The coronavirus disease 19 (COVID-19) pandemic led to large-scale lockdown in many countries, including Spain. This measure caused significant changes in health care delivery and societal attitudes, potentially leading to delays in the diagnosis of skin tumors. In most malignant skin tumors, there is a direct relationship between tumor size, time since onset, and prognosis.1,2 The aim of this study was to evaluate the attitudes of patients with a malignant skin tumor during the COVID-19 state of emergency and determine the impact of lockdown on these tumors. The study was performed at the Dermatology Department of Hospital Clínico Universitario in Valencia, Spain. Patients presenting with a melanocytic tumor, a fast-growing tumor, or a tumor with a diameter larger than 1 cm during the easing of lockdown restrictions (May 18 to June 30, 2020) were included. Those with a clinical diagnosis of basal cell carcinoma (BCC) or squamous cell carcinoma (SCC) in situ were excluded. All patients were asked to complete a structured questionnaire (see supplementary material).
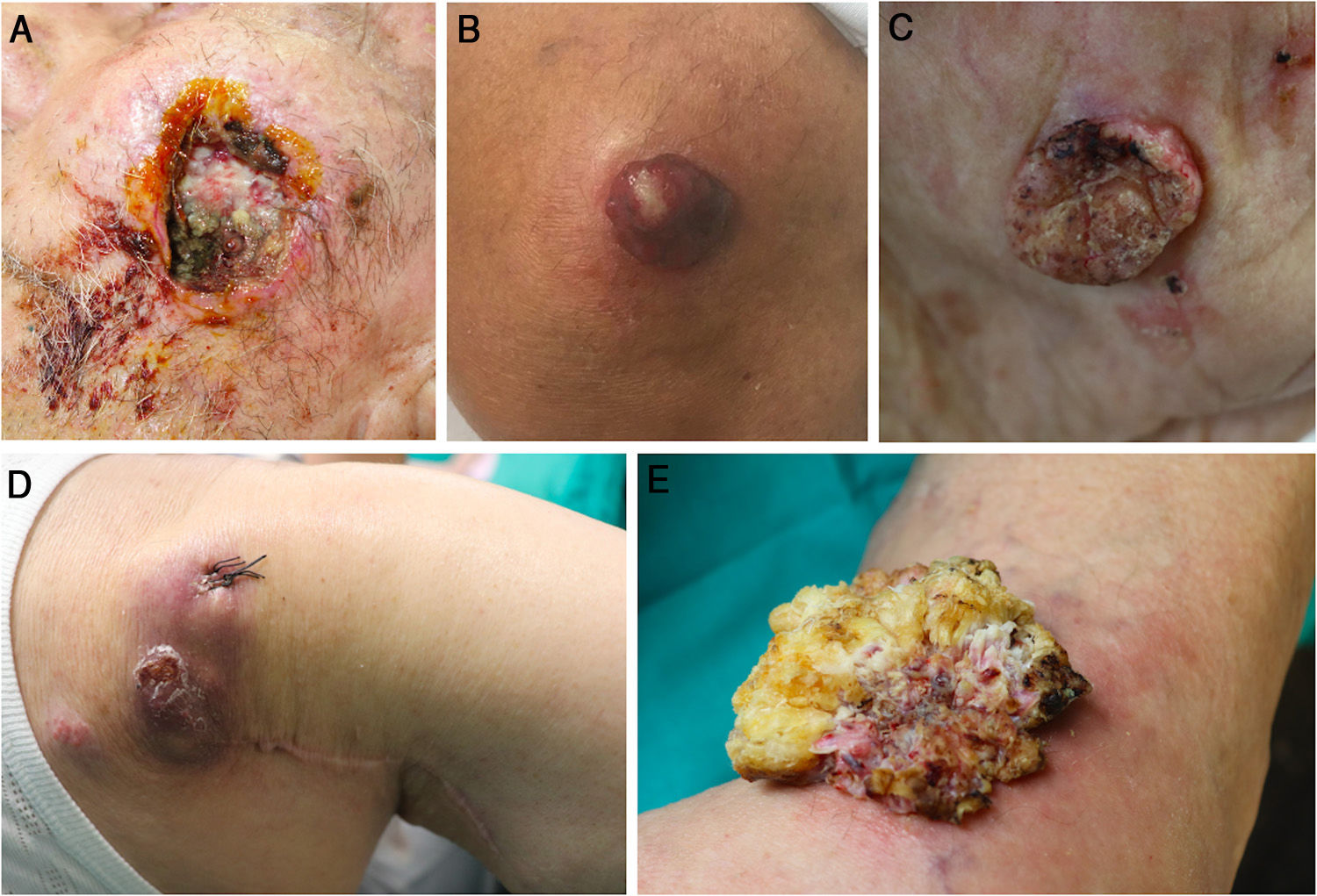
Nineteen patients (8 women and 11 men) with a mean age of 79 years were initially included. Two patients were excluded following histologic confirmation of an in situ tumor (BCC in one case and SCC in the other). The clinical diagnoses were 12 SCCs/keratoacanthomas, 1 verrucous carcinoma, 5 melanomas, and 1 Merkel cell carcinoma (MCC) (Fig. 1). Following histology, the diagnoses were 8 SCCs, 2 keratoacanthomas, 1 verrucous carcinoma, 4 melanomas, 1 MCC, 2 BCCs, and 1 hypertrophic actinic keratosis. Seventeen of the tumors (89%) were primary tumors and 2 were recurrences (1 MMC, treated medically and 1 SCC, treated palliatively). Seven of the 10 SCCs were classified as high-risk according to the criteria proposed by Cañueto et al.1 (Table 1). The questionnaire to evaluate patient attitudes was completed by 16 patients. Ten patients (62.5%) had had an earlier appointment to evaluate their lesion, but it had been cancelled due to lockdown. Among the reasons given for not seeking care earlier, 5 had not thought their lesion to be important and 7 had had their appointment cancelled. Four patients mentioned home confinement restrictions, not being allowed to go the hospital by their families, or being afraid of becoming infected at the hospital. In answer to the question, “Why are you consulting about your lesion now?”, 8 patients said that they were scared, 5 that they had an appointment, 4 that they had associated symptoms, and 1 that the lockdown restrictions had been eased. Twelve of the lesions (75%) had associated symptoms, mainly pain (n = 5) or itching (n = 4). Thirteen of the patients (81%) had been previously seen by a health care professional (a general practitioner in 62.5% of cases). Eight patients had been referred from emergency care. The origin of the other patients was teledermatology (n = 1), primary care (n = 3), an appointment from before lockdown (n = 2), another hospital department (n = 1), and a private clinic (n = 1). Finally, 68.7% of the patients said that under normal circumstances they would have sought care earlier (Table 2). The findings of this study show that 62.5% of patients with a high-risk malignant skin tumor received a delayed diagnosis because of the cancellation of an appointment at our dermatology department due to the COVID-19 state of emergency. Tejera-Vaquerizo and colleagues recently estimated that diagnostic and treatment delays in patients with skin tumors could lead to thicker tumors, increased mortality,3 and higher health care costs.4 Seventy percent of the SCCs in our series were classified as high-risk, but this high proportion is probably related to the inclusion criteria. It is noteworthy that 5 patients did not seek care earlier because they were not worried about their lesion, indicating that some members of the population are still unaware of the importance of early skin cancer diagnosis and highlighting the important role that general practitioners and teledermatology have in the early detection of high-risk skin tumors. Fifty percent of patients went directly to the emergency department to consult about their lesion. Just 25% were referred through primary care or teledermatology. This low rate is probably due to the exceptional circumstances, as most primary care centers were busy providing care to patients with COVID-19. Our findings also show the important role played by dermatologists in emergency departments. Seventy-five percent of patients had associated symptoms, which in some cases (e.g., pain in SCC) is associated with a poor prognosis.1 Nonetheless, just 4 patients sought care because of symptoms.
Clinical images of 5 of the skin tumors from this study. A, recurrent squamous cell carcinoma on the cheek with clinical perineural invasion. B, Superficial spreading melanoma on the knee with a Breslow thickness of 7.70 mm. C, Invasive squamous cell carcinoma on the cheek with a thickness of 6.5 mm. D, Recurrent Merkel cell carcinoma on the right shoulder. E, Verrucous carcinoma with a 5-cm diameter on the knee.
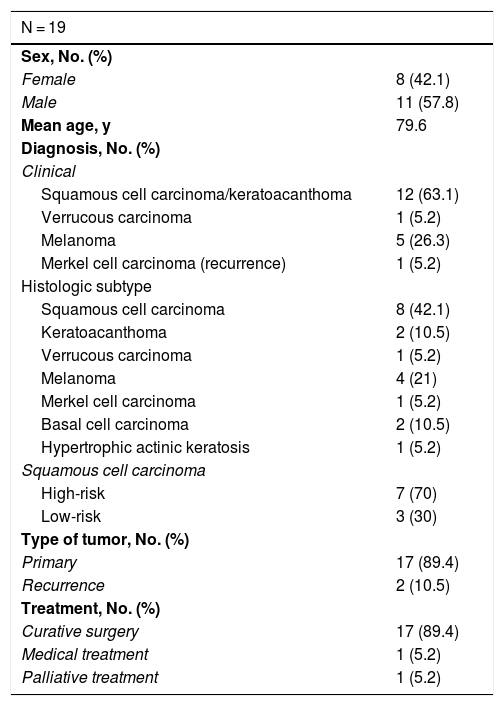
Baseline Characteristics of Patients and Tumors.
| N = 19 | |
|---|---|
| Sex, No. (%) | |
| Female | 8 (42.1) |
| Male | 11 (57.8) |
| Mean age, y | 79.6 |
| Diagnosis, No. (%) | |
| Clinical | |
| Squamous cell carcinoma/keratoacanthoma | 12 (63.1) |
| Verrucous carcinoma | 1 (5.2) |
| Melanoma | 5 (26.3) |
| Merkel cell carcinoma (recurrence) | 1 (5.2) |
| Histologic subtype | |
| Squamous cell carcinoma | 8 (42.1) |
| Keratoacanthoma | 2 (10.5) |
| Verrucous carcinoma | 1 (5.2) |
| Melanoma | 4 (21) |
| Merkel cell carcinoma | 1 (5.2) |
| Basal cell carcinoma | 2 (10.5) |
| Hypertrophic actinic keratosis | 1 (5.2) |
| Squamous cell carcinoma | |
| High-risk | 7 (70) |
| Low-risk | 3 (30) |
| Type of tumor, No. (%) | |
| Primary | 17 (89.4) |
| Recurrence | 2 (10.5) |
| Treatment, No. (%) | |
| Curative surgery | 17 (89.4) |
| Medical treatment | 1 (5.2) |
| Palliative treatment | 1 (5.2) |
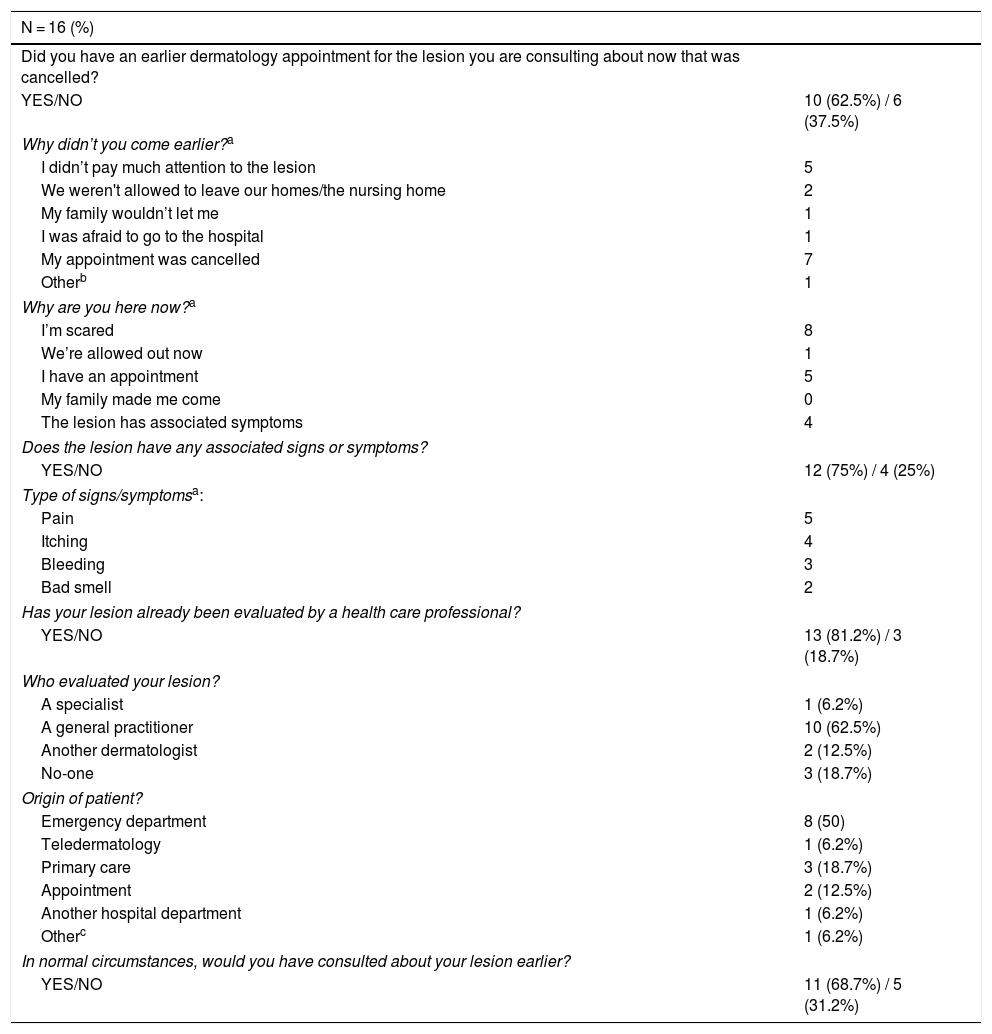
Summary of Survey Answers.
| N = 16 (%) | |
|---|---|
| Did you have an earlier dermatology appointment for the lesion you are consulting about now that was cancelled? | |
| YES/NO | 10 (62.5%) / 6 (37.5%) |
| Why didn’t you come earlier?a | |
| I didn’t pay much attention to the lesion | 5 |
| We weren't allowed to leave our homes/the nursing home | 2 |
| My family wouldn’t let me | 1 |
| I was afraid to go to the hospital | 1 |
| My appointment was cancelled | 7 |
| Otherb | 1 |
| Why are you here now?a | |
| I’m scared | 8 |
| We’re allowed out now | 1 |
| I have an appointment | 5 |
| My family made me come | 0 |
| The lesion has associated symptoms | 4 |
| Does the lesion have any associated signs or symptoms? | |
| YES/NO | 12 (75%) / 4 (25%) |
| Type of signs/symptomsa: | |
| Pain | 5 |
| Itching | 4 |
| Bleeding | 3 |
| Bad smell | 2 |
| Has your lesion already been evaluated by a health care professional? | |
| YES/NO | 13 (81.2%) / 3 (18.7%) |
| Who evaluated your lesion? | |
| A specialist | 1 (6.2%) |
| A general practitioner | 10 (62.5%) |
| Another dermatologist | 2 (12.5%) |
| No-one | 3 (18.7%) |
| Origin of patient? | |
| Emergency department | 8 (50) |
| Teledermatology | 1 (6.2%) |
| Primary care | 3 (18.7%) |
| Appointment | 2 (12.5%) |
| Another hospital department | 1 (6.2%) |
| Otherc | 1 (6.2%) |
| In normal circumstances, would you have consulted about your lesion earlier? | |
| YES/NO | 11 (68.7%) / 5 (31.2%) |
Seventy-percent of patients with a high-risk skin tumor did not seek necessary medical care during the COVID-19 state of emergency because of home confinement, cancelled appointments, or fear of infection. Our findings highlight the growing importance of image-based systems in dermatology and particularly within systems designed to facilitate the early diagnosis of skin tumors. They also demonstrate how dermatologists play an essential role in emergency departments by facilitating an early diagnosis of many skin disorders.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Porcar Saura S, Pons Benavent M, Guillén Climent S, García Vázquez A. Actitud de los pacientes con tumores cutáneos durante la pandemia de la COVID-19. Actas Dermosifiliogr. 2021;112:195–198.