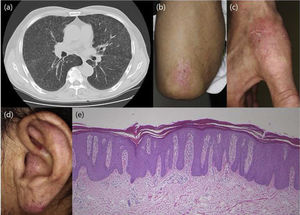
A 65-year-old man was admitted to the respiratory department of our hospital, for the detail investigation of bilateral hilar lymphadenopathy. Examination by lung computed tomography revealed lymph node adenopathy (Fig. 1) and bronchoscopic lung biopsy revealed non-caseating epithelioid granulomas, and thus he was diagnosed with sarcoidosis. Also, he was suffering from diabetes mellitus for five years previously. During admission, he was referred to our department complaining of itchy eruptions of the upper limbs and ears. He stated that he was diagnosed with psoriasis eight years previously and treated with topical corticosteroids but without sufficient effects. On physical examination, scaly erythematous plaques were scattered on the knees, elbows, fingers and ears. Nail involvement was not observed, and he had no arthritis. Skin lesions suggestive of sarcoidosis were not seen on the scalp, trunk and extremities including the knee. Results of laboratory examination elevated serum angiotensin converting enzyme (34.0 U/ml, normal; 8.3-21.4), sIL-2R (1850 U/ml,1–4 normal; 121-613) and negative tuberculin reaction. Neither ocular nor cardiac sarcoidosis was detected in detailed examination. Histological examination from the knee lesion showed regular epidermal proliferation, intraepidermal neutrophil infiltration, parakeratosis, dilated vessels in the dermal papilla, and perivascular cellular infiltrates. CD4− and CD8+ T-cells were detected in the epidermis and upper dermis. Sarcoid granulomas were not observed in the dermis or subcutis. The patient was treated with topical corticosteroid ointment.
The present patient first developed psoriasis, and five years later the diagnosis of sarcoidosis was made. He had been treated with topical therapy only, therefore it is unexpected that sarcoidosis was induced by medications for psoriasis. He had ocular and lung sarcoidosis, whereas cutaneous sarcoidal lesions were not observed, at least at the initial visit to our department. To date, several cases of co-existence of psoriasis and sarcoidosis have been reported1. Those cases usually present both cutaneous psoriatic and sarcoidal skin lesion, whereas our patient did not exhibit cutaneous sarcoidosis. T helper(Th)1 type cytokines are favored in the initial phase of sarcoidosis. In particular, tumor necrosis factor (TNF)-α is important in the formation of sarcoidal granuloma2. A shared TNF-α-mediated pathogenesis between psoriasis and sarcoidosis may exist. TNF-α activates Th17 cells to lead Interleukin (IL)-17 production, and IL-17 inflammatory pathway has been suggested to be important in psoriasis. Also, recent studies have suggested an important role of IL-17 in sarcoidosis, and enhanced expression of IL-17A+ interferon-γ+ and IL-17A+ IL-4+ memory T cells was shown in sarcoidal lungs3. Thus, Th17 profile has been implicated to play a role in sarcoidosis, possibly by inducing granuloma formation via suppression of regulatory T cells3. Another study showed upregulation of IL-23 and IL-21 in the lesions of cutaneous sarcoidosis4. In addition, pso p27 is a protein detected in mast cells in psoriatic lesions and extractable from psoriatic scales. Pso p27 is abundantly expressed in psoriatic lesional skin, and also expression of pso p27 is increased in the lungs of pulmonary sarcoidosis Figure 15. Role of pso p27 in sarcoidosis needs further studies.
Please cite this article as: Ishikawa M, Yamamoto T. Psoriasis en placa en un paciente con sarcoidosis. Actas Dermosifiliogr. 2021;112:865–866.