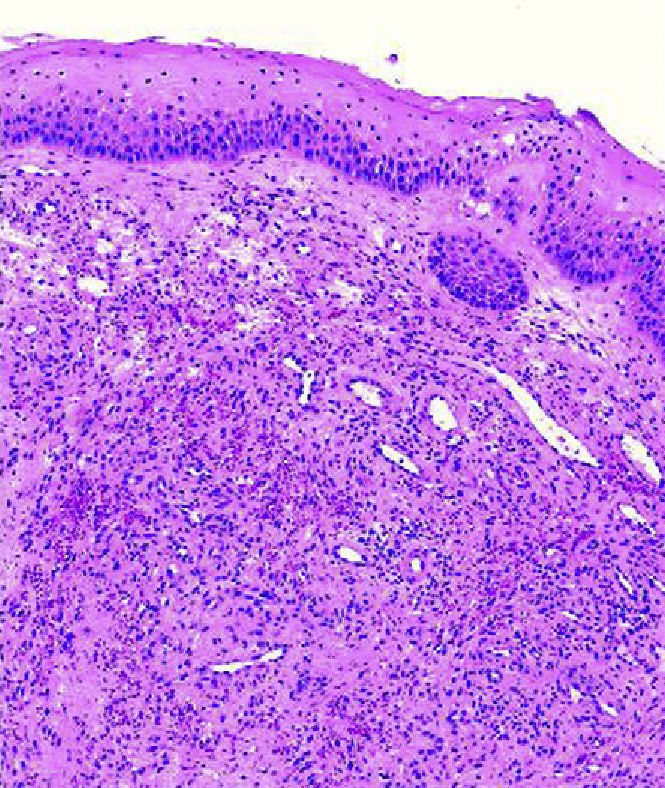
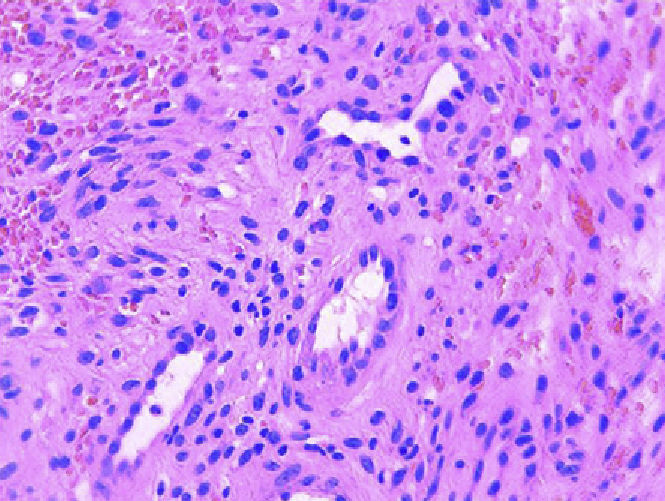
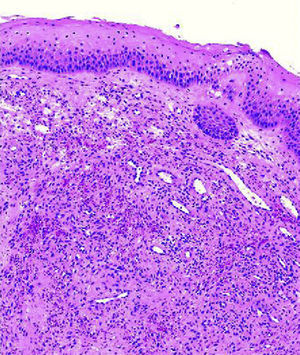
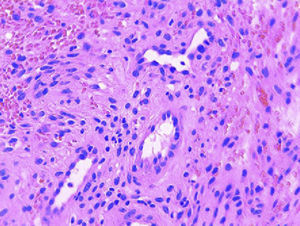
HistopathologyThe lesion was removed by shave excision, followed by coagulation of the base. Histologic examination by hematoxylin-eosin staining revealed a diffuse dermal proliferation of spindle cells that penetrated between the collagen bundles, along with the formation of blood-filled vascular spaces (Fig. 2). Several preexisting blood vessels were also observed protruding towards the newly formed vessels (Fig. 3). Immunohistochemistry was positive for herpes virus type 8 (HHV-8).
What Is Your Diagnosis?
DiagnosisOral Kaposi sarcoma.
Clinical CourseScreening studies excluded visceral involvement. The lesion was completely removed by shave excision at the first visit and required no additional treatment.
DiscussionKaposi sarcoma is the most commonly diagnosed tumor in patients with acquired immunodeficiency syndrome and accounts for 90% of all cancers in this group.1 The oral cavity is a common site of epidemic Kaposi sarcoma and it is estimated that 71% of HIV-positive patients with Kaposi sarcoma present lesions in this location. In 22% of cases the tumor initially presents in the mouth.2 The most common clinical manifestations are dark red to violaceous macules and ulcerated nodular lesions, mainly located on the palate.
Favorable conditions created by HIV infection include a predominance of TH1 cytokines, such as interferon-gamma, tumor necrosis factor alpha, and interleukins 1 and 6, all of which are known to induce Kaposi sarcoma.
The introduction of HAART promotes the healing of Kaposi sarcoma lesions and prevents the appearance of others, mainly due to the reduction of the HIV and HHV-8 load3,4 and a decrease in antiangiogenic and antiinflammatory factors. However, after starting treatment with HAART, patients may also experience inflammatory immune reconstitution syndrome, a paradoxical reaction, with exacerbation of opportunistic infections in the context of immunological recovery.5
The example we present is the result of the combination of both factors: immune response to a preexisting opportunistic HHV-8 infection and the inflammatory component of inflammatory immune reconstitution syndrome (reflected by the rapid growth and pedunculated form of the tumor).
Please cite this article as: Catalá A, et al. Nódulo sésil en mucosa gingival. Actas Dermosifiliogr.2012;103:433-4.