Short-duration ambulatory surgery for the removal of skin tumors under local anesthesia is increasingly common in dermatology. Preoperative assessment has traditionally targeted the identification of any unknown diseases or other health conditions that might lead to changes in plans for anesthesia or surgery. Hospitals and specialists differ greatly in the tests they order in patients about to undergo outpatient dermatologic surgery given that hardly any finding would be likely to contraindicate or lead to changes in the procedure. This study aimed to provide guidance for those ordering tests before outpatient dermatologic surgery.
MethodsIn 2017 our hospital developed a protocol to standardize preoperative testing for outpatient dermatologic surgery. We designed an observational, descriptive, retrospective analysis of tests ordered for patients scheduled for such surgery before and after the protocol was applied.
ResultsFewer tests were ordered after the protocol was introduced. We detected no statistically significant differences in relation to type of surgery planned or postoperative complications.
ConclusionsPatients about to undergo outpatient dermatologic surgery under local anesthesia who have no unusual health risks may not require preoperative testing.
La cirugía dermatológica ambulatoria es una práctica clínica cada vez más habitual, basada en la extirpación de tumores cutáneos mediante anestesia local y con un tiempo quirúrgico reducido. Tradicionalmente, la valoración preoperatoria se ha realizado con el fin de detectar alguna alteración o proceso patológico desconocido que pudiera modificar el plan anestésico y/o quirúrgico. Existe una gran variabilidad entre centros y especialistas sobre las pruebas a solicitar en aquellos pacientes que van a ser sometidos a una intervención quirúrgica dermatológica ambulatoria, teniendo en cuenta que, por el perfil de esta cirugía, prácticamente ningún hallazgo podría modificar o contraindicar la intervención. El objetivo es ofrecer una referencia de actuación para la petición de pruebas preoperatorias en cirugía dermatológica ambulatoria.
MétodosEn 2017 se desarrolló en nuestro centro un protocolo para intentar unificar la petición de pruebas preoperatorias en cirugía dermatológica ambulatoria. Se realizó un estudio observacional, descriptivo y retrospectivo analizando las pruebas solicitadas a pacientes sometidos a este tipo de cirugía, comparando antes y después de la aplicación del protocolo.
ResultadosTras la instauración del protocolo se solicitó menor número de pruebas complementarias, sin diferencias estadísticamente significativas en el tipo de cirugía ni complicaciones postoperatorias.
ConclusionesLos pacientes que vayan a ser sometidos, bajo anestesia local, a cirugía dermatológica ambulatoria, y que se encuentren en su estado de salud habitual, podrían no tener indicación de realización de pruebas complementarias preoperatorias.
Ambulatory dermatologic surgery is increasingly common due to growing demand as a result of increased life expectancy and greater access to the health care system. Most dermatologic surgery consists of outpatient procedures to remove skin tumors, as their incidence is increasing and it is estimated that 1 of every 5 people will develop skin cancer during their lifetime.1,2
Due to the profile of patients who develop skin tumors, candidates for dermatologic surgery tend to have major comorbidities. Preoperative assessment is an essential component in the management of surgical patients and its ultimate goal is to optimize the status of the patient prior to surgery.3
Many studies3–7 have examined the utility of additional preoperative tests in ambulatory surgery and have questioned their use owing to lack of relevant in terms of preoperative management and of their effect on the surgical results. Traditionally, these preoperative tests have been ordered and carried out routinely, and are not based on clinical evidence.
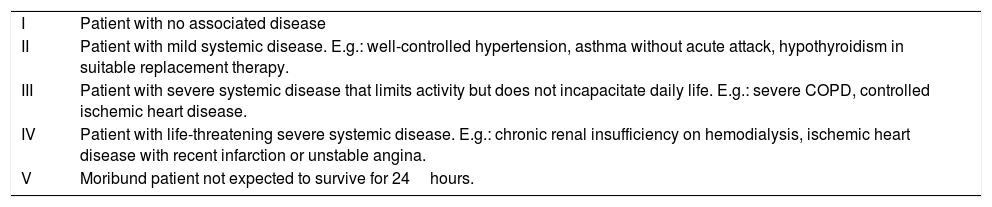
The most widely used scale for evaluating the risk of surgical patients is that proposed by the American Society of Anesthesiologists (ASA), which classifies patients according to their morbidity (Table 1). In this regard, different scientific societies have proposed ordering preoperative tests in accordance with the patient's risk and the proposed surgery. Despite these considerations, however, preoperative tests ordered in ambulatory dermatologic surgery vary considerably depending on the hospital and the surgeon,8 and there are no studies, protocols or guidelines that define the tests that should be ordered. As part of the project to improve the quality of care at Hospital Universitario Gregorio Marañón, Madrid, Spain, in 2016, the development of a protocol for adapting preoperative tests to patients undergoing ambulatory dermatologic procedures in order to reduce existing variability was proposed as a quality objective.
ASA Score.
| I | Patient with no associated disease |
| II | Patient with mild systemic disease. E.g.: well-controlled hypertension, asthma without acute attack, hypothyroidism in suitable replacement therapy. |
| III | Patient with severe systemic disease that limits activity but does not incapacitate daily life. E.g.: severe COPD, controlled ischemic heart disease. |
| IV | Patient with life-threatening severe systemic disease. E.g.: chronic renal insufficiency on hemodialysis, ischemic heart disease with recent infarction or unstable angina. |
| V | Moribund patient not expected to survive for 24hours. |
The objective of our study was to assess the number of preoperative tests requested following the application of that protocol and to determine the incidence of surgical complications in both periods.
MethodsWe performed a descriptive retrospective study that compared the preoperative tests ordered by the dermatology department of Hospital General Universitario Gegorio Marañón during 2 equivalent time periods: before application of the protocol (January 1 to March 31, 2016) and after its application (January 1 to March 31, 2017). The study included all patients operated on at our department during both periods. Data were obtained from the electronic patient records and informed consent was provided.
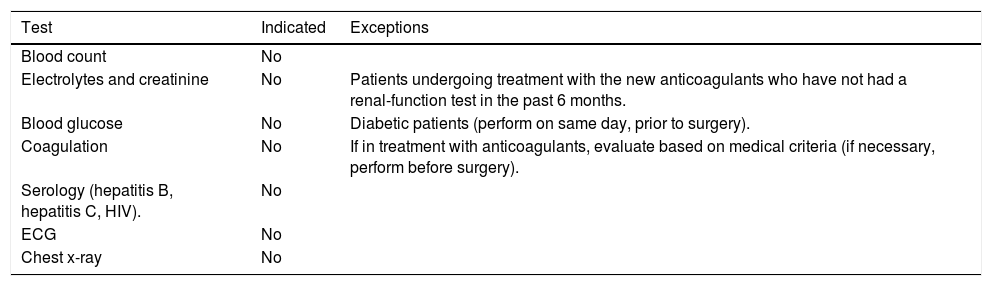
A protocol of recommendations for requesting preoperative tests in ambulatory dermatologic surgery was developed at our hospital by members of the anesthesiology and resuscitation department and the dermatology department, following the recommendations of the Spanish Society of Anaesthesiology, Resuscitation and Pain Therapy and of the Spanish Association of Major Ambulatory Surgery.9 The protocol determined that patients who required this type of surgery and who remained in their usual state of health did not require any tests. It also established some exceptions, which are shown in Table 2. This protocol was distributed to members of the dermatology and anesthesiology departments and was applied from January 2017.
Summary of Recommendations for Preoperative Tests in Patients Undergoing Ambulatory Dermatologic Surgery.
| Test | Indicated | Exceptions |
|---|---|---|
| Blood count | No | |
| Electrolytes and creatinine | No | Patients undergoing treatment with the new anticoagulants who have not had a renal-function test in the past 6 months. |
| Blood glucose | No | Diabetic patients (perform on same day, prior to surgery). |
| Coagulation | No | If in treatment with anticoagulants, evaluate based on medical criteria (if necessary, perform before surgery). |
| Serology (hepatitis B, hepatitis C, HIV). | No | |
| ECG | No | |
| Chest x-ray | No |
The epidemiologic characteristics of the enrolled patients, the surgical procedures they underwent, the differences between the 2 periods with respect to the preoperative tests ordered, the results of those tests, and any postoperative complications were analyzed.
Statistical AnalysisVersion 22 of the SPSS statistical software package was used for the statistical analysis. The Kolmogorov-Smirnov test was used to determine whether numeric variables were normally distributed. A descriptive and comparative analysis was performed for the 2 periods studied. Quantitative variables with a normal distribution were compared using the t test for independent samples. The Mann-Whitney U test was used where distribution was not normal. Qualitative variables were compared with the χ2 test or the Fisher exact test, as appropriate. A value of P<.05 was considered to be statistically significant.
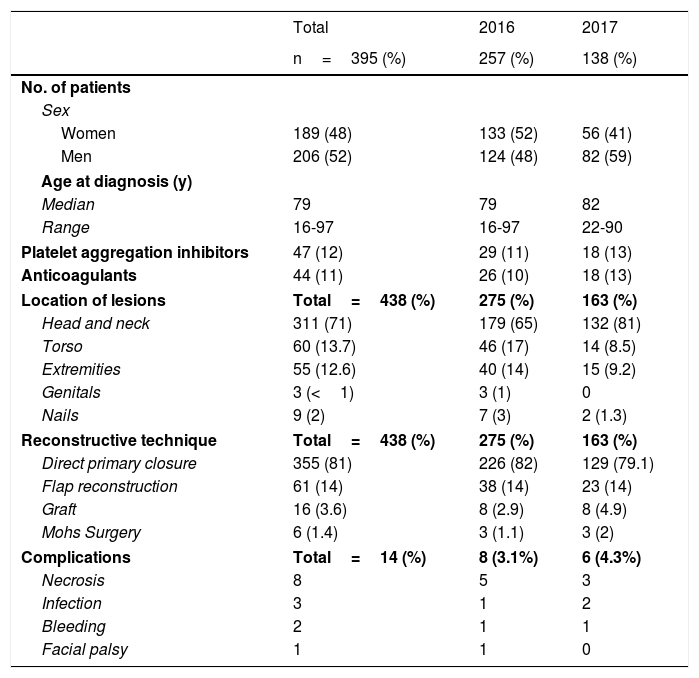
ResultsA total of 395 patients who underwent ambulatory dermatologic surgery at Hospital General Universitario Gregorio Marañón in the first quarter or 2016 and 2017 (257 in 2016 and 138 in 2017) were enrolled in the study. The number of patients undergoing surgery was lower in the second period than in the first period, owing to lesser availability of operating theaters in that quarter. Nevertheless, a comparative study found no differences between the 2 groups for the variables analyzed.
A total of 438 lesions were removed, with a mean of 1.10 lesions per patient per operation. Table 3 shows the epidemiologic characteristics, location of the lesions, reconstructive technique, and surgical complications in the patients enrolled in the study.
Epidemiological Data of Patients Undergoing Ambulatory Dermatologic Surgery Included in the Study.
| Total | 2016 | 2017 | |
|---|---|---|---|
| n=395 (%) | 257 (%) | 138 (%) | |
| No. of patients | |||
| Sex | |||
| Women | 189 (48) | 133 (52) | 56 (41) |
| Men | 206 (52) | 124 (48) | 82 (59) |
| Age at diagnosis (y) | |||
| Median | 79 | 79 | 82 |
| Range | 16-97 | 16-97 | 22-90 |
| Platelet aggregation inhibitors | 47 (12) | 29 (11) | 18 (13) |
| Anticoagulants | 44 (11) | 26 (10) | 18 (13) |
| Location of lesions | Total=438 (%) | 275 (%) | 163 (%) |
| Head and neck | 311 (71) | 179 (65) | 132 (81) |
| Torso | 60 (13.7) | 46 (17) | 14 (8.5) |
| Extremities | 55 (12.6) | 40 (14) | 15 (9.2) |
| Genitals | 3 (<1) | 3 (1) | 0 |
| Nails | 9 (2) | 7 (3) | 2 (1.3) |
| Reconstructive technique | Total=438 (%) | 275 (%) | 163 (%) |
| Direct primary closure | 355 (81) | 226 (82) | 129 (79.1) |
| Flap reconstruction | 61 (14) | 38 (14) | 23 (14) |
| Graft | 16 (3.6) | 8 (2.9) | 8 (4.9) |
| Mohs Surgery | 6 (1.4) | 3 (1.1) | 3 (2) |
| Complications | Total=14 (%) | 8 (3.1%) | 6 (4.3%) |
| Necrosis | 8 | 5 | 3 |
| Infection | 3 | 1 | 2 |
| Bleeding | 2 | 1 | 1 |
| Facial palsy | 1 | 1 | 0 |
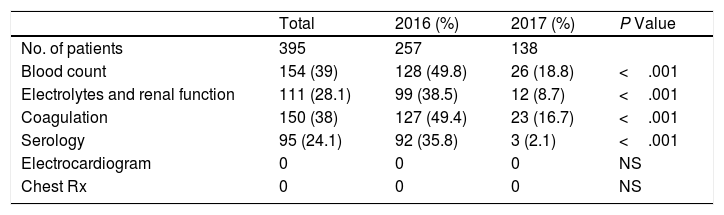
The number of tests requested was lower in the 2017 period than in the 2016 period. Blood counts and coagulation tests were requested in nearly half of patients in 2016, whereas these tests were requested in less than 20% of patients in 2017. Thirty percent fewer biochemistry and serology tests were ordered in 2017 than in 2016. The preoperative tests carried out in the 2 periods are shown in Table 4.
Preoperative Tests Requested in the Study Overall and Comparing the Periods Prior to and After Application of the Protocol.
| Total | 2016 (%) | 2017 (%) | P Value | |
| No. of patients | 395 | 257 | 138 | |
| Blood count | 154 (39) | 128 (49.8) | 26 (18.8) | <.001 |
| Electrolytes and renal function | 111 (28.1) | 99 (38.5) | 12 (8.7) | <.001 |
| Coagulation | 150 (38) | 127 (49.4) | 23 (16.7) | <.001 |
| Serology | 95 (24.1) | 92 (35.8) | 3 (2.1) | <.001 |
| Electrocardiogram | 0 | 0 | 0 | NS |
| Chest Rx | 0 | 0 | 0 | NS |
NS indicates not significant.
Out of all the tests ordered, abnormal results were found in 6 patients: 2 serology tests were positive for hepatitis B, 1 blood count showed abnormally low hemoglobin (9.6g/dL), 1 blood count revealed mild thrombocytopenia (90,000 platelets), and 1 blood count revealed elevated levels of gamma-glutamyl transferase (102U/L).
Surgical complications were recorded in 14 patients (3.5%) (Table 3). Most of these complications occurred in patients undergoing more complex surgical procedures, such as grafts and mixed-thickness flaps. No differences were found in the number of findings in additional tests or in surgical complications between the 2 periods.
DiscussionApplication of the preoperative protocol in ambulatory dermatologic surgery established at our hospital has made it possible to reduce the total number of tests ordered by 40% (from 244 in 2016 to 151 in 2017) without increasing surgical risk. No increase was found in the incidence of postoperative complications following application of the protocol.
The results of the additional tests rarely affect clinical management of the patient and are of little predictive value for perioperative complications in asymptomatic patients.4 A randomized controlled study published in 20005 showed that performing preoperative tests in patients who underwent surgery for cataracts provided no advantage in terms of preventing surgical complications, as shown by other studies on ophthalmologic surgery.6,7
In the project Compromiso por la Calidad de las Sociedades Cientificas en España (commitment to quality by scientific societies in Spain), in the section on “do not perform” recommendations, the quality standard of the Spanish Society of Anaesthesiology, Resuscitation and Pain Therapy states, “do not perform laboratory tests in patients with no systemic disease (ASA I and II) prior to low-risk surgery with minimal estimated blood loss” and “do not perform preoperative tests in cataract surgery, unless indicated based on the patient's clinical history and the physical examination”.10 Similarly, in relation to other specialties,11,12 procedures such as surgery for inguinal hernia, umbilical hernia, hemorrhoidectomy, and arthroscopic surgery, which have a low associated rate of complications, involve minimal blood loss, are short, and require minimal postoperative care, are candidates for not performing preoperative tests.
These tests are of unquestionable diagnostic value provided that they are indicated. The recommendations contained in the protocol and, by extension, in this study, should be seen as a guide and can never replace professional medical judgement. However, routinely ordering these tests has not been shown to be an efficient practice13 and causes unnecessary discomfort to the patient and increases health care expenditure.4
The current health care system champions the rational and efficient use of resources. Preoperative management includes additional tests that, while not expensive individually, constitute a huge expense if we consider the large number of patients undergoing surgery, especially ASA I and II patients. Given the estimated mean cost of each test,14–16 economic differences between hospitals aside, performing a blood count, biochemistry, coagulation, serology for HIV, hepatitis B, and hepatitis C, chest x-ray, and electrocardiogram for 1 patient involves a cost of approximately 112 euros; this cost is not justified by the risk-benefit relationship and cannot be considered an efficient practice in terms of resource-management. In 2016, 742 patients underwent ambulatory surgery at the dermatology department of our hospital. If the protocol had been applied that year, an estimated savings of 83,000 euros would have been achieved.
The results of our study support the tendency to not perform proposed by different societies and publications, and aim to encourage different medical and surgical specialties to begin to establish evidence-based protocols that optimize ordering of preoperative tests.17
In conclusion, requesting additional preoperative tests may not be indicated in patients undergoing ambulatory dermatologic surgery with local anesthetic who are in their usual state of health.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Nieto-Benito LM, Vilas-Boas P, Zaballos M, Llorente-Parrado C, Avilés-Izquierdo JA. Recomendaciones en la petición de pruebas preoperatorias en cirugía dermatológica ambulatoria. Actas Dermosifiliogr. 2019;110:469–473.