Excision of cutaneous scalp tumors results in surgical defects that are difficult to repair because of poor distensibility in this area of the body. The main aim of this study was to develop a structured algorithm to help choose the best technique for reconstructing scalp defects.
Material and methodsRetrospective study of patients who required surgical reconstruction following excision of a cutaneous scalp tumor. We excluded patients with defects that could be closed by simple direct suture and defects for which it was initially decided to use a skin graft or healing by secondary intention. The defects were classified into 5 groups according to the minimum distance between edges. The different reconstruction techniques used were evaluated in each group. The outcomes analyzed were complete defect closure, intraoperative and postoperative complications, and final aesthetic result.
ResultsWe included 119 patients (102 men and 17 women) with a mean age of 71 years (range, 32–93 years). Mean follow-up was 42 months (range, 6–120 months). Sixty-eight patients had a moderate-sized defect with a distance between edges of 1 to 4cm. Reconstructions started with relaxation incisions in 43 defects and resulted in the successful closure of 22 of them. Defects with a distance of 1 to 2cm required a single relaxation incision. Two incisions were required for defects with a distance of 2 to 3cm, while 3 incisions were required for those with a distance of 3 to 4cm. In the 21 cases in which relaxation incisions were insufficient to close the defect, the incisions were extended to mobilize the flap to achieve closure. Relaxation incisions alone were insufficient for closing defects with a distance greater than 4cm.
ConclusionsThe 1-2-3 rule can help in choosing the best reconstruction technique for moderate-sized defects based on the principle that 1, 2, or 3 initial relaxation incisions are needed depending on the minimum distance between edges (1-2cm, 2-3cm, or 3-4cm). In all cases, incision extension to mobilize the corresponding flaps remains an option.
La extirpación quirúrgica de tumores cutáneos de cuero cabelludo crea defectos difíciles de reparar por la poca distensibilidad de la zona. El objetivo principal de este trabajo es conseguir un algoritmo estructurado que permita la elección de la mejor técnica reconstructiva para el cierre de los defectos quirúrgicos de cuero cabelludo.
Materiales y métodosEstudio retrospectivo de 119 pacientes que requirieron la extirpación quirúrgica de tumores de cuero cabelludo con posterior reconstrucción quirúrgica para el cierre del defecto. Se excluyeron los pacientes con defectos que pudieron ser cerrados mediante sutura directa simple, así como en los que desde el principio se decidió emplear injertos cutáneos o se dejaron cerrar por segunda intención. Los defectos se clasificaron en 5 grupos según la distancia mínima de aproximación de los bordes y se evaluaron en cada grupo las diferentes opciones de reconstrucción quirúrgica. Se tuvieron en cuenta como objetivos finales el cierre completo del defecto, las complicaciones intra- y postoperatorias, así como el resultado estético final.
ResultadosSe incluyeron 119 pacientes (102 varones y 17 mujeres); edad media 71 años (rango, 32-93 años). El seguimiento medio fue de 42 meses (rango, 6-120 meses). De los 119 pacientes, 68 tenían defectos de mediano tamaño con una distancia de aproximación entre 1 y 4cm. En 43 de ellos se inició la reconstrucción mediante incisiones de descarga que permitieron el cierre del defecto en 22 casos. Los defectos con distancias de 1 a 2cm necesitaron una sola incisión de descarga. Los comprendidos entre 2 y 3cm, 2 incisiones y de 3 a 4cm, 3 incisiones. En los 21 casos que no cerraron a través de las incisiones de descarga, se ampliaron estas incisiones a sus correspondientes colgajos para conseguir el cierre. Ninguno de los defectos mayores de 4cm cerró solo con las incisiones de descarga.
ConclusionesLa regla«1-2-3» permite elegir la mejor técnica reconstructiva para defectos de mediano tamaño realizando inicialmente 1, 2 o 3 incisiones de descarga según sea la distancia de aproximación de los bordes del defecto entre 1-2cm, entre 2-3cm o entre 3-4cm respectivamente, con la opción de ampliar a los colgajos correspondientes si fuera necesario.
High sun exposure on the scalp, especially in men who are bald, often leads to skin tumors, which are preferably treated by surgical excision. Because the scalp is highly vascularized, flaps that would not be feasible at other sites can be constructed here. Skin pallor after scalp reconstruction does not augur failure or predict necrosis as it does at other locations. Moreover, the subgaleal plane is ideal for flap elevation, and periosteal resection makes it difficult to use skin grafts.
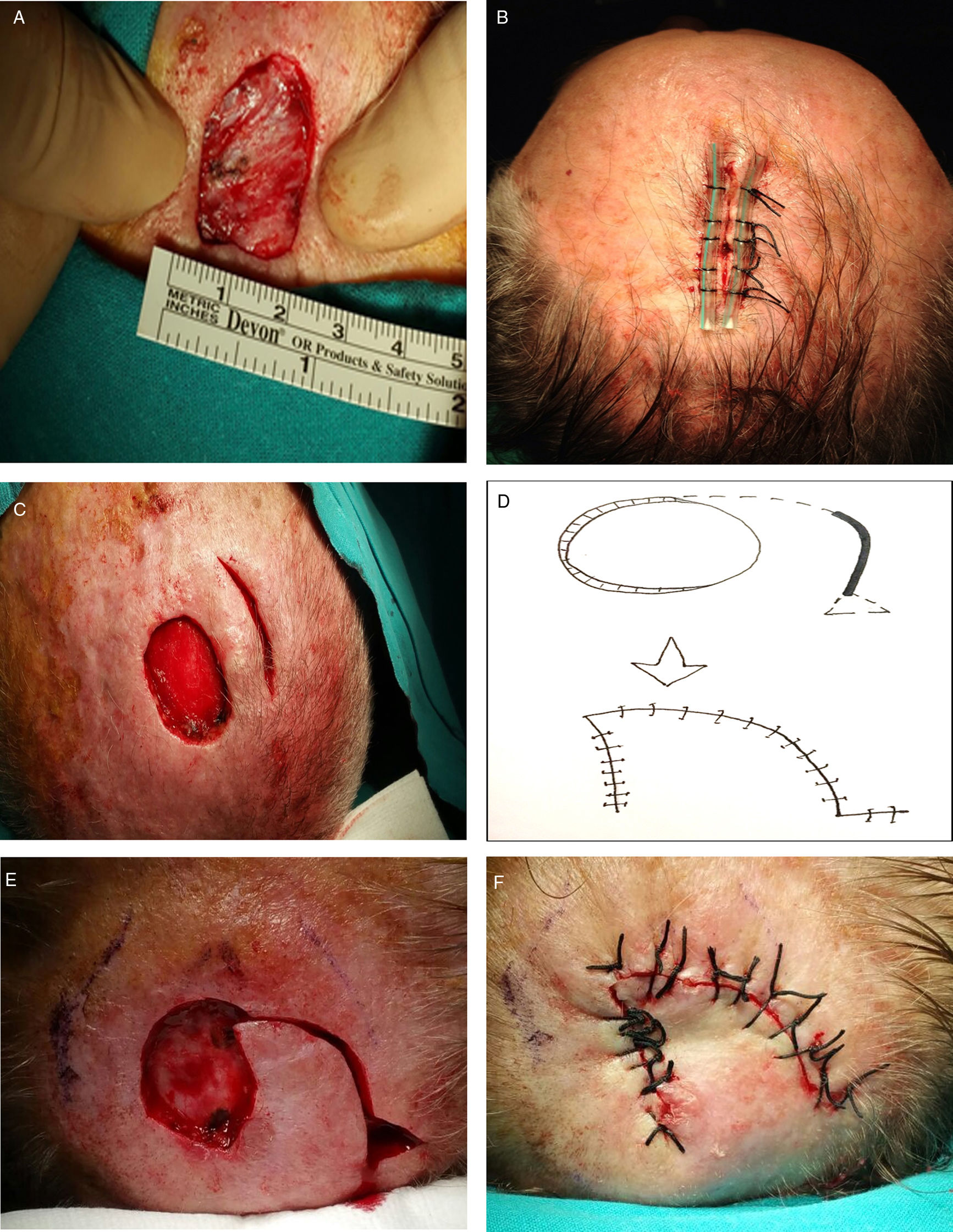
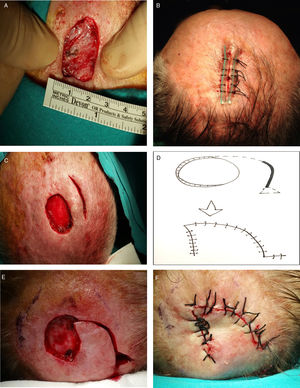
The reconstruction of surgical defects on the scalp is nevertheless challenging for several reasons: anatomical convexity limits tissue displacement, resistance to advancement is different at different points on the scalp, and there is also interindividual variation. Therefore, the natural diameter of the defect is not the best criterion to consider when choosing a reconstruction technique. As a consequence, a surgeon beginning the process of reconstruction first manually pulls the sides of the scalp defect closer together to determine the minimum distance that can be achieved between them (Fig. 1A). The utility of this maneuver, which gives an overall idea of both the defect's diameter and the skin tension in the region, is analyzed in this paper.
Reconstruction of defects with a minimum side-to-side distance less than 2cm after the skin was drawn together manually. A, Measuring the minimum achievable distance between sides. B, A probe-reinforced suture is recommended for distances less than 1cm. C, Defects measuring between 1and 2cm may require a release incision. D–F, If closure is still not possible, a rotation flap can be used.
Records were analyzed for 119 patients who underwent surgical excision of scalp tumors between 2007 and 2017. Although a total of 725 scalp tumors had been excised, cases were excluded if the first choice for defect closure was a simple suture, granulation (secondary-intention healing), or a skin graft.
The cases were classified in 5 groups according to the minimum manually achievable distance between the sides of the defect: less than 1cm, between 1and 2cm, from 2to 3cm, from 3to 4cm, and more than 4cm.
Outcomes evaluated were the rate of use of the simplest feasible technique for closing the defect in each minimum-distance group, the results observed during follow-up, early and late complications, and final cosmetic results.
Most defects with minimum achievable side-to-side distances of less than 1cm were closed with a single suture of mattress stitches reinforced by a sterile aspiration probe placed on either side of the vertical line (Fig. 1B). The probes absorbed all the tension in the closure, facilitated traction, and protected the borders from tearing. Very good results were obtained with the reinforced suture, which is simple and accomplished quickly, resolving nearly all small defects of less than 1cm.
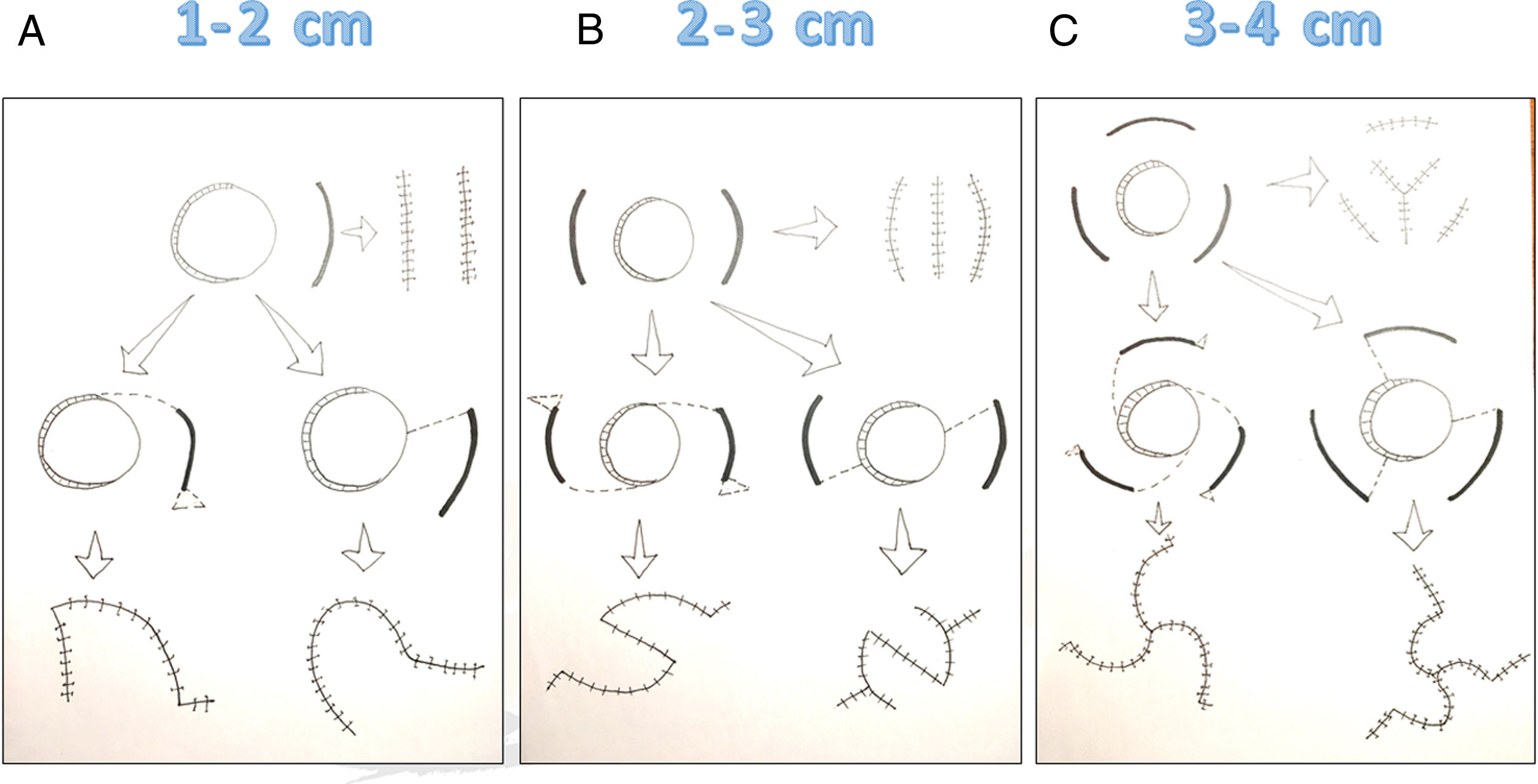
When the minimum achievable distance between the sides of the defect was between 1and 2cm, a release incision was made at a distance from the defect that was similar to its diameter (Fig. 1C). In many cases this incision provided enough tissue mobility to close both defects using 2 independent sutures. If closure was not possible with this approach, however, the release incision was extended along a curve towards the defect to create a classic rotation flap (Figs. 1D–1F). Another possibility was to make a perpendicular back-incision from the defect to create a Limberg transposition flap. Finally, if necessary, a second such flap could be created on the other side of the defect (a double Limberg) or an O-to-Z rotation flap could be designed. Such techniques were not usually required in this group, however.
When the minimum achievable side-to-side distance was between 2and 3cm, reconstruction started with 2release incisions on either side of the defect. None of the defects in this category could be closed with a single release incision; 2 such incisions were therefore always made and in many cases achieved sufficient advancement to allow the defect to be closed with 3 independent lines of suture (Figs. 2A and 2B). If the defect could not be closed with this approach, however, the release incisions were extended along a curve in the direction of the defect (Fig. 2C) to create a double rotation flap (Figs. 2D and 2E). Other defects in this size group were closed by extending the release incisions with a perpendicular back-incision to create double Limberg flaps.
Reconstruction of defects with a minimum side-to-side distance of 2to 3cm after the skin was drawn together manually.
A, Begin the process of closing these defects by making 2release incisions. B, After elevating the tissue, close with sutures. C–D, If that approach fails, design a double O-to-Z rotation flap. E, Close.
When the minimum distance between the sides fell between 3and 4cm, 3release incisions were made around the defect (Fig. 3A). None of the defects in this group could be closed with either a single or 2 release incisions. Since it is not possible to switch from 2 to 3 release incisions, 3 of them were appropriately distributed around the defect from the start in all the cases in this group. These incisions facilitated closure of the defect using the recently described Mercedes flap1 (Figs. 3B and 3C). If the wound could not be closed with this approach, all 3 incisions were extended along a curve in the direction of one side of the defect. Three flaps were elevated and the defect was closed with a triple rotation flap technique first described in 1971 by Orticochea.2 As in the groups described above, the release incisions could also be extended by a perpendicular back-incision to create a triple Limberg flap (Figs. 3D–3F).
Reconstruction of defects with a minimum side-to-side distance of 3to 4cm after the skin was drawn together manually. A, Begin the process of closing these defects by making 3release incisions. B, Draw the skin together and secure with a single suture. C, Close the release incisions with a Mercedes flap. D–E, If a Mercedes flap cannot close the defect, prepare a triple Limberg flap. F, Close.
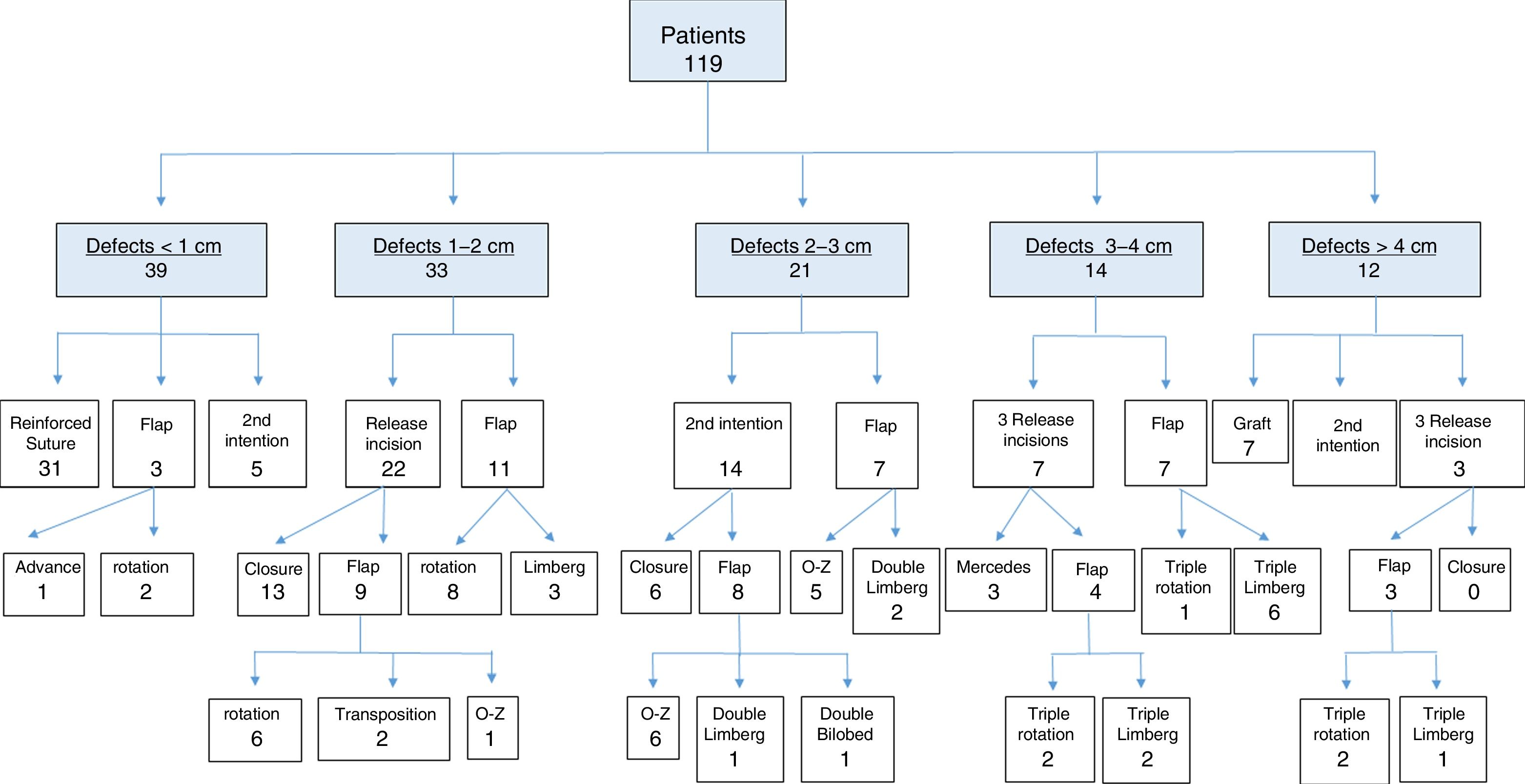
The distribution of defect sizes and closure techniques is shown in Fig. 4. The 119 patients studied (102 men, 17 women) ranged in age from 32 to 93 years. The average age was 71 years. Most of the excised tumors were spindle cell squamous carcinomas (89). There were also basal cell carcinomas (20), melanomas (7) merkelomas (2), and a single angiosarcoma. The patients were followed for an average of 42 months (range, 6–120 months).
Thirty-nine of the 119 patients had small surgical defects (minimum achievable side-to-side distance of less than 1cm). Thirty-one of these cases were closed with a suture reinforced with a sterile aspiration probe on either side of the wound. Five others that were only partly closed with this type of suture were allowed to complete the process by second-intention healing. Flaps were used in 3other cases (1advancement flap and 2rotation flaps). Results were excellent in most of the 31 cases closed directly with a reinforced suture, but superinfection of the wound complicated 2cases. Somewhat wider, less cosmetically pleasing scars resulted in the 5cases that were allowed to heal by second intention. Surgery lasted longer in the 3flap reconstructions, and one of these incisions reopened 3days later.
The group of defects with minimum achievable side-to-side distances of 1to 2cm comprised 33cases. A single release incision started the process in 22of these cases and closure was completed without a flap in 13of them. The release incision was extended to allow closure with a rotation flap in the 9remaining cases in this group, and that technique provided successful reconstruction in 6 of them. In 2 cases the incision was extended to create a Limberg transposition flap, and in the last of the 9cases a second contralateral rotation flap was required to close the defect with a double O-to-Z rotation flap. No initial release incision was made in 11cases in this 33-patient group. Instead, a rotation flap was immediately chosen for 8 of the 11, and a Limberg transposition flap was used for the other 3. Good cosmetic results were seen in short- and long-term follow-up visits with these patients, except for slight dehiscence in a reconstruction started with a single release incision and in another reconstructed directly with a Limberg flap.
There were 21patients in the group with defects with minimum side-to-side distances of 2to 3cm. Two release incisions were made in 14 of them and were sufficient for closure in 6. In a few cases a single release incision was initially tried but was never sufficient for closure; therefore, a second was made. In another 6in the group of 14patients for whom the 2release incisions were insufficient, the incisions were extended to create 2O-to-Z rotation flaps. The 2remaining patients in the group required extension of the incisions to create 2transposition flaps (1Limberg-type flap and 1bilobed flap). In the 7remaining cases in this group of 21, a double rotation flap (5cases) or a transposition flap (2cases) was designed directly. No differences were observed in outcomes during follow-up, regardless of whether or not release incisions were made (ie, whether flaps were initially designed or the result of extending the release incisions). The sutures reopened in only 2 cases repaired by starting with release incisions. A single case of superinfection occurred in a defect closed with a double Limberg flap created by extending the release incisions.
Fourteen patients had defects that measured 3to 4cm from side to side. None of the 14 could be closed with either 1 or 2 release incisions. In 7 of the 14 cases, 3 release incisions were made directly, and they allowed for primary closure of the defect with a Mercedes flap in 3 of them. In the other 4 cases, the release incisions were extended back to the defect to create triple rotation flaps in 2and Limberg transposition rotation flaps in 2. The remaining 7defects were repaired directly with triple Limberg flaps (6cases) or a triple rotation flap (1case). No differences in outcomes were observed on follow-up, although 1Mercedes flap and 2of the direct Limberg flaps opened up.
Twelve patients had surgical defects measuring more than 4cm even after the sides were pulled together. Reconstruction started with 3 release incisions in 3 of the 12, but as primary closure could not be achieved, triple flaps were designed. Seven cases required skin grafts. Two were left for second-intention healing. Closure with a triple rotation flap was attempted in 2cases. One of them closed partially and a graft was then provided to complete the closure. The twelfth case was reconstructed with a directly designed triple Limberg flap. Follow-up records showed that second-intention healing took more than 6weeks. The outcomes in the cases requiring grafts were good, although partial necrosis developed in 1of the 7cases, and the cosmetic outcome was not ideal in some. Dehiscence occurred in 2of the 3flap reconstructions.
Overall, 13 of the 119 patients (10.92%) experienced some type of complication or poor cosmetic outcome, results that were more frequent in patients with large surgical defects. However, frequency bore no relation to the type of reconstruction technique chosen.
DiscussionGuidelines and review articles advise on the best reconstruction approach to use in difficult areas on the face,3,4 but the closure of surgical defects on the scalp is particularly problematic because of skin tension and poor elasticity. Most clinical guidelines and decision trees use the area of the defect as the basis for choosing the most appropriate technique.5–9 However, this criterion does not take into consideration interindividual variation in skin elasticity or other patient factors such as the zone under the scalp that is affected or the effects of prior treatments (for example, fibrosis after radiotherapy or scaring from previous sutures). To remedy this problem, this study proposes a new concept, the minimum side-to-side distance when the skin around the defect is drawn together manually. This minimum manually achievable distance between sides reflects a combination of the diameter of the defect and the elasticity of the tissues around it and thus offers an objective criterion for guiding choice of reconstructive technique. To use this approach, the surgeon beginning reconstruction of the defect created by excising a scalp lesion, must first draw the sides of the defect as close together as possible and measure the minimum distance. This maneuver, which surgeons often do unconsciously, should be expressly attended to and measured precisely if it is to provide information on which to base the choice of reconstructive technique.
Another innovative aspect of this approach is the initial employment of release incisions as the first reconstructive step. These extra incisions increase the area that can be advanced. The tissue freed in this way is sufficient to close most defects.
Yet another contribution this approach makes is to facilitate flap design by extending the release incisions in the event that they are insufficient for defect closure. Because these incisions can be transformed, a strategic sequence emerges that starts by trying the simplest effective technique and then adapting it according to individual circumstances.
This retrospective case series shows that large defects, of a minimum distance of more than 4cm, can be closed by either second-intention healing or total skin grafts. Release incisions did not achieve closure of any of these defects, and flap closure —whether initially planned or created by extending release incisions —was associated with a higher rate of complications. Other options for closing large defects include galeal incisions to facilitate skin displacement, flaps in combination with Burow grafts, tissue expansion,10 latissimus dorsi pediculated flaps,11 free flaps,12 or dermal regeneration systems.13
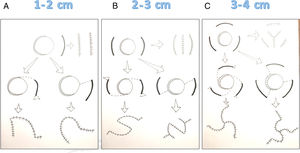
The reconstruction decision tree described here, using the minimum manually achievable distance between the sides of a defect as the starting point, is termed the 1–2–3 rule for its mnemonic value. To reconstruct defects with a minimum distance between 1and 2cm, start with 1release incision; for defects between 2and 3cm, start with 2incisions; and for those between 3and 4cm, start with 3incisions. If closure cannot be accomplished with the recommended number of release incisions, they can be extended to design rotation or transposition flaps (Fig. 5).
The 1–2–3 rule for reconstructing scalp defects.
Reconstruction of defects with a minimum side-to-side distance of 1 to 2cm starts with a single release incision that can be extended to create a rotation or transposition flap if necessary. Reconstruction of defects with a minimum side-to-side distance of 2 to 3cm starts with 2 release incisions, which can be extended to create double rotation or transposition flaps. Reconstruction of defects with a minimum side-to-side distance of 3 to 4cm starts with 3 release incisions, which can be extended to provide triple rotation or transposition flaps if necessary.
Sixty-eight cases in this series involved mid-sized defects with minimum manually achievable distances between 1and 4cm. Closure was achieved by means of the release incisions in 22 of the 43 cases (51%) in which the reconstruction process started with them. Thus, over half the patients’ defects could be fully closed by using the simplest process, which takes advantage of the mobility afforded by such incisions without resort to flaps.
The proposed stepped and adaptable 1–2–3 rule follows a logical sequence that starts by attempting closure with a direct suture. If closure is not possible, the surgeon passes on to the next simplest option —a reinforced suture. The next step in the sequence is a release incision, followed if necessary by extending the incision to design a rotation or transposition flap. A fourth option is the design of a contralateral rotation or transposition flap to facilitate movement of a large area of surrounding tissue to close the defect. This stepped approach therefore offers many alternatives incrementally while still ensuring that the simplest possible technique appropriate for each defect will be the one that is used. In contrast, if a complex flap is designed and begun from the start of reconstruction, closure may still be impeded but without the possibility of incrementally adding alternatives.
Naturally, this 1–2–3 rule must be adapted to individual cases, according to the patient's general condition and the surgeon's preferences. For certain individuals and defects with minimum side-to-side distances between 1and 4cm, skin grafts covering the whole defect or second-intention healing may be good options. However, grafts usually give inferior cosmetic results and are associated with greater risk of necrosis. Second-intention healing, on the other hand, although simple and faster to prepare, requires a much longer period of waiting for scar tissue to form, placing a greater burden on the patient while still giving only modest cosmetic results at the end.
The complication rates in this case series were similar to those reported in another series.14 Complications were more common in patients with large defects, but no influence of reconstructive technique could be identified. Flaps made by extending the release incisions yielded cosmetic and functional results that were similar to the flaps designed from the start of the process. This observation supports the approach of beginning with release incisions to attempt to close the defect by that means alone and later extending incisions to create flaps only if necessary.
LimitationsThis study is affected by the limitations intrinsic to any retrospective design. The protocol described, starting with release incisions, was not applied to all the scalp defects resolved during the period of the study. Of the 68 patients with defects measuring 1to 4cm, reconstruction started with release incisions in 43. Reconstruction flaps were planned initially for the other patients before the protocol described by the 1–2–3 rule was introduced. In addition, the number of patients with large defects (minimum manually achievable distances of 4cm from side to side) was small in comparison with the numbers in other groups. Therefore, it is impossible to draw conclusions about other more complex reconstruction techniques for defects that are large or involve the bone. Initiating reconstruction with release incisions is therefore appropriate only for defect sizes with minimum manually achievable distances of 1 to 4cm between sides.
ConclusionsThis stepped approach to choosing the simplest effective technique for closing scalp defects relies on first observing the minimum manually achievable distance between the sides of a defect. The 1–2–3 rule indicates the number of release incisions that mark the starting point in the reconstruction process, according to the minimum distance measured. The incisions can be extended to design flaps if necessary.
Conflicts of InterestThe author declares that he has no conflicts of interest.
Please cite this article as: Russo F. Regla «1-2-3» para la reconstrucción de defectos de mediano tamaño del cuero cabelludo. Actas Dermosifiliogr. 2019;110:474–481.