In their excellent study on erythroderma, Cuellar-Barboza et al.1 analyze the various causes of this condition in adults. The etiology is neoplastic or paraneoplastic in 1% of cases, and, within this group, erythroderma is most frequently associated with hematological malignancies and cutaneous T-cell lymphomas, which account for 25%–40% of cases of erythroderma associated with cancer.
Of note, the authors compile a series of laboratory findings and group them by frequency. These have previously been reported in the literature and include elevated erythrocyte sedimentation rate, leukocytosis, eosinophilia, anemia, liver function, and kidney function. They highlight the importance of the eosinophil count in drug reaction with eosinophilia and systemic symptoms syndrome and call to mind the association between eosinophilia and malignant erythroderma. Their approach stresses the usefulness of Sézary cell count analysis in the diagnosis of Sézary syndrome and mycosis fungoides.
Given the difficulty and importance of the diagnosis of paraneoplastic erythroderma, we believe it would be interesting for the protocol put forward by the authors to include simple and accessible biomarkers that could assist in screening for tumors associated with erythroderma. In this sense, various studies have shown that increased levels of cyanocobalamin (vitamin B12) are correlated with an increased risk of occult solid and hematologic malignancies.1–8
Pathophysiology is based on the metabolism of cobalamin: under normal conditions, most cobalamin in blood (80%) does not circulate freely and must bind to transport proteins, namely, haptocorrin2–5 or type I transcobalamin,3,5,8 both of which can be synthesized by granulocytes.3,5 In addition, the levels of these transport proteins in blood are correlated with serum cobalamin levels, thus explaining the high levels detected in blood dyscrasia.2–8
Nevertheless, high cobalamin levels have also been observed in some solid tumors (e.g., pharynx, esophagus, liver, stomach, biliary tract, pancreas, lung, colon-rectum, prostate, ovary, cervix, and bladder),2–7 possibly because the synthesis of type I transcobalamin could be increased by neoplastic cells themselves.3,8 On the other hand, since haptocorrin4 and type I transcobalamin8 are metabolized in the liver, primary tumors affecting the liver,2,3,8 metastases,3,8 or other non–tumor-related causes3,6,8 would make it possible to detect high serum cobalamin levels owing to the reduced clearance of the binding proteins.
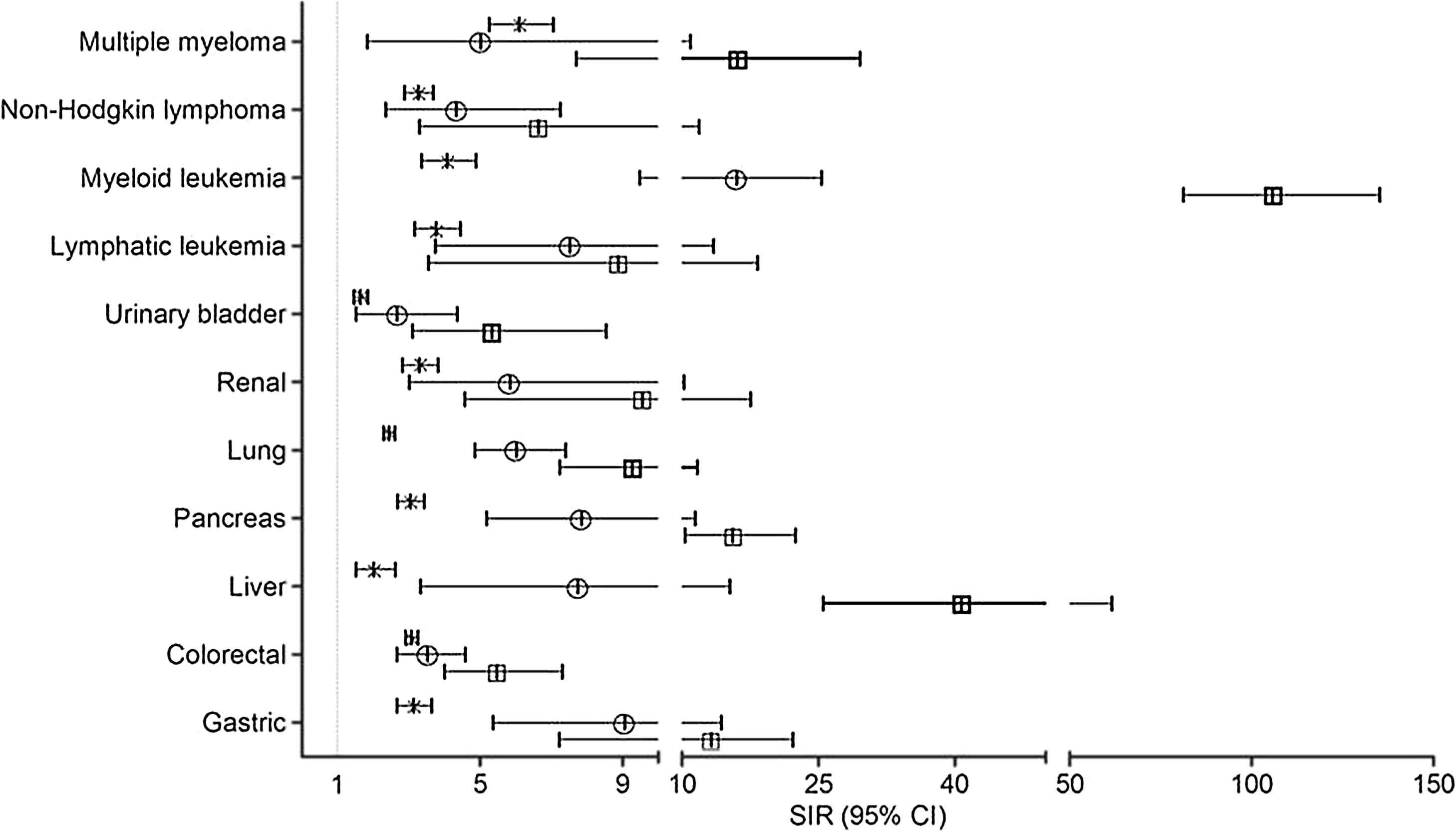
Arendt et al.2 conclude that, while high cobalamin could be associated with smoking, alcohol, or liver disease, levels above 800 pmol/L are significantly associated with neoplasms, especially hematologic malignancies, such as non-Hodgkin lymphoma, Hodgkin lymphoma, multiple myeloma, and leukemia (Fig. 1). We include the graph from Arendt et al.,2 which shows the risk of diagnosing various types of tumor during the same year plasma cobalamin levels are determined.
In this sense, Chiche et al.3 demonstrate the statistically significant association between vitamin B12 concentrations greater than 1275 pg/mL and hematologic malignancy.
Later studies4,6 reveal similar results and a poorer prognosis and higher mortality rates have been demonstrated for patients with cancer and elevated B12 levels than those with cancer and normal B12 levels.4
In conclusion, we believe that it would be interesting to include serum cobalamin levels in the erythroderma protocol of Cuellar-Barboza et al.,1 since such a determination is simple, inexpensive, and accessible when screening for paraneoplastic erythroderma, especially that associated with hematologic malignancy.
Please cite this article as: Andamoyo-Castañeda A, Gómez-Moyano E, Godoy Díaz DJ, Martínez Pilar L. Papel de la cianocobalamina en el abordaje práctico de la eritrodermia paraneoplásica. Actas Dermosifiliogr. 2021;112:199–200.