Lichen amyloidosis (LA) is a form of primary localized cutaneous amyloidosis that is associated with pruritic skin-colored or hyperpigmented hyperkeratotic papules1,2; these papules can coalesce to form plaques that often display a wavy pattern. The lesions are found mainly in the pretibial region, and generalized involvement is uncommon.3,4 Numerous approaches have been used to treat LA, although none has achieved a complete cure. We present a case of generalized LA that responded satisfactorily to narrowband UV-B therapy.
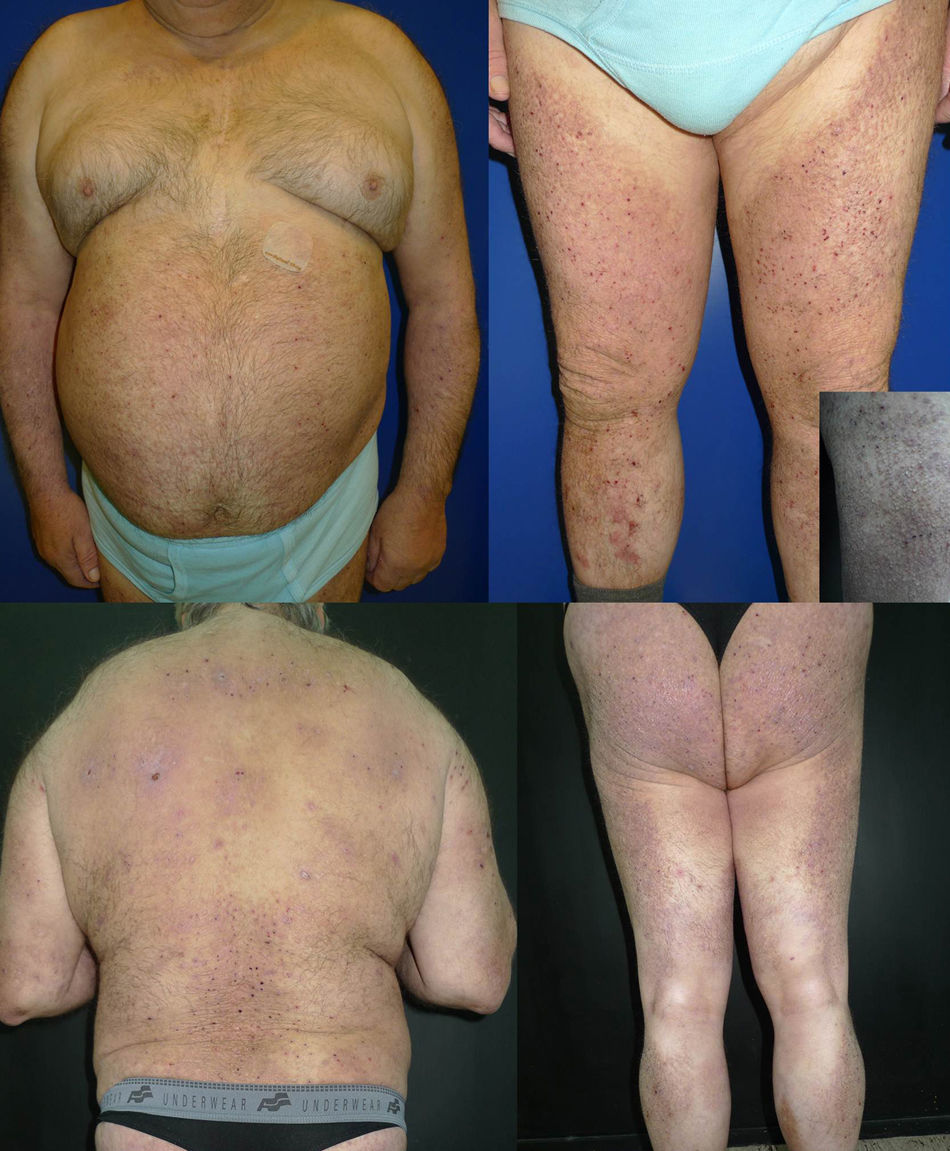
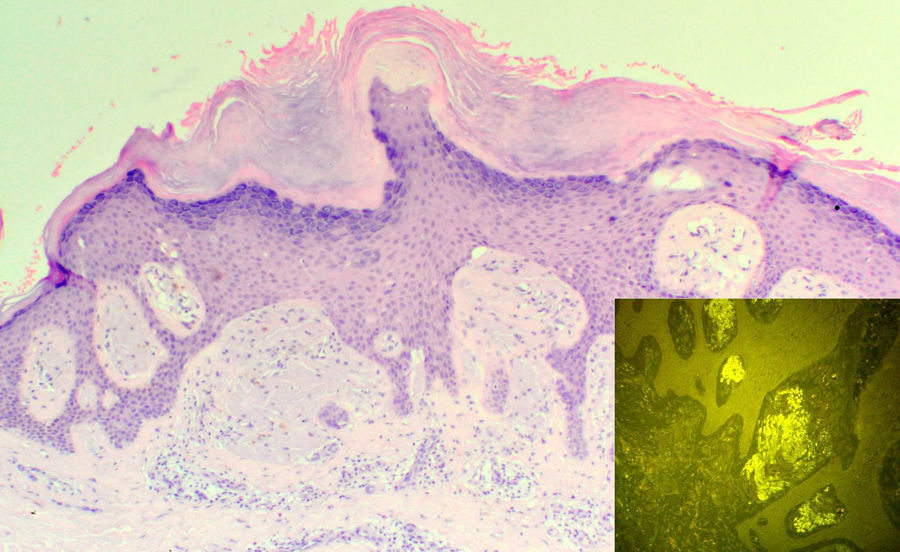
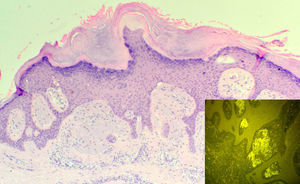
The patient was a 69-year-old man with Fitzpatrick skin type III and a past history of insulin-dependent diabetes mellitus, arterial hypertension, and ischemic heart disease. He consulted for pruritic lesions on the trunk and extremities that had first appeared 4 years earlier and had been treated unsuccessfully with topical corticosteroids. A series of laboratory and additional tests were performed to screen for potential causes of the pruritus, and the patient did not present an underlying eczematous condition. Physical examination revealed slightly desquamating plaques formed of multiple hyperpigmented hemispheric papules, many of which had been eroded by scratching. The lesions affected the anterior and posterior surfaces of the arms and legs, abdomen, back, and buttocks, with a symmetrical bilateral distribution (Fig. 1). Histopathology revealed compact orthokeratotic hyperkeratosis, irregular acanthosis, and deposits in the papillary dermis that caused widening of the papillae with lateral shift of the epidermal ridges. The deposits were composed of acellular, amorphous eosinophilic material with abundant fissures caused by retraction; the material fluoresced green with thioflavin T (Fig. 2). We thus confirmed the diagnosis of LA. Phototherapy with narrowband UV-B was started (3 times weekly). The initial dose was 0.35J/cm2 (determined according to phototype), which was increased by 10% to 20% at each session. A significant reduction in the pruritus and progressive flattening of the papules in all the affected areas was observed from the initial sessions. Complete resolution of the lesions on the trunk and arms was achieved after 57 sessions and a cumulative dose of 109.27J/cm2 (maximum dose, 2.33J/cm2) (Fig. 3). The physical and symptomatic improvement persisted at the time of writing, after 4 months of follow-up, with no further treatment.
Compact orthokeratotic hyperkeratosis, irregular acanthosis, and deposits in the papillary dermis that caused widening of the papillae with lateral shift of the epidermal ridges (hematoxylin-eosin, original magnification x100). Inset: Deposits of amyloid material in the papillary dermis showing green fluorescence (thioflavin T, original magnification x200).
Treatment of LA is somewhat unsatisfactory. The different approaches tried include topical or intralesional corticosteroids, oral and topical dimethylsulfoxide, calcineurin inhibitors, oral retinoids, cyclophosphamide, dermabrasion, and neodymium:yttrium-aluminum-garnet laser therapy, as well as various phototherapy modalities.1,5
Only 3 cases of LA treated satisfactorily with narrowband UV-B therapy have been reported to date.5–7 In 2 of those cases, LA was associated with refractory atopic dermatitis, and narrowband UV-B was combined with other treatments to improve the clinical condition.5,6 The third case involved a man with generalized LA whose lesions characteristically affected areas of the body with lower skin temperatures, sparing areas with higher temperatures. The patient's response to narrowband UV-B monotherapy was excellent.7
The amyloid substance in LA is thought to originate from necrosis of the epidermal keratinocytes of the basal layers of the epidermis.8 Narrowband UV-B therapy diminishes basal cell activity, thus reducing the production of amyloid.5 Furthermore, narrowband UV-B has proven effective for the treatment of pruritus by suppressing the proliferation of keratinocytes and reducing apoptosis of keratinocytes and T cells and inflammation. In this way, it is possible to diminish or eliminate one of the factors that very probably induce and/or worsen LA. Other authors consider that the effectiveness of narrowband UV-B therapy is due to the marked elevation of the temperature in the booth, with the consequent increase in skin temperature and suppression of the heat-dependent synthesis of amyloid.7
Grimmer et al.9 recently reported 2 cases of LA treated with a combination of psoralen-UV-A therapy and oral acitretin. The authors concluded that this modality was effective and practical and that its effects were maintained over time. Finally, a study that compared the efficacy of topical corticosteroids with UV-B phototherapy and topical psoralen-UV-A in patients with LA found better results, namely, diminished pruritus and a decrease in the number of skin lesions, in the areas treated with phototherapy.10
To our knowledge, we present the second case of LA not associated with other skin conditions and that responded satisfactorily to narrowband UV-B in monotherapy. Although further studies are necessary to define the exact mechanism of action and level of efficacy, we believe that narrowband UV-B therapy could represent a safe and effective alternative in the management patients with generalized LA lesions.
Please cite this article as: Alonso-González J, et al. Liquen amiloide generalizado con respuesta satisfactoria a ultravioleta B de banda estrecha. Actas Dermosifiliogr. 2013;104:527–9.