The incidence of lymphogranuloma venereum (LGV) — a sexually transmitted infection (STI) produced by the L1, L2, and L3 serovars of Chlamydia trachomatis — is increasing. The 8 patients in this case series were diagnosed with LGV in the STI unit of our dermatology department. Our patients were younger than those in previously published case series, and on presentation they most often complained of tumorous masses (lymphadenopathy) in the groin. Dermatologists should be familiar with this disease. Samples must be taken correctly to ensure an accurate diagnosis and early treatment.
El linfogranuloma venéreo (LGV) es una infección de transmisión sexual (ITS) producida por los serovares L1, L2 y L3 de la bacteria Chlamydia trachomatis y cuya incidencia está en aumento. Presentamos una serie de 8 pacientes diagnosticados en nuestra Unidad de ITS del Servicio de Dermatología. La edad de nuestros pacientes es menor que en otras series publicadas y el síntoma más frecuente de presentación es la tumoración adenopática inguinal. El dermatólogo debe conocer esta patología y realizar una correcta toma de muestras para un diagnóstico preciso y un tratamiento precoz.
Lymphogranuloma venereum (LGV) is a sexually transmitted disease (STD) caused by the L1, L2, and L3 serovars of the Chlamydia trachomatis (CT) bacterium. This disease, common in tropical and subtropical areas, occurred only infrequently in Europe before 2003.1 Subsequently, its incidence has increased considerably driven by outbreaks, particularly among men who have sex with men (MSM), to the extent it became a notifiable disease (ND) in 2008 in the European Union and in 2015 in Spain.2
According to the study by Asunción Díaz et al.,2 from 2005 to 2015, prior to modification of epidemiologic surveillance at the national level, cases of LGV were published in 7 autonomous communities in Spain: Andalusia, Asturias, Catalonia, Canarias, Madrid, Valencia, and Basque Country. Catalonia was the autonomous community with most cases, 597 in total, given that LGV has been considered an ND since 2007 in that region. The Madrid region had 136 cases. In the remaining autonomous communities, the number of cases reported was lower, ranging from 2 cases in the Basque Country in 2006 to 15 in Andalusia between 2013 and 2015. The Valencia region only reported 1 case.
According to the Spanish Epidemiologic Surveillance Network, in 2016, 248 cases of LGV were reported, one of which was in the Valencia region.3 The objective of this study was to assess the clinical and epidemiological characteristics of patients diagnosed with LGV in our dermatology department from January 2017 through December 2018, after the STD Unit (abbreviated as UITS) was established in the General University Hospital, Valencia, Spain.
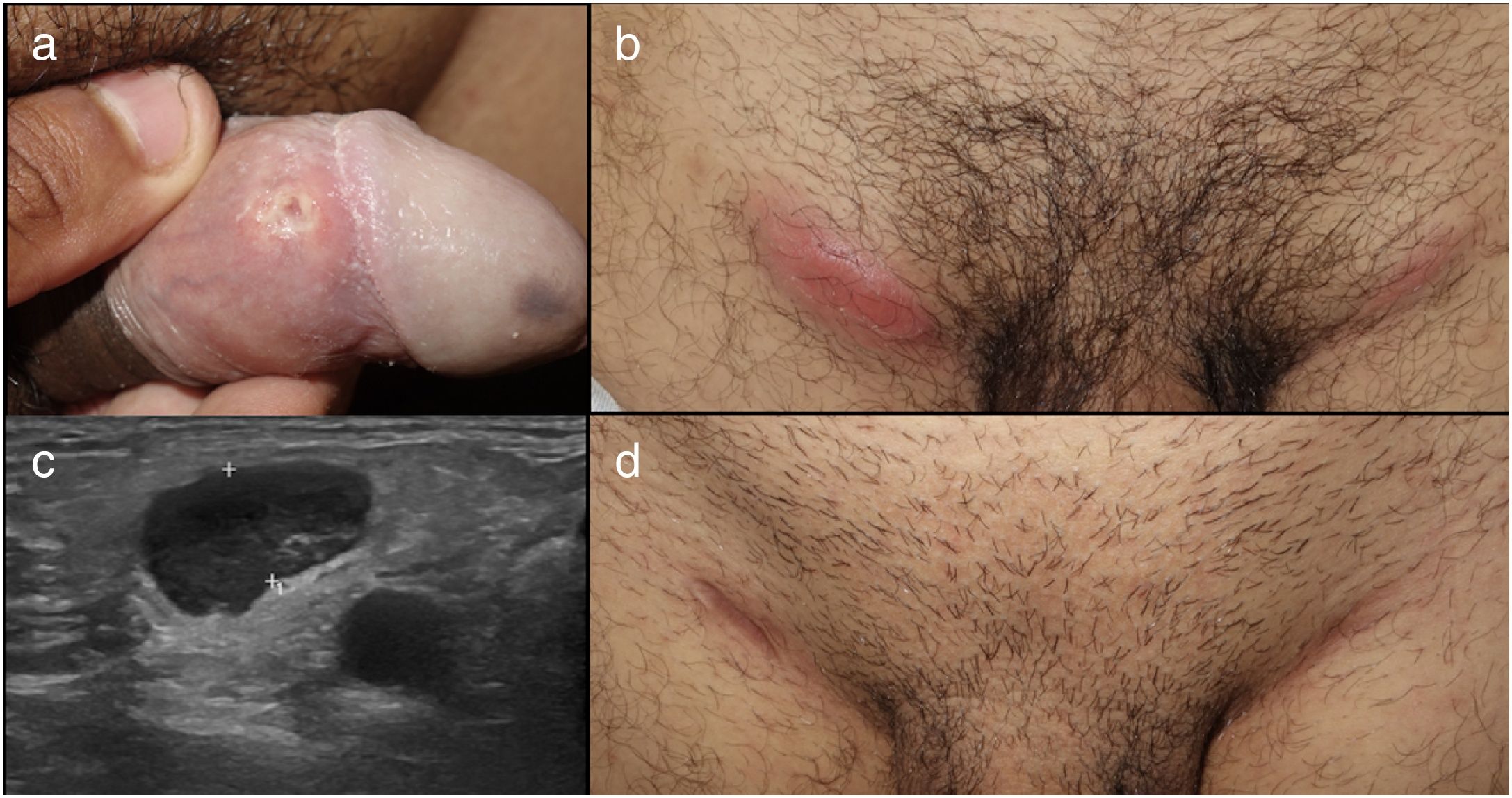
In this period, we have diagnosed a total of 644 cases of STDs in our unit, with the most frequent being condyloma acuminata (37%), urethritis (19%), genital herpes (13.6%), and syphilis (12.6%). A total of 8 cases of LGV were diagnosed (1.2%). The 8 patients were male (1 currently a transexual woman), with a mean (SD) age of 27.25 (7) years. The clinical-epidemiologic characteristics are summarized in Table 1. Patient 3 is illustrated in Fig. 1. All patients except 1 were referred to the UITS as dermatological emergencies. The other, the only 1 who was HIV positive, was referred from the general emergency department, and was initially assessed by the infectious diseases department. After diagnosis of LGV, 2 patients were diagnosed with another concomitant STD (one of them proctitis also associated with Mycoplasma genitalium and another with a primary HIV infection and syphilis reinfection).
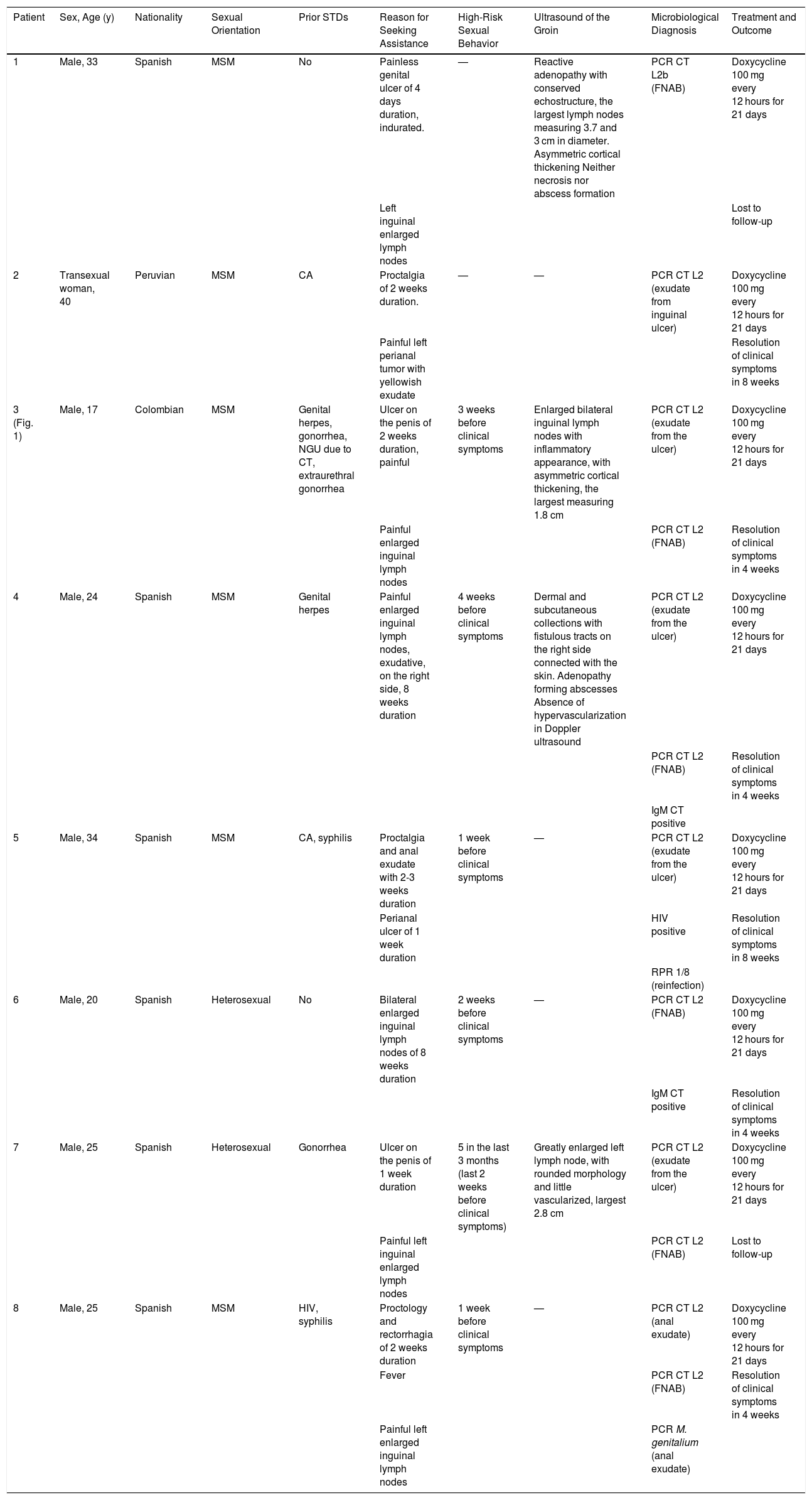
Clinical-Epidemiological Characteristics of Patients Diagnosed with LGV in Our STD Unit.
| Patient | Sex, Age (y) | Nationality | Sexual Orientation | Prior STDs | Reason for Seeking Assistance | High-Risk Sexual Behavior | Ultrasound of the Groin | Microbiological Diagnosis | Treatment and Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Male, 33 | Spanish | MSM | No | Painless genital ulcer of 4 days duration, indurated. | — | Reactive adenopathy with conserved echostructure, the largest lymph nodes measuring 3.7 and 3 cm in diameter. Asymmetric cortical thickening Neither necrosis nor abscess formation | PCR CT L2b (FNAB) | Doxycycline 100 mg every 12 hours for 21 days |
| Left inguinal enlarged lymph nodes | Lost to follow-up | ||||||||
| 2 | Transexual woman, 40 | Peruvian | MSM | CA | Proctalgia of 2 weeks duration. | — | — | PCR CT L2 (exudate from inguinal ulcer) | Doxycycline 100 mg every 12 hours for 21 days |
| Painful left perianal tumor with yellowish exudate | Resolution of clinical symptoms in 8 weeks | ||||||||
| 3 (Fig. 1) | Male, 17 | Colombian | MSM | Genital herpes, gonorrhea, NGU due to CT, extraurethral gonorrhea | Ulcer on the penis of 2 weeks duration, painful | 3 weeks before clinical symptoms | Enlarged bilateral inguinal lymph nodes with inflammatory appearance, with asymmetric cortical thickening, the largest measuring 1.8 cm | PCR CT L2 (exudate from the ulcer) | Doxycycline 100 mg every 12 hours for 21 days |
| Painful enlarged inguinal lymph nodes | PCR CT L2 (FNAB) | Resolution of clinical symptoms in 4 weeks | |||||||
| 4 | Male, 24 | Spanish | MSM | Genital herpes | Painful enlarged inguinal lymph nodes, exudative, on the right side, 8 weeks duration | 4 weeks before clinical symptoms | Dermal and subcutaneous collections with fistulous tracts on the right side connected with the skin. Adenopathy forming abscesses Absence of hypervascularization in Doppler ultrasound | PCR CT L2 (exudate from the ulcer) | Doxycycline 100 mg every 12 hours for 21 days |
| PCR CT L2 (FNAB) | Resolution of clinical symptoms in 4 weeks | ||||||||
| IgM CT positive | |||||||||
| 5 | Male, 34 | Spanish | MSM | CA, syphilis | Proctalgia and anal exudate with 2-3 weeks duration | 1 week before clinical symptoms | — | PCR CT L2 (exudate from the ulcer) | Doxycycline 100 mg every 12 hours for 21 days |
| Perianal ulcer of 1 week duration | HIV positive | Resolution of clinical symptoms in 8 weeks | |||||||
| RPR 1/8 (reinfection) | |||||||||
| 6 | Male, 20 | Spanish | Heterosexual | No | Bilateral enlarged inguinal lymph nodes of 8 weeks duration | 2 weeks before clinical symptoms | — | PCR CT L2 (FNAB) | Doxycycline 100 mg every 12 hours for 21 days |
| IgM CT positive | Resolution of clinical symptoms in 4 weeks | ||||||||
| 7 | Male, 25 | Spanish | Heterosexual | Gonorrhea | Ulcer on the penis of 1 week duration | 5 in the last 3 months (last 2 weeks before clinical symptoms) | Greatly enlarged left lymph node, with rounded morphology and little vascularized, largest 2.8 cm | PCR CT L2 (exudate from the ulcer) | Doxycycline 100 mg every 12 hours for 21 days |
| Painful left inguinal enlarged lymph nodes | PCR CT L2 (FNAB) | Lost to follow-up | |||||||
| 8 | Male, 25 | Spanish | MSM | HIV, syphilis | Proctology and rectorrhagia of 2 weeks duration | 1 week before clinical symptoms | — | PCR CT L2 (anal exudate) | Doxycycline 100 mg every 12 hours for 21 days |
| Fever | PCR CT L2 (FNAB) | Resolution of clinical symptoms in 4 weeks | |||||||
| Painful left enlarged inguinal lymph nodes | PCR M. genitalium (anal exudate) |
Abbreviations: CA, condyloma acuminata; CT, Chlamydia trachomatis; FNAB, fine needle aspiration biopsy; HIV, human immunodeficiency virus; MSM, men who have sex with men; NGU, nongonococcal urethritis; STD, sexually transmitted disease; M. genitalium, Mycoplasma genitalium.
Patient 3 with painful genital ulcer on the inner face of the foreskin (a) associated with painful bilateral inflammatory adenopathy in the groin (b). Ultrasound of the groin showed greatly enlarged lymph nodes with cortical asymmetry and limited vascularization. After treatment with doxycycline 100 mg every 12 hours for 21 days, lymph node enlargement reduced leaving a residual scar.
Ultrasound of the groin was performed in 4 patients before microbiological diagnosis. Definitive diagnosis was established in all cases by detecting DNA of CT L1-L2-L3 serovars by polymerase chain reaction (PCR) in exudate from the ulcer (5 cases), anal exudate (1 case), or fine-needle aspiration biopsy (FNAB) samples of an enlarged lymph node (6 cases). In all cases, the samples were taken at the time of the first visit. In all patients, the L2 serovar was isolated and in 3, biopsy was performed for histopathologic study. In the samples, epithelial ulcer was observed with a dense lymphoplasmacytic infiltrate occupying the full thickness of the dermis. Immunohistochemistry for Treponema pallidum was negative in all cases.
All patients received treatment with oral doxycycline 100 mg every 12 hours for 21 days, with resolution of the signs and symptoms within 4-8 weeks (except for 2 patients who were lost to follow-up).
LGV is an uncommon STD that can cause genital-inguinal or anorectal disease depending on how infection occurred. Infection is initially manifest in the form of a papule or herpetiform and usually painless lesions. The primary lesion usually appears between 3 and 30 days after contact. Often, primary lesions can go unnoticed given that they heal quickly with no or minimal scarring or because of their extragenital site.4 Rectal exposure can cause proctalgia which may or may not be associated with anal exudate as the most frequent symptom. After 2-6 weeks, the secondary stage of the disease is manifest with regional lymph node involvement, leading to painful inflammation of the inguinal or femoral lymph nodes. This inflammation is usually unilateral and results in suppuration, fistulous tracts, and/or abscesses. During this phase, general symptoms such as low fever, shivers, myalgia, and arthralgia may occur.5 LGV, like other ulcerated STDs, increases susceptibility to other STDs, such as HIV, as was detected in one of our 8 patients.
In agreement with previously published data in Spain, most cases occurred in Spanish MSM.2 The mean age was 27 years, which is slightly lower than that reported previously, with a range of 30 to 45 years; this difference can be attributed to young adults having sex at an increasingly young age in recent years with a lower condom usage.6 Unlike some of the publications in Spain, only 1 of our patients (12.5%) had prior HIV infection compared with approximately 30% to 60% of HIV-positive patients with a diagnosis of LGV.2 This prevalence increases in cases of proctitis caused by LGV.7 Moreno-Ribera et al.8 reported a total of 38 cases of LGV in their UITS over 4 years, all in MSM and more than 90% of them HIV-positive.
The most frequent symptom in our series was inguinal tumor corresponding to a secondary stage of the disease in 5 patients, 1 of them associated with a painless genital ulcer. This differs from the studies published with most number of patients, in which the main symptom is proctitis or proctocolitis9 even though the proportion of MSM patients is similar. Moreno-Ribera et al.8 reported that 86% of their patients diagnosed with LGV had clinical symptoms of proctitis. At times, the primary stage can go unnoticed (in almost 30% of cases), with LGV diagnosis occurring later.2 Of the 5 cases with genital-inguinal disease, the lesions were unnoticed in 2 (40%) of them. It is important to screen for other concomitant STDs. In our study, 2 of the 8 patients (25%) had an infection associated with LGV. This percentage is somewhat lower than in other published studies, where it is estimated that 46% of patients can present with coinfection.7
Historically, diagnosis of LGV was based on clinical presentation along with appropriate serologic findings. However, the criteria for interpretation of serologic tests have not been standardized and so new molecular methods have been developed to confirm LGV infection from clinical samples (particularly anorectal biopsies in MSM or FNAB of enlarged lymph nodes). These methods focus on confirming the serovars associated with LGV by sequencing the outer membrane protein A (ompA) gene or through real-time PCR to identify a deletion specific to L2b on the polymorphic membrane protein H (pmpH) gene. It is not sufficient to confirm infection by CT by the routinely available nucleic acid amplification tests as they are positive for chlamydia infections both in patients with LGV and those without.5
In terms of treatment, clinical guidelines support the use of doxycycline 100 mg twice a day for 21 days as treatment of choice for LGV. The 3-week duration is chosen because LGV infections are more invasive and difficult to eradicate than other non-LGV CT infections.1 Erythromycin, 500 mg 4 times a day for 21 days is an alternative treatment shown to be effective, although gastrointestinal intolerance and dosing may limit its usefulness. In addition to antibiotic therapy, local drainage of lesions could also be considered to prevent the development of ulceration or fistulous tracts. The treatment is the same for patients with HIV infection, although they may take longer to respond to treatment.5
In conclusion, we should also highlight the importance of dermatologists in the management of STD; this is a key part of our specialty. Although this is an uncommon disease, the incidence of LGV is increasing and often the dermatologist is the point of access to the healthcare system for these patients. It is essential to ensure that samples are correctly taken at the time of the first visit, including FNAB in the case of enlarged lymph nodes, as this is often the only opportunity we will have to confirm diagnosis as some patients never return to the clinic. It is of utmost importance that dermatologists have a high index of suspicion to avoid delays in diagnosis and treatment; this is key for the patient and also for breaking the chain of transmission.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Magdaleno-Tapial J, Hernández-Bel P, Valenzuela-Oñate C, Ocete-Mochon MD, Pérez-Ferriols A. El resurgir del linfogranuloma venéreo, una enfermedad que el dermatólogo debería conocer. Actas Dermosifiliogr. 2021;112:453–457.