Pityriasis lichenoides (PL) is a skin disease of unknown origin that is characterized by scaling papules. It is relatively common in childhood but very rare in the first year of life, with just 9 cases described in the literature.
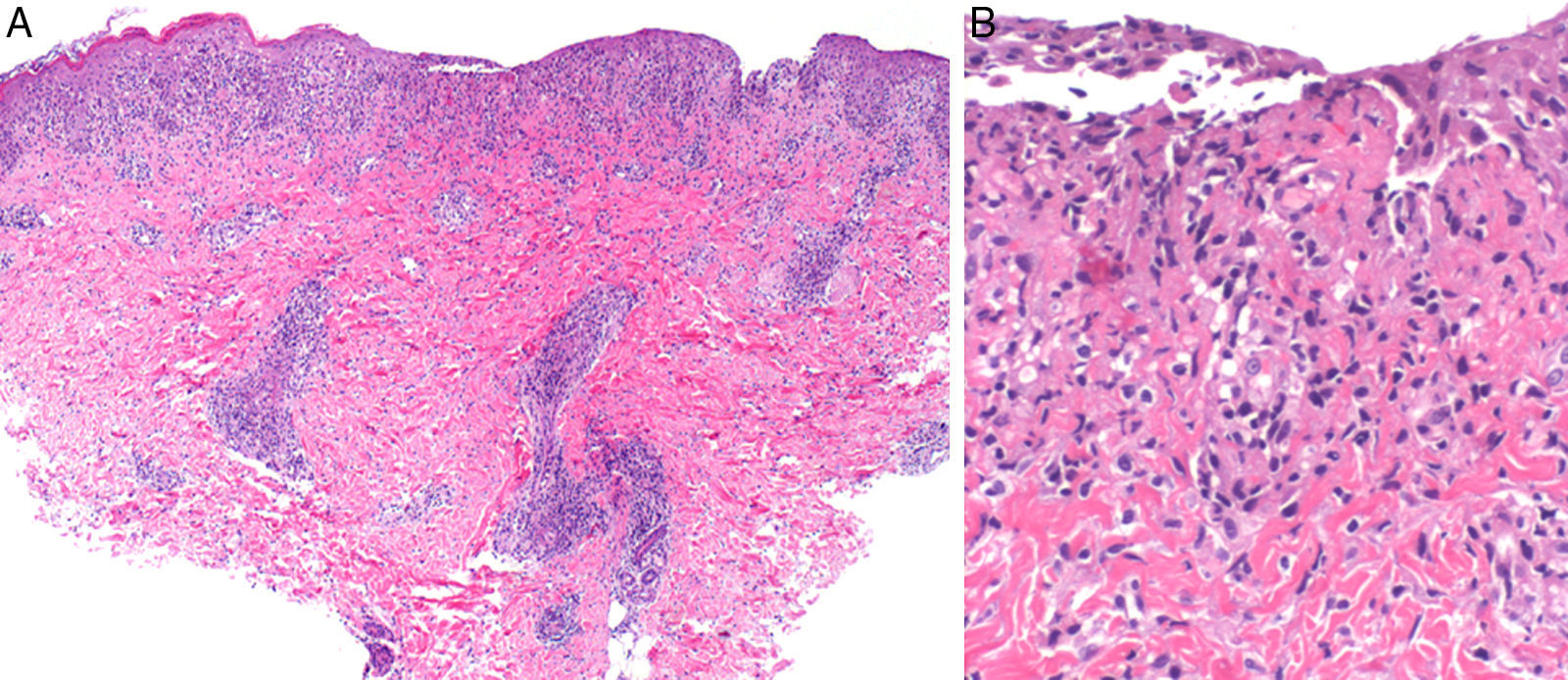
We report the case of a 9-month-old boy with no personal or family history of interest who was seen in our department for generalized skin lesions that had been present for a week. The patient was afebrile and had no other symptoms or known history of prior infection. Physical examination revealed papular scaling, erythematous-brownish lenticular lesions on the trunk and proximal extremities (Fig. 1). There was no mucosal involvement and the physical examination was otherwise normal. Histology showed a deep, perivascular lymphohistiocytic inflammatory infiltrate, with fibrinoid necrosis in the vessel walls and involvement of the dermal-epidermal junction. In the epidermis there was diffuse parakeratosis, focal exocytosis, isolated necrotic keratinocytes, and small foci of necrosis (Fig. 2). Immunohistochemical staining with anti-S100 protein and CD1 antibodies was negative. Based on the clinical and histologic findings, we diagnosed PL and prescribed topical corticosteroid therapy (methylprednisolone aceponate), which resulted in slight improvement of the lesions. The condition improved spontaneously over the following months, leaving residual postinflammatory hypopigmented macules.
A, Deep perivascular lymphohistiocytic inflammatory infiltrate with involvement of the dermal-epidermal junction (hematoxylin-eosin, original magnification ×10). B, Detail showing interface alteration, fibrinoid necrosis in the vessel walls, and isolated necrotic keratinocytes (hematoxylin-eosin, original magnification ×40).
PL is an inflammatory disease of unknown origin. There have been some reports of T-cell clonality, suggesting that the condition is either the result of an immune response to an as yet unidentified infectious agent or a cutaneous T-cell lymphoproliferative disorder.1 However, because progression to cutaneous T-cell lymphoma is so rare in children, additional genetic factors would probably need to be present. There are 2 clinical variants of PL: pityriasis lichenoides chronica and pityriasis lichenoides et varioliformis acuta (PLEVA). However, acute and chronic lesions may coexist. Histologic findings may also vary according to the clinical variant, but they do not always correlate with clinical morphology. Prognosis is excellent, and while PL can last for months, or even years, progression to T-cell lymphoma is very rare.2
PL can occur at any age, but it is particularly common in children, with incidence peaking at 2, 5, 10, and 12 years of age.3 It is very rare in the first year of life. In our review of the literature, we found only 9 cases of onset before the age of 12 months. These included 1 congenital case,4 3 cases with onset at 8 months of age,5–7 and 1 case with onset at 11 months of age.8 We also found mention of an additional 4 cases in children aged under 1 year in a retrospective study of 124 children with PL.3 In the 9 cases described in the literature, all the patients (8 boys and 1 girl) were otherwise healthy. There was just 1 case with a history of previous infection, in which pneumococci and Haemophilus influenza were isolated.6 Six of the patients had lesions clinically consistent with PLEVA, with ulceronecrotic lesions that resolved with topical corticosteroid therapy in a maximum of 2 months.3,7,8 The remaining 3 patients had lesions that were clinically and histologically consistent with PL chronica.4–6 The disease followed an indolent course in 2 patients, 1 of whom developed an indurated plaque in the right iliac fossa after a year and a half. The plaque was initially compatible with lymphomatoid papulosis but 2 years later, it was histologically diagnosed as cutaneous T-cell lymphoma.5 The second patient developed parapsoriasis at 10 years of follow-up.6
Given the scarcity of cases in the literature, no clear conclusions can be drawn, but based on our review, PL would appear to be very rare in children under 12 months of age, with just 10 cases, including ours, reported to date. Within this age group, PL is more common in boys and tends to occur in an acute form and to resolve spontaneously without complications. Nevertheless, given the possible association with lymphoproliferative disorders, long-term monitoring is recommended.
Please cite this article as: López-Villaescusa MT, Hernández-Martín Á, Colmenero I, Torrelo A. Pitiriasis liquenoide en un lactante de 9 meses. Actas Dermosifiliogr. 2013;104:829–830.