Glossodynia is a medical disease of unknown etiology and pathogenesis, in which interest has grown in the last decade. Its exact prevalence is not known, but is estimated to be between 0.7% and 15% of the general population; it is most common in postmenopausal women.1 Glossodynia is defined clinically as a subjective sensation of burning, soreness, or pain that occurs daily and may occasionally be associated with dysgeusia or xerostomia, with no detectable lesions on the oral mucosa. The condition is characterized by its chronic course, the absence of local or systemic disease, and the high prevalence of psychiatric comorbidities, the most common of which are depression and anxiety.2
No guidelines exist regarding treatment. However, a number of therapeutic alternatives have been employed, based on scant scientific evidence of limited quality, with modest results. The results of clinical trials are difficult to compare because of the lack of uniformity of patient selection criteria, treatments, doses, and therapeutic response measures.3
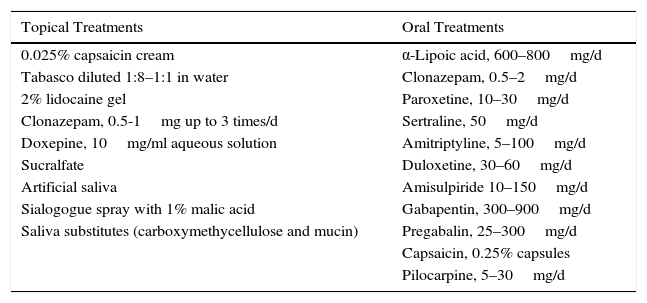
The various topical and oral treatments that have been used are summarized in Table 1. The treatments with greatest scientific evidence are currently α-lipoic acid and clonazepam.3
Most Widely Used Therapeutic Options Described in the Literature.
| Topical Treatments | Oral Treatments |
|---|---|
| 0.025% capsaicin cream | α-Lipoic acid, 600–800mg/d |
| Tabasco diluted 1:8–1:1 in water | Clonazepam, 0.5–2mg/d |
| 2% lidocaine gel | Paroxetine, 10–30mg/d |
| Clonazepam, 0.5-1mg up to 3 times/d | Sertraline, 50mg/d |
| Doxepine, 10mg/ml aqueous solution | Amitriptyline, 5–100mg/d |
| Sucralfate | Duloxetine, 30–60mg/d |
| Artificial saliva | Amisulpiride 10–150mg/d |
| Sialogogue spray with 1% malic acid | Gabapentin, 300–900mg/d |
| Saliva substitutes (carboxymethycellulose and mucin) | Pregabalin, 25–300mg/d |
| Capsaicin, 0.25% capsules | |
| Pilocarpine, 5–30mg/d |
α-Lipoic acid is an antioxidant and neuroprotective agent that, at a dose of 600mg/d, has been shown to provide a short-term improvement of symptoms, with an efficacy between 55% and 90%, depending on the study.3,4 Clonazepam can lead to partial improvement, between 70% and 80%, with a duration of effect of 6 months.3,5 Factors predicting a better therapeutic response to clonazepam include increased saliva flow, more intense symptoms, and the absence of concomitant use of other psychotropic drugs.1
A 6-month course of cognitive therapy has been useful in reducing symptom intensity in 27% of patients.3
Selective serotonin reuptake inhibitors (SSRI), including paroxetine and sertraline, can be useful in patients with associated depression; higher levels of evidence are found for paroxetine, with a partial response in 80% of patients after 12 weeks. Another advantage of the SSRIs is the absence of anticholinergic effects, such as dryness of the mouth.1
The tricyclic antidepressants, such as amitriptyline and nortriptyline, and dual inhibitors, such as duloxetine, are often used in neuropathic disorders, and it has been suggested that they may be effective, but no studies are available to support this assertion.3
Nor do studies exist to support the efficacy of gabapentin and pregabalin.
Several studies show a partial improvement with topical 0.02% capsaicin due to blockade of substance P. This can be given as mouthrinses with tabasco dissolved in water in a ratio between 1:8 and 1:1, though results are not highly significant.1,4
In conclusion, glossodynia is a common cause for consultation. Management is complex and should be multidisciplinary, with a group of specialists in which the dermatologist is a key element. Data available at the present time are insufficient to establish specific management recommendations, and individualized treatment will vary according to patient characteristics, comorbid conditions, duration and intensity of the symptoms, and the presence of xerostomia.
Please cite this article as: Cembrero-Saralegui H, Imbernón-Moya A. FR–Glosodinia: novedades terapéuticas. Actas Dermosifiliogr. 2017;108:63–64.