Within the broad range of manifestations that syphilis can cause, lesions on the oral mucosa and eye involvement are very rare, particularly as isolated lesions. We describe a patient with oral lesions and eye involvement, with no associated skin lesions.
The patient was a 59-year-old man, with no past history of interest. He was referred from another center to investigate a 1-year history of oral mucosal symptoms presenting as odynophagia, a sensation of excess mucus secretion, and painful erosive lesions in the oral cavity and pharynx. The patient had also been seen in ophthalmology for a decrease in visual acuity over the previous 3 months.
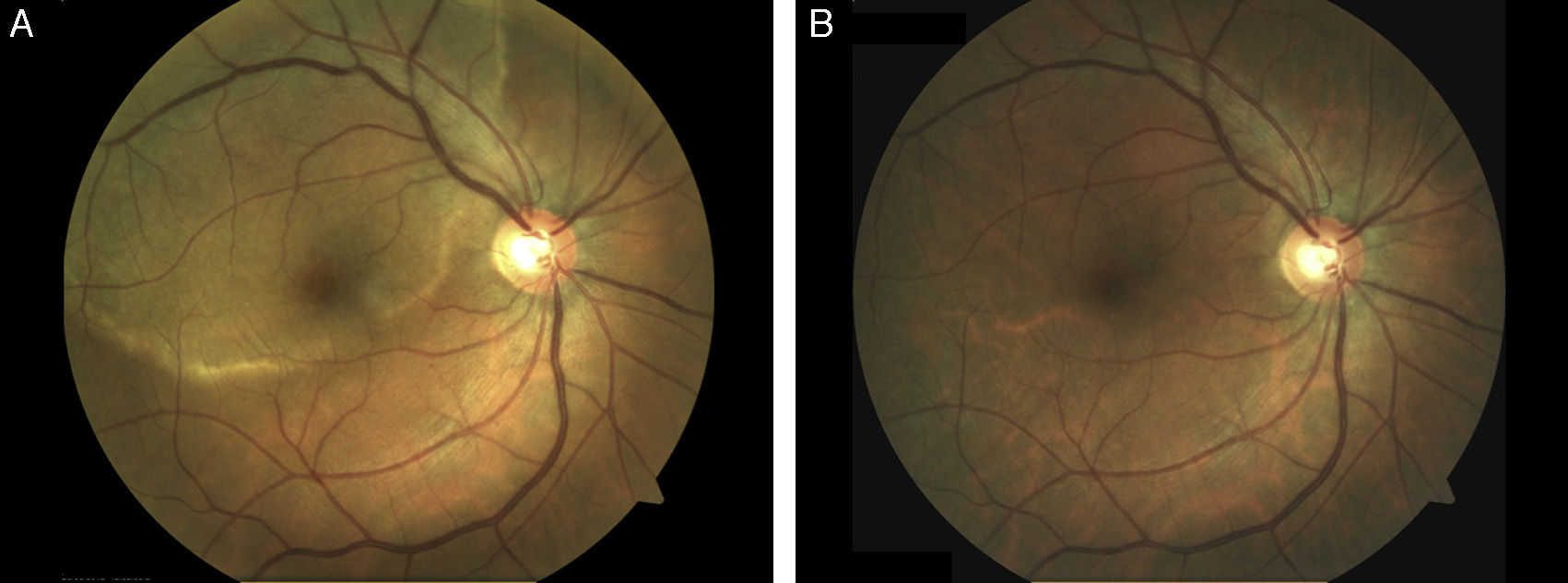
Physical examination revealed erosive lesions on the hard palate and on the right tonsillar pillar (Fig. 1) and difficulty swallowing. On ophthalmologic examination, a large, circular, yellowish placoid lesion was observed on the pigmented epithelium of the retina, at the macula. The lesion extended to the upper temporal vascular arches of the right eye (Fig. 2A). Visual acuity was 20/50. This was initially considered as a chorioretinitis of uncertain origin. Biopsy of an oral lesion showed epidermal hyperplasia with a dense mixed inflammatory infiltrate with a predominance of plasma cells that extended into the deep dermis and was localized mainly around the blood vessels. Lymphocyte exocytosis was also observed. A provisional diagnosis of secondary syphilis was made, and staining with antitreponemal antibody showed the presence of numerous spirochetes in the mucosa and in smaller numbers in the submucosa. Syphilis serology in blood was positive (rapid plasma reagin, 1:128; treponema pallidum hemagglutination test, +). On further questioning, the patient denied previous skin lesions but did state that about 18 months earlier he had had an erosion on the glans that had been diagnosed as genital herpes at other center. Based on these findings, we made a diagnosis of posterior placoid chorioretinitis of probable syphilitic origin. HIV serology was negative and lumbar puncture showed a slight increase in the protein content of the cerebrospinal fluid (64mg/dL), with normal cellularity and glucose levels and positive reagin antibodies titers (Venereal Disease Research Laboratory). A diagnosis was therefore made of secondary syphilis with central nervous system involvement (neurosyphilis) and the patient was treated with penicillin G sodium at a dose of 4 million IU intravenously every 4hours for 14 days. The clinical course was favorable, with resolution of the oral lesions and a clear improvement in the ocular lesion (Fig. 2B).
Syphilis can cause oral lesions in all of its stages, but they are most common in the secondary stage (30% of patients). However, the absence of concomitant skin manifestations, as in our case, is very rare.1 The oral lesions of secondary syphilis are clinically very heterogeneous and typically nonspecific; they include macules, papules, plaques and ulcers, which may be single or multiple, and they are usually associated with nonspecific pharyngitis, tonsillitis, or laryngitis, sometimes with palpable lymph nodes.2 These lesions most frequently occur together with the typical cutaneous manifestations of the disease, and usually resolve within 3 to 12 weeks.3 In the present case, however, the lesions were isolated and persisted for at least a year. In a review of the literature, we found isolated case reports of oral lesions without associated skin manifestations,3,4 but none had a clinical course of more than 5 months in patients who, like ours, were immunocompetent.
Isolated lesions of syphilis on the oral mucosa are a considerable diagnostic challenge, and the histology of these lesions must therefore be carefully evaluated for any detail that will help to reach the diagnosis. In addition, the patient must be questioned closely about noncutaneous features of the disease, which must be investigated in detail as in the more common forms of the disease. Microscopy is often relatively nonspecific, but a recent article suggested that the presence of perivascular or perineural infiltrates of plasma cells and lymphocyte exocytosis could be signs that support the diagnosis.5 In our case, the infiltrate of plasma cells was very dense and intense lymphocyte exocytosis was observed, leading us to suspect the diagnosis.
The extracutaneous manifestations can be very varied. Eye involvement is one of the less common manifestations but, when it occurs, it usually develops during the secondary phase of the disease and it can affect any segment of the globe. Scleritis and uveitis are the most common forms of presentation, but keratitis and conjunctivitis can also develop.6,7 Acute syphilitic posterior placoid chorioretinitis (ASPPC) is a recently described ocular manifestation and is extremely rare in immunocompetent patients such as the patient we describe.8
ASPPC was first described in 1988 and, since that time, only 60 cases have been published, of which 40% were diagnosed in HIV-positive patients.9 Clinically, ASPPC is characterized by the appearance of yellowish placoid lesions situated at the macula and there is a marked loss of visual acuity.9 The search for extracutaneous manifestations, and for eye involvement in particular, is essential in these patients (especially if associated with immune compromise), as these alterations not only affect the prognosis of the disease but they are also of importance when choosing the treatment to be administered. The presence of syphilitic eye lesions, as in the present case, is diagnostic of neurosyphilis, making the patient a candidate for intravenous treatment.
Although the incidence of neurosyphilis is low in immunocompetent patients (0.2-2.1 cases per 100000 population10) and that of syphilitic ocular involvement is even lower, the increase in the number of cases of syphilis in recent years in developed countries requires us to be aware of the most atypical and least common presentations of this disease as, when this is not diagnosed early, the infection can spread and the harm to the patient can increase.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Plana-Pla A, Pelegrín-Colás L, Bielsa-Marsol I, Ferrandiz-Foraster C. Lesiones orales y coriorretinitis placoide posterior como forma de presentación de sífilis secundaria en un paciente inmunocompetente. Actas Dermosifiliogr. 2016;107:783–784.