Understanding the origin and referral routes of patients seen in teledermatology and in-person dermatology consultations in Spain is of interest from the perspective of health care management. The objective of this study was to describe the referral routes and the frequency and characteristics of teledermatology consultations in Spain.
Material and methodsWe performed a descriptive cross-sectional study of data collected over 6 days from the DIADERM study sample, which included the outpatients diagnosed by 80 Spanish dermatologists, selected by means of stratified random sampling. We studied the source and destination of patients based on funding, type of consultation, and age of the patients. We reported the frequency of teledermatology consultations, their origin and destination, type of funding, age of the patients, and most common diagnoses, and compared them with the same characteristics for in-person consultations.
ResultsIn private consultations, most patients were direct clients, whereas the most frequent source in public consultations was primary care and the dermatologist. Sixty-six percent of patients were referred to dermatology and 27% were discharged. No differences in these percentages were found between public and private consultations. The ratio of follow-up to initial visits was 0.8 for public consultations and 0.2 for private consultations. Teledermatology accounts for 1% of consultations. Eighty percent of these come from primary care and 17% are direct visits. Thirty-three percent of these visits are referred to primary care —a greater proportion than in in-person consultations. Galicia, Andalusia, and Catalonia are the regions with the highest percentage of consultations.
ConclusionsThe results suggest that dermatologists in Spain have a considerable ability to resolve cases. Teledermatology accounts for a small percentage of consultations and access to these consultations is direct in a large percentage of cases.
El conocimiento de las rutas de origen y derivación de los pacientes atendidos en consulta dermatológica presencial y de teledermatología en España tiene interés desde el punto de vista de la gestión sanitaria. El objetivo de este estudio es describir las rutas de derivación y la frecuencia y características de la teledermatología en España.
Material y métodosEstudio transversal descriptivo sobre la muestra del estudio DIADERM, que recogió la actividad de 80 dermatólogos españoles, seleccionados mediante muestreo aleatorio estratificado, durante 6 días. Se estudiaron el origen y destino de los pacientes en función de la financiación, el tipo de consulta y la edad de los pacientes. Se describió la frecuencia de las consultas por teledermatología, su origen y destino, el tipo de financiación, la edad de los pacientes y los diagnósticos más frecuentes, comparándolos con la consulta presencial.
ResultadosEl origen más frecuente en la consulta privada es el directo, mientras que en la pública es la atención primaria y el propio dermatólogo. Un 66% de los pacientes se derivan a dermatología y un 27% son dados de alta. No existen diferencias en estos porcentajes entre consulta pública y privada. El índice sucesivas/primeras fue de 0,8 para la consulta pública y de 0,2 para la privada. La teledermatología representa un 1% de las consultas. El 80% procede de atención primaria y el 17% tiene origen directo. Se deriva a atención primaria el 33%, en mayor proporción que en consulta presencial. Galicia, Andalucía y Cataluña son las regiones donde representa un mayor porcentaje de consultas.
ConclusionesLos resultados sugieren una alta capacidad resolutiva de las consultas de dermatología en España. La teledermatología representa un porcentaje pequeño de las consultas, y el acceso a ella se da en un porcentaje relevante de pacientes por vía directa.
The DIADERM study was performed in 2016 to report on outpatient dermatology care in Spain.1 The study revealed that most patients were referred to the dermatology clinic via the dermatologist (34% of cases), followed by the primary care physician. Similarly, the most common destination after the consultation was the dermatologist, and most visits resulted in discharge.1 However, these referral routes may depend on other variables, such as patient age, whether the clinic is private or public, and whether the clinic is a specialist center. In terms of health care management, it is particularly interesting to study referral routes with respect to these variables and the percentage of consultations that lead to discharge. The destination of dermatology patients has been reported in other countries2; however, equivalent data are lacking in Spain.
In teledermatology, that is, distance health care using telecommunication technology,3 knowledge of referral routes can serve as an indicator of the use of this care modality in Spain. Many studies have shown that teledermatology can reduce waiting lists, act as a triage service for referrals from primary care, and ensure easy access to specialized care from remote locations.4–10 Spain has one of the highest frequencies of publications on teledermatology,11 which is a growing modality for consultation in Spain. In 2014, it was used by 70 centers, ie, more than 25% of all public dermatology clinics in Spain.12 Data from DIADERM enabled us to report on teledermatology referral routes and their characteristics.
The objective of the present study was to describe referral routes for patients seen in dermatology outpatient clinics in Spain and to report on the frequency and characteristics of teledermatology consultations in Spain.
Material and MethodsStudy Design and SampleWe performed a descriptive cross-sectional study.
The reference population comprised patients who attended a dermatology outpatient clinic in Spain. The data were obtained from the DIADERM study.1 In summary, we collected a sample of 8832 patients who consulted with 80 Spanish dermatologists selected using stratified random sampling. Data were collected twice during the year 2016 (3 consecutive days in January and 3 in May). The unit of analysis was the patient. We reported on the dermatologists’ activity, both in public and in private centers.
Study Variables and Statistical AnalysisWe collected the origin and destination of each patient seen at the clinic.1 Origin was classified as follows: direct with no previous consultation; referred from primary care; and referred from another specialist or from the dermatology department (including, with no distinctions between them, check-ups or referrals from another dermatologist from the same or another center). The destination was classified by the respondent as discharge with no further follow-up, discharge with follow-up in primary care, referral to another specialist, or follow-up in the dermatology department, including surgery.
The origin of the patients was studied according to the following variables: public or private consultation; specialist consultation (citing patients with the same disease or group of diseases) or general consultation; or consultation for patients aged < 18 years. The most common diagnoses were recorded based on these variables in order to determine whether they could affect referral routes. Similarly, the destinations were studied based on the abovementioned variables, as was the destination according to whether the patient was attending his/her first visit (understood as not being a referral from a dermatologist) or not. The routes of origin and destination were compared according to whether these variables were present or not.
We calculated the frequency of patients seen via teledermatology, whether the consultations were publicly or privately funded (with a private consultation understood to be one in which treatment could not be funded by the social security system or health insurance companies), age group, origin, and referral destination. These percentages were compared with those of patients seen at face-to-face visits. In the case of results for teledermatology, in addition to frequencies, we estimated the number of patients seen per month throughout Spain. We also recorded the most frequent diagnoses in teledermatology and face-to-face visits, as well as the percentage of consultations in each regional section of the Spanish Academy of Dermatology and Venereology (AEDV).
The statistical analysis was performed taking into account the design used to collect the sample. We used the survey command in Stata (StataCorp. 2015. Stata Statistical Software, Release 14, StataCorp LP), which provides standard errors for correlated data. Frequencies were expressed as percentages with their 95% confidence interval (CI). The comparisons were made using the χ2 test or Fisher exact test.
The DIADERM study was approved by the Research Ethics Committee of the Province of Granada, Spain.1
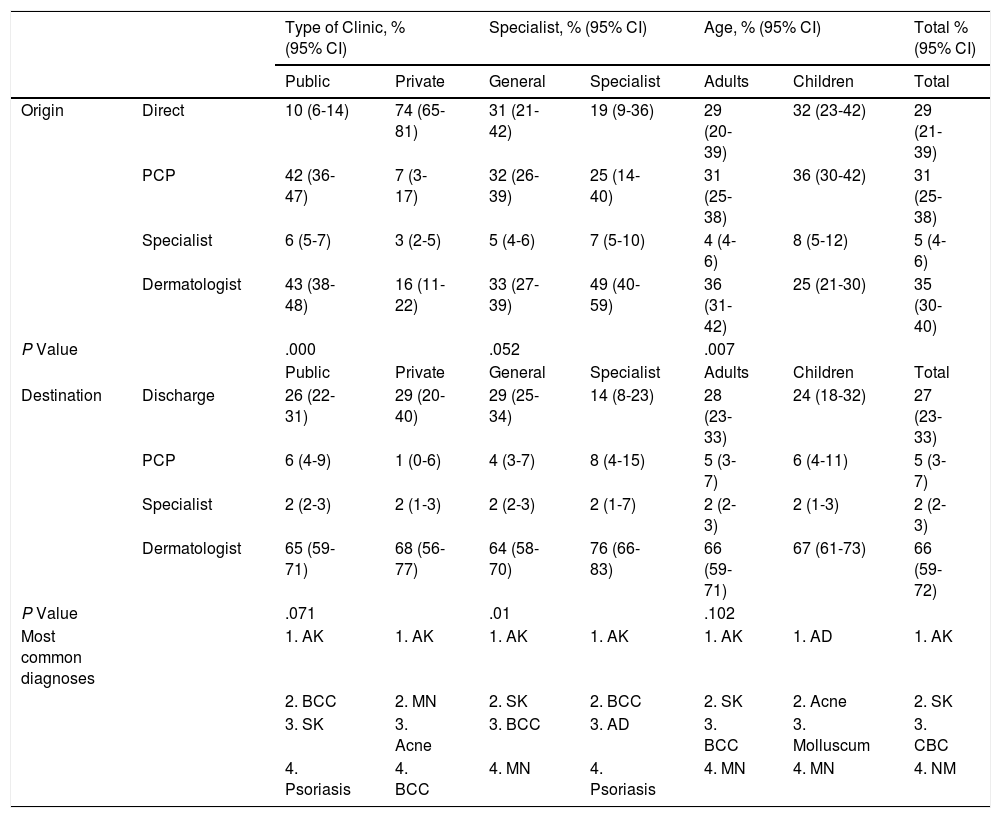
ResultsOriginTable 1 shows the origin of the patients according to the variables studied. In private consultations, most patients were direct clients (74% [95% CI, 65%-81%]), whereas the most frequent origin in public consultations was primary care or the dermatology department. The most frequent diagnosis in both cases was actinic keratosis. In specialist consultations, half of the patients were referred by a dermatologist, whereas in general consultations, primary care, direct origin, and referral by a dermatologist each accounted for around 30% of the patients, although the differences were not significant (Table 1). Primary care was the main origin for pediatric patients (36% [95% CI, 23%-42%]); the dermatologist was the main origin for adults (36% [95% CI, 31%-42%]).
Origin and Referral of Patients According to Other Variables.
| Type of Clinic, % (95% CI) | Specialist, % (95% CI) | Age, % (95% CI) | Total % (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| Public | Private | General | Specialist | Adults | Children | Total | ||
| Origin | Direct | 10 (6-14) | 74 (65-81) | 31 (21-42) | 19 (9-36) | 29 (20-39) | 32 (23-42) | 29 (21-39) |
| PCP | 42 (36-47) | 7 (3-17) | 32 (26-39) | 25 (14-40) | 31 (25-38) | 36 (30-42) | 31 (25-38) | |
| Specialist | 6 (5-7) | 3 (2-5) | 5 (4-6) | 7 (5-10) | 4 (4-6) | 8 (5-12) | 5 (4-6) | |
| Dermatologist | 43 (38-48) | 16 (11-22) | 33 (27-39) | 49 (40-59) | 36 (31-42) | 25 (21-30) | 35 (30-40) | |
| P Value | .000 | .052 | .007 | |||||
| Public | Private | General | Specialist | Adults | Children | Total | ||
| Destination | Discharge | 26 (22-31) | 29 (20-40) | 29 (25-34) | 14 (8-23) | 28 (23-33) | 24 (18-32) | 27 (23-33) |
| PCP | 6 (4-9) | 1 (0-6) | 4 (3-7) | 8 (4-15) | 5 (3-7) | 6 (4-11) | 5 (3-7) | |
| Specialist | 2 (2-3) | 2 (1-3) | 2 (2-3) | 2 (1-7) | 2 (2-3) | 2 (1-3) | 2 (2-3) | |
| Dermatologist | 65 (59-71) | 68 (56-77) | 64 (58-70) | 76 (66-83) | 66 (59-71) | 67 (61-73) | 66 (59-72) | |
| P Value | .071 | .01 | .102 | |||||
| Most common diagnoses | 1. AK | 1. AK | 1. AK | 1. AK | 1. AK | 1. AD | 1. AK | |
| 2. BCC | 2. MN | 2. SK | 2. BCC | 2. SK | 2. Acne | 2. SK | ||
| 3. SK | 3. Acne | 3. BCC | 3. AD | 3. BCC | 3. Molluscum | 3. CBC | ||
| 4. Psoriasis | 4. BCC | 4. MN | 4. Psoriasis | 4. MN | 4. MN | 4. NM | ||
Abbreviations: AD, atopic dermatitis; AK, actinic keratosis; BCC, basal cell carcinoma; CI, confidence interval; MN, melanocytic nevus; PCP, primary care physician; SK, seborrheic keratosis.
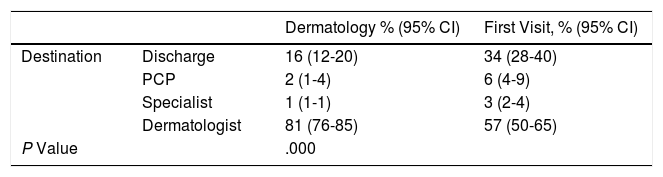
Table 1 shows the patients’ destinations according to the study variables. There were no differences in referral route according to patient age or how the consultation was funded, although significant differences were observed between specialist and general consultations, with discharges being less frequent in specialist consultations (Table 1). We also found significant differences between the origin and subsequent referral (Table 2).
Destination of New Patients Compared With Patients Referred From Dermatology.
| Dermatology % (95% CI) | First Visit, % (95% CI) | ||
|---|---|---|---|
| Destination | Discharge | 16 (12-20) | 34 (28-40) |
| PCP | 2 (1-4) | 6 (4-9) | |
| Specialist | 1 (1-1) | 3 (2-4) | |
| Dermatologist | 81 (76-85) | 57 (50-65) | |
| P Value | .000 | ||
Abbreviation: CI, confidence interval; PCP, primary care physician.
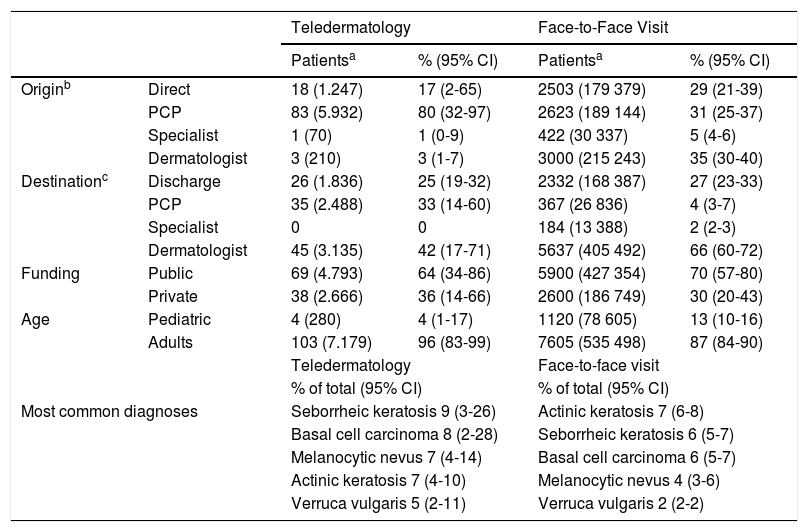
Teledermatology accounted for 1.2% of consultations (95% CI, 0.4%-3.7%), that is, 107 patients seen over the 6 days (estimated incidence of 7459 patients per month throughout Spain). Primary care was the origin for 80% of patients (Table 3); this differed significantly from that of patients seen at face-to-face visits (P=.015). The need for a further visit to the dermatologist was less common in patients seen via teledermatology than in those seen at face-to-face visits. Referral for follow-up by primary care was more frequent in teledermatology, although the percentage of discharges with no indication for follow-up was similar in both groups (Table 3).
Characteristics of Teledermatology Consultations.
| Teledermatology | Face-to-Face Visit | ||||
|---|---|---|---|---|---|
| Patientsa | % (95% CI) | Patientsa | % (95% CI) | ||
| Originb | Direct | 18 (1.247) | 17 (2-65) | 2503 (179 379) | 29 (21-39) |
| PCP | 83 (5.932) | 80 (32-97) | 2623 (189 144) | 31 (25-37) | |
| Specialist | 1 (70) | 1 (0-9) | 422 (30 337) | 5 (4-6) | |
| Dermatologist | 3 (210) | 3 (1-7) | 3000 (215 243) | 35 (30-40) | |
| Destinationc | Discharge | 26 (1.836) | 25 (19-32) | 2332 (168 387) | 27 (23-33) |
| PCP | 35 (2.488) | 33 (14-60) | 367 (26 836) | 4 (3-7) | |
| Specialist | 0 | 0 | 184 (13 388) | 2 (2-3) | |
| Dermatologist | 45 (3.135) | 42 (17-71) | 5637 (405 492) | 66 (60-72) | |
| Funding | Public | 69 (4.793) | 64 (34-86) | 5900 (427 354) | 70 (57-80) |
| Private | 38 (2.666) | 36 (14-66) | 2600 (186 749) | 30 (20-43) | |
| Age | Pediatric | 4 (280) | 4 (1-17) | 1120 (78 605) | 13 (10-16) |
| Adults | 103 (7.179) | 96 (83-99) | 7605 (535 498) | 87 (84-90) | |
| Teledermatology | Face-to-face visit | ||||
| % of total (95% CI) | % of total (95% CI) | ||||
| Most common diagnoses | Seborrheic keratosis 9 (3-26) | Actinic keratosis 7 (6-8) | |||
| Basal cell carcinoma 8 (2-28) | Seborrheic keratosis 6 (5-7) | ||||
| Melanocytic nevus 7 (4-14) | Basal cell carcinoma 6 (5-7) | ||||
| Actinic keratosis 7 (4-10) | Melanocytic nevus 4 (3-6) | ||||
| Verruca vulgaris 5 (2-11) | Verruca vulgaris 2 (2-2) | ||||
Abbreviation: PCP, primary care physician.
Approximately two-thirds of teledermatology patients are seen in the public health system, and 4% are aged < 18 years (95% CI, 1%-17%); these figures do not differ significantly from those of patients seen at face-to-face visits. Distance consultations were more frequent in Galicia (6% of all consultations), Catalonia (2%), and Andalucía (1%).
Teledermatology was used at some time by 15 of the 80 dermatologists (18.75%) during the 3 days in January and by 7 of 73 (9.59%) during the 3 days in May.
DiscussionThe DIADERM study made it possible to obtain a representative national overview of the origin and referral of patients attending dermatology outpatient clinics and of the use of teledermatology in Spain. The main origin for consultations at public centers was primary care and the dermatology clinic itself, since, in theory, direct access is not possible in this setting. Notwithstanding, it is striking that the origin was direct in 10%: some cases may correspond to patients referred from the emergency department (variable not collected). In private clinics, most patients were referred directly, and only 16% were from the dermatology department. This figure includes check-ups. Since direct access is—in theory—impossible in the public health system, it is important to remember that the difference we observed with private clinics is structural and necessarily imposed by the system. The high percentage recorded for direct origin in private clinics points to a high demand for dermatologic care in Spain, and we can assume that some of these patients have been seen by primary care physicians in the public health system.
The successive/first index—successive consultations divided by first consultations—is an indicator that is frequently used in health care management to evaluate the activity of outpatient clinics.13 This index helps to estimate the ability of a clinic to resolve cases, although it does not take into account possible re-entries of unresolved problems. In our study, if we assumed that all patients referred from the dermatologist are patients undergoing check-ups, we would have an index of 0.8 for public clinics and 0.2 for private clinics. These values point to a high ability to resolve cases, although it is striking that they do not agree with referrals, where, in both areas, 2 of every 3 patients undergo a check-up in the dermatology department. We cannot explain this observation, although it could be due to the fact that many check-ups are in the long term or many patients do not keep their appointments, especially in private centers. Similarly, the official statistics show a higher percentage of check-ups in private clinics (41%).14 However, the study population in this case is different, since it includes only polyvalent centers with major outpatient surgery or imaging-based diagnostic techniques, thus probably ruling out many of the private centers included in DIADERM.
Our data on destination can be compared with those of Bertanha et al,2 who analyzed the destination of patients seen at a triage dermatology clinic for new patients in Brazil and reported a similar figure for discharges (33%). Curiously, we did not find significant differences in destination between public and private clinics. This is paradoxical, given that, depending on the origin, we did find a potentially greater ability to resolve cases in private clinics (see above). As for type of clinic, the tendency toward discharge is lower in specialist clinics than in general clinics, probably because fewer new patients are seen in the former and the most frequent diagnoses are chronic or oncologic diseases (Table 1), which require additional follow-up.
Around 1% of the consultations were via telemedicine. This represents a small percentage of the total number of consultations, although we know from a recent study that teledermatology has been implemented in more than 25% of dermatology services in Spain.12 This figure is higher than in the USA, where a recent survey showed that 11% of dermatologists used teledermatology,15 and lower than in the UK, where the percentage was 48%.16 Teledermatology was more frequently used in Galicia, Catalonia, and Andalucía. These differences may be explained by the uneven implementation of the electronic clinical history,17 the interest shown by autonomous communities and hospitals, and the presence of teams of dermatologists interested in the field. The results of recent studies indicate that teledermatology is well implemented in these 3 autonomous communities, although Madrid is the community with the highest number of services using it.12 The finding that most patients were from primary care is as expected, given that teledermatology is more frequently used for triage in order to avoid unnecessary referrals and reduce waiting times.7,11 The origin was direct in 17% of patients, probably because of access to teledermatology via smartphone apps, although this was not investigated in our survey. A survey carried out in 2014 only analyzed the use of teledermatology in public centers12; therefore, it would be interesting to perform new studies to investigate the implementation of direct access teledermatology via apps in Spain. Funding and patient age did not differ significantly from those of the face-to-face visits.
The limitations of the study are those of the survey itself, in which participation was not complete (response rate, 60%), although the sample size led us to envisage this problem, with the result that the sample was overestimated. Second, we recognize that there may well have been some ambiguity in destination between the options discharge and discharge with follow-up by primary care, especially in telemedicine, where, in the public system, the patient normally visits primary care to receive results, even if follow-up is not necessary; this may diminish the reliability of the results. Third, the low number of patients seen via teledermatology indicates that the corresponding results were not very accurate. Furthermore, the uneven distribution of the activity of teledermatology may lead to bias. Lastly, given that the study of the characteristics of teledermatology was not an initial objective of the survey, we were unable to study many potentially interesting variables that are specific to this discipline.
In conclusion, our results suggest that dermatology clinics in Spain have a considerable ability to resolve cases. Some of the differences observed between private and public centers are due to structural differences in the health system: the origin is more frequently direct in private centers, because in public centers, patients can only be referred to a dermatologist from another specialist or a primary care physician. The high percentage for direct origin in private centers points to a high demand for dermatology services in Spain. We can assume that a large number of these patients are being seen in primary care. It could be interesting to perform studies to compare the cost-effectiveness of management of patients in primary care with that of direct access to a dermatologist.
Teledermatology accounts for a small percentage of all dermatology consultations. It is most widely used in Galicia. Finally, access to teledermatology in Spain is direct in a significant number of cases, probably as a result of the use of smartphone apps. In summary, as far as we know, the data we present are the first to bring together the referral routes and the frequency and characteristics of teledermatology in Spain. We believe that performing similar studies in the future could be of interest, since they would show how these variables progress over time. Given the increasing use and interest in teledermatology, future studies could include other variables associated with teledermatology, such as the method used (real-time or prerecorded), the person who takes the photos, and the use of Smartphone apps.
FundingThe DIADERM study is sponsored by Fundación Piel Sana de la AEDV (Healthy Skin Foundation of the Spanish Academy of Dermatology and Venereology), which received funding from Novartis. The pharmaceutical company did not participate in data collection, data analysis, or interpretation of the results. Guillermo González-López received the Juan de Azúa grant from Fundación Piel Sana, part of which was used to fund the present study.
Conflicts of InterestThe authors declare that they have no conflicts of interest related to this article.
The DIADERM project was made possible thanks to cooperation between the regional coordinators and the participants.
Regional Section Coordinators:
Agustín Buendía, Pablo Fernández-Crehuet, Husein Husein-ElAhmed, Jesús Vega, Agustín Viera, José Manuel Carrascosa, Marta Ferrán, Enrique Gómez, Lucia Ascanio, Ignacio García Doval, Salvador Arias, and Yolanda Gilaberte
Participants:
Juan A. Sánchez, Amalia Serrano, Rosa Castillo, Ramón Fernandez, José Armario, Carolina Lluc Cantalejo, Cristina Albarrán, María Cruz Martín, Juan Antonio Martín, Román Barabash, Lara Pérez, Manuel Salamanca, Carlos Hernández, José Francisco Millán, Inmaculada Ruiz, Susana Armesto, Marta González, Valia Beteta, Concepción Cuadrado de Valles, Pilar Cristóbal, María Magdalena Roth, Juan Garcias, Ricardo Fernandez de Misa, Estela García, María del Pino Rivero, José Suárez, Birgit Farthmann, Alba Álvarez, Irene García, Caridad Elena Morales, María Cristina Zemba, Trinidad Repiso, Carmen Sastre, María Ubals, Alejandro Fernández, Urbà González, Ramón Grimalt, Sara Gómez, Ingrid López, Franco Antonio Gemigniani, María José Izquierdo, Fernando Alfageme, Nuria Barrientos, Laura María Pericet, Santiago Vidal, Celia Camarero, Pablo Lázaro, Cristina García, María Pilar de Pablo, Pedro Herranz, Natalia del Olmo, María Castellanos, Natalia Jiménez, Sonsoles Aboín, Isabel Aldanondo, Adriana Juanes, Dulce María Arranz, Olga González, Luis Casas, Juan José Vázquez, Carmen Peña, José Luis Cubero, Carlos Feal, María Eugenia Mayo, Nicolás Iglesias, Rafael Rojo, Elfidia Aniz, Sabrina Kindem, Nerea Barrado, Marisa Tirado, Ester Quecedo, Isabel Hernández, Antonio Sahuquillo, Rebeca Bella, Ramón García, Anaid Calle, Francesc Messeguer, Alberto Alfaro, Luisa Casanova, Libe Aspe, María Pilar Moreno, Izaskun Trébol, Gonzalo Serrano, Víctor Manuel Alcalde, Patricia García, Carmen Coscojuela.
Please cite this article as: González-López G, Descalzo-Gallego MÁ, Arias-Santiago S, Molina-Leyva A, Gilaberte Y, Fernández-Crehuet P, et al. Referral of Patients to Dermatology and Teledermatology Consultations in Spain. DIADERM Study. Actas Dermosifiliogr. 2019;110:146–152.