On December 31, 2019, the World Health Organization identified a novel coronavirus (SARS-CoV-2) in the city of Wuhan in China that spread very quickly and has to date resulted in the deaths of thousands of people by causing COVID-19 disease. Various Coronavirus disease-19 (COVID-19) associated dermatological manifestations have been reported. Among these, Pityriasis rosea (PR) and PR-like rash have been published previously. During the COVID-19 pandemic, the diagnosis of PR has become more common1–5.
PR is a self-limited inflammatory skin disease that can be induced viral agents especially HHV-6 (Human herpes virus 6), HHV-7 (Human herpes virus 7), autoimmunity, psychogenic factors, vaccines and drugs1,2.
We present here a case of PR in a confirmed COVID-19 pediatric patient.
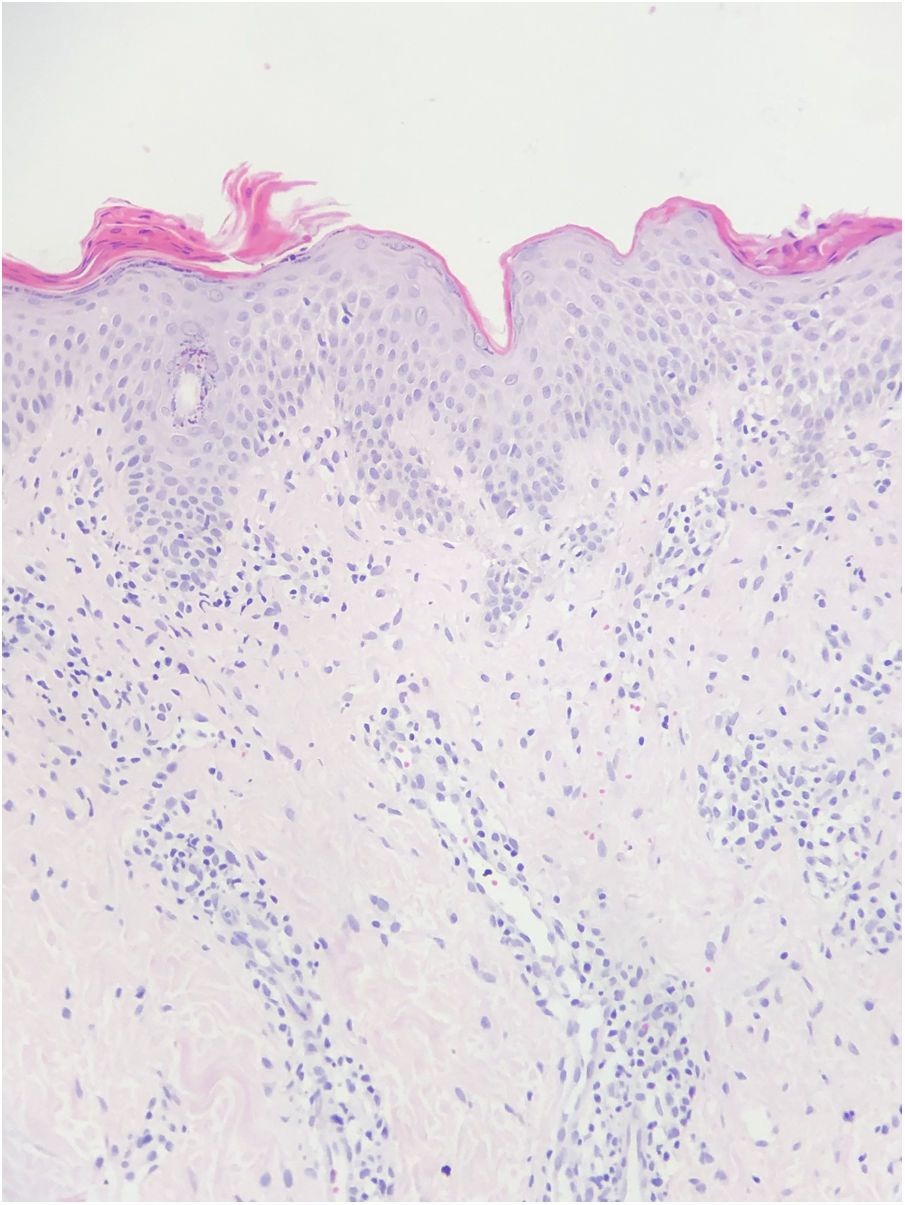
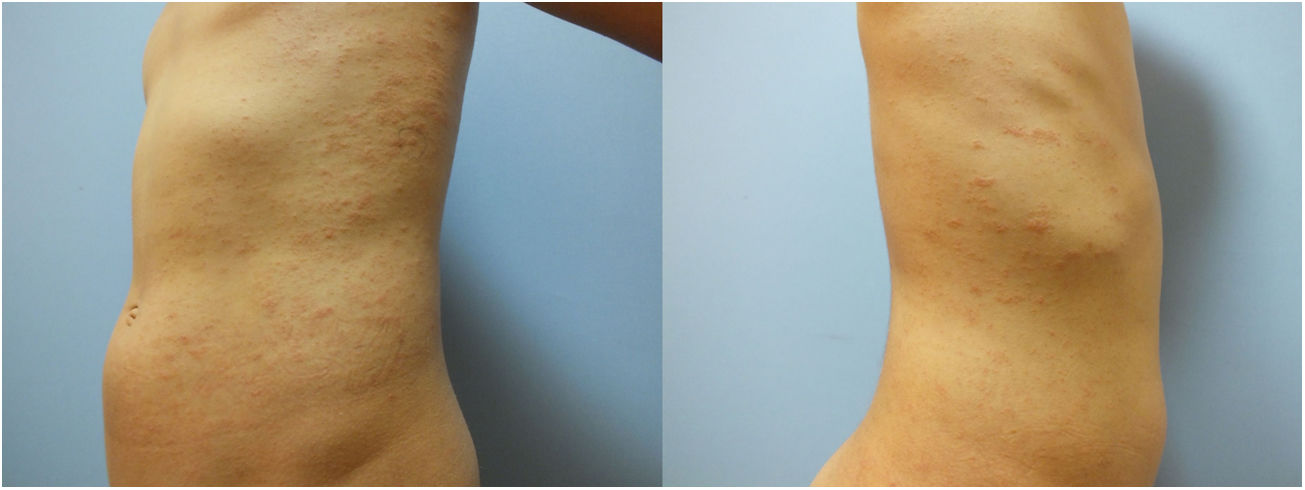
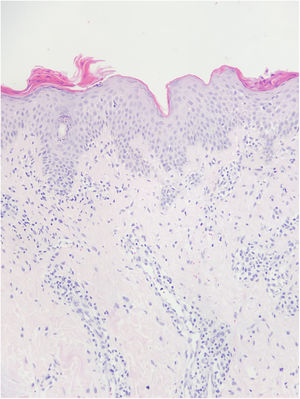
A 10-year-old boy presented with a 20-day history of skin rash. It was learned that he had Covid-19 infection about 1 month ago and he did not use any medication. In dermatological examination, there were small plaques with erythema and collary scaly located parallel to the ribs on the body (Fig. 1). Complete blood count, liver and kidney function tests, hepatitis markers, sedimentation and CRP values were in normal ranges. Histopathology of one lesion's biopsy showed focal parakeratotic peaks, spongiosis, focal spongiotic vesiculation, lymphocyte exocytosis, mildly irregular acanthosis with mild homogenization of collagen in the dermis, mild to moderate perivascular erythocyte infiltration in the superficial vascular plexus, scattered lymphocyte infiltration, sparse lymphocytes was seen (Fig. 2). The diagnosis of PR after Covid -19 infection was established with clinical and histopathologic findings. The patient was treated with betamethasone valerate ointment, 10% urea and cetirizine. Lesions regressed one month later.
The association between PR and COVID‐19 infection is not clearly known. In the literature, patients with confirmed COVID-19 developed PR and PR-like rash, some of them while asymptomatic or symptomatic disease, others after COVID-19 infection2–5. Therefore, in a patient presenting with PR and PR-like rash, it is necessary to keep in mind Covid-19 infection and suggest SARs-CoV-2 testing for necessary patients. PR could be directly dependent to COVID-19 infection, or to viral reactivation (HHV-6, HHV-7, EBV)1–5. In addition, the increased psychological stress caused by the pandemic period may have contributed to the trigger1. Due to the limited number of data, it is very difficult to prove a causal relation in these cases.
In conclusion, dermatologists should be aware that cutaneous symptoms may be linked to COVID-19 infection.
The patient and his family in this manuscript have given written informed consent to publication of his case details.
Please cite this article as: Öncü INS, Güler D, Gürel G, Yalçın GŞ. Pitiriasis rosada en un paciente pediátrico con diagnóstico confirmado de COVID-19. Actas Dermosifiliogr. 2021;112:864–865.