Eccrine squamous syringometaplasia (ESS) is a squamous metaplasia of the cuboidal cells of the of the eccrine sweat ducts. ESS is considered a nonspecific reactive response to exposure to toxic agents and drugs but has also been described following cutaneous processes, such as tumors, infections and inflammatory conditions, such as pyoderma gangrenosum, phytophotodermatitis, and chronic ulcers.1–4
We report a peculiar case of radiodermatitis with the unusual histopathologic finding of ESS.
The patient was a 62-year-old man who reported the appearance of an itchy erythematous plaque on the right side of his back. The plaque had developed 15 days earlier. His medical history included metabolic syndrome, hyperuricemia, and chronic ischemic heart disease. The patient was receiving regular treatment with atorvastatin, allopurinol, enalapril, isosorbide, carvedilol, ticlopidine, sitagliptin, and metformin. In the previous 2 months, he had undergone a diagnostic coronary angiography and 2 angioplasties.
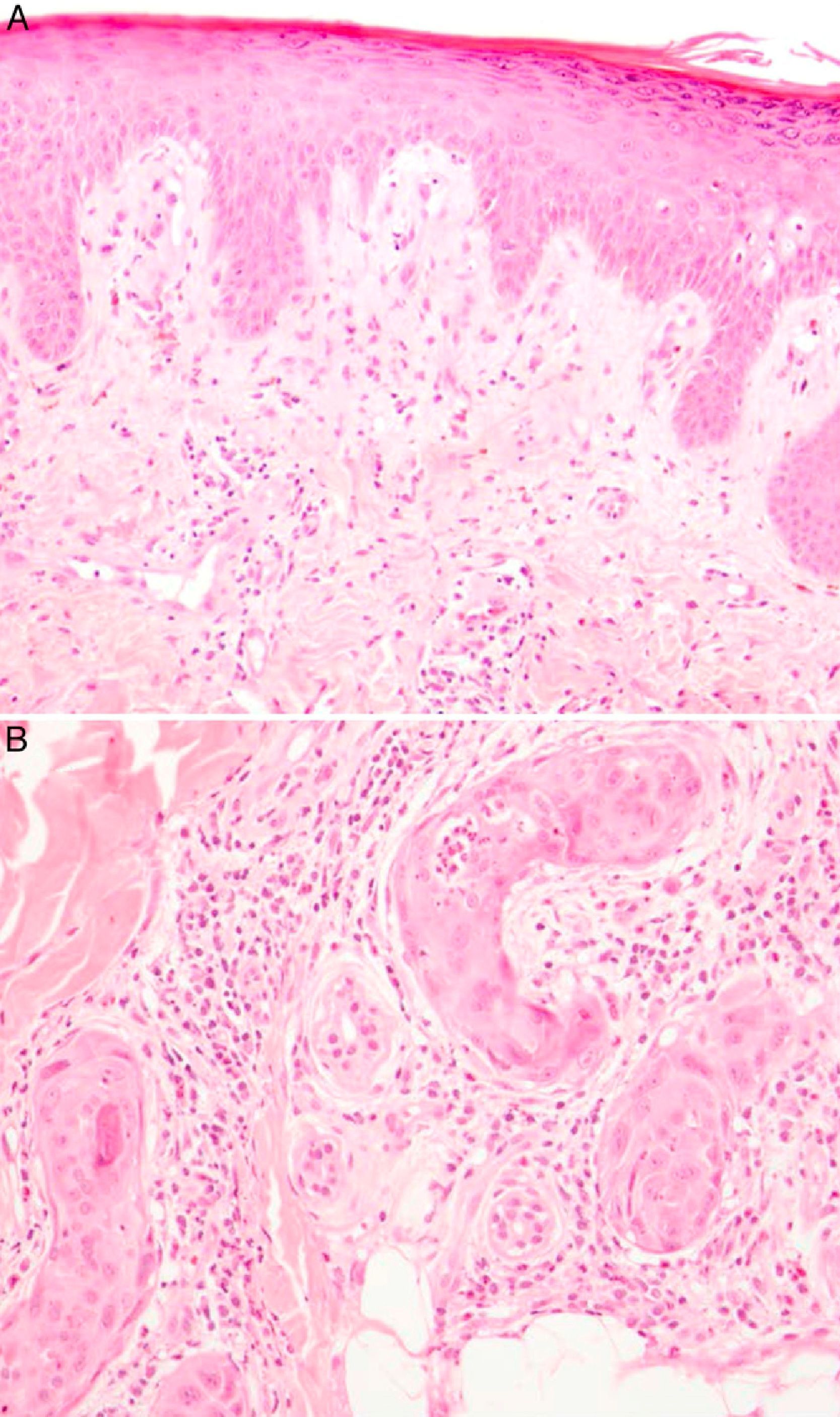
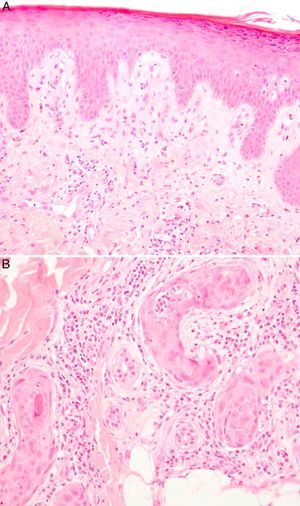
Physical examination revealed a square-shaped erythematous plaque (9×12cm) with well-defined borders and an eroded center (Fig. 1). The location coincided with one of the sites irradiated when the patient received a total dose of 7.8Gy in 3 separate procedures. Histopathology demonstrated hyperkeratosis, irregular acanthosis and dysmaturation of the epidermis, a moderate predominantly neutrophilic perieccrine inflammatory infiltrate in the dermis, and squamous metaplasia of both eccrine coil and duct (Fig. 2). These findings were compatible with ESS.
A, Hyperkeratosis and irregular acanthosis. Signs of epidermal dysmaturation: dyskeratotic cells, with keratinocytes of altered size and polarity, some of which are binucleated (hematoxylin-eosin, original magnification×10). B, Eccrine duct in which areas of squamous metaplasia and a neutrophilic infiltrate can be observed inside the coil, as well as a moderate perieccrine inflammatory infiltrate (hematoxylin-eosin, original magnification×40).
The radiodermatitis plaque responded favorably to local treatments and topical corticosteroids. At the time of writing, only slight residual hyperpigmentation persisted.
The frequency of radiodermatitis caused by coronary procedures is not known but is thought to be increasing due to the growing use and complexity of these interventions. The most commonly affected locations are the right axillary region, the middle third of the back, the right anterolateral region of the chest, and the scapular area, as in the present case.5,6
Depending on the time of onset of skin lesions after exposure, radiodermatitis is classically described as either acute or chronic. In recent years, a subacute category has also been added; this form usually occurs weeks to months after the initial exposure.7
The radiation dose required to cause erythema is estimated at 3Gy, and doses of over 12Gy can cause peeling as well as secondary necrosis and ulceration. However, the dose threshold varies widely depending on the area exposed and an individual's susceptibility.8,9 Thus, the radiation dose of more than 7.8Gy received by our patient in the lesion area was sufficient to initiate a cutaneous inflammatory response which may have induced both the radiodermatitis and the ESS.
We have found no similar cases in the literature describing an association between these two conditions.
This patient had not been exposed to any new substances, except for Visipaque (iodixanol), an iodinated contrast agent used during fluoroscopic procedures. However, no association between this substance and ESS has been described.
The differential diagnosis should include dermatitis due to radiation recall, which can present with ESS.10 However, radiation recall dermatitis most commonly affects areas of radiotherapy-exposed skin that are subsequently reactivated by a second substance, often a chemotherapeutic agent. In our case, given the short clinical course of the condition and the lack of exposure to precipitating agents, we can reasonably rule out this diagnosis.
In summary, we have presented an unusual case of ESS in a patient with radiodermatitis, which we believe should be added to the list of dermatological conditions in which signs of ESS may be observed.
Please cite this article as: Concha Garzón MJ, et al. Radiodermitis secundaria a procedimiento diagnóstico con signos de siringometaplasia escamosa ecrina. Actas Dermosifiliogr. 2013;104:255–7.