The main objective of dermatologic oncologic surgery is the surgical excision of a tumor with sufficient safety margins, allowing correct management thereafter. However, achieving the best functional and cosmetic result is a secondary objective that is acquiring ever greater importance, and that has even been extended to the excision of benign lesions, many of which are not included in the range of services offered by numerous hospitals.1
Several different surgical techniques have been developed to avoid wound dehiscence in the immediate and late postoperative periods. The conventional technique for which the best results have been reported is the one described by Weber and Wulc2 in 1992. That technique was modified and improved by Serrano et al.3 in 2015, hiding the entry and exit orifices of the suture by performing the subcutaneous vector-running suture along the length of the wound, completely burying the suture.
Based on the concept proposed by Serrano,3 we perform a continuous suture by tissue planes to prevent dehiscence of the wound and, thus, of the scar.4 Our wound closure consists of a continuous subcutaneous suture followed by an intradermal suture, demonstrated previously in the surgical videos section of Actas Dermo-Sifiliográficas.
This adaptable and simple technique enables us to control tension forces until the wound has healed. It is not necessary to remove the suture material. To avoid the formation of foreign body granulomas that can develop with nonabsorbable sutures, we use a mid-term absorbable suture: Novosyn 3/0, a mid-term absorbable multifilament synthetic suture of braided and coated poly(glycolide-co-L-lactid 90/10). Two additional advantages of this technique are that it is rapid to perform and that no assistant is needed to cut the suture material after each stitch.5
Between January and December, 2015, we performed a prospective nonrandomized pilot study in our unit to determine dehiscence in the immediate postoperative period and in the mid-term using the technique described above and the one employed in conventional surgery. The study was approved by the ethics committee of our hospital. All patients were over 18 years of age. The variables gathered were sex, age, clinical diagnosis, length and breadth of the incision, and width of dehiscence at 3 and 6 months. All the lesions excised were on the trunk or root of the thighs.
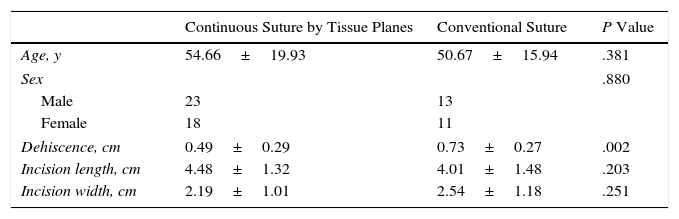
A descriptive analysis was performed of the overall population and by groups after testing for normality of the continuous quantitative variables using the Kolmogorov-Smirnov test. Variables were compared using the Student t test or Welch test for normal variables and the Mann Whitney U test for non-normal variables. The χ2 test was used to study associations between qualitative variables. Sixty-five patients were included in the study. Wound closure was performed with the continuous suture by tissue planes in 37 patients and with the conventional Weber technique in 28 (Table 1). No statistically significant differences were found between the 2 groups in the variables age, sex, and length and breadth of the incision. Wounds closed using the continuous suture by tissue planes presented a mean dehiscence of 4.88mm, whereas mean dehiscence in the conventional suture group was 7.25mm; this difference was statistically significant (P=.002).
Comparison of the 2-Suture Techniques Performed in the Study Patients.
| Continuous Suture by Tissue Planes | Conventional Suture | P Value | |
|---|---|---|---|
| Age, y | 54.66±19.93 | 50.67±15.94 | .381 |
| Sex | .880 | ||
| Male | 23 | 13 | |
| Female | 18 | 11 | |
| Dehiscence, cm | 0.49±0.29 | 0.73±0.27 | .002 |
| Incision length, cm | 4.48±1.32 | 4.01±1.48 | .203 |
| Incision width, cm | 2.19±1.01 | 2.54±1.18 | .251 |
No infectious complications were observed in the immediate or late postoperative periods with either of the 2 techniques after strict adherence to the pre- and postsurgical verification protocols applied in our hospital.6
The main limitation of our pilot study is that comparison of the 2 surgical techniques was not performed in patients with paired sites and randomization to the treatment groups. It should also be noted that this suture technique is designed for use in areas of high tension, such as the trunk and limbs, though initially all body regions were included. Results in the late postoperative period are not yet available. However, it is clear that dehiscence with our technique is less marked that with conventional surgery.
This is a novel line of research,7 and a recent publication has reported on new systems of nontraumatic wound closure that have been tested in a prospective randomized controlled clinical study.8 All the lesions were on the trunk and limbs, and although there were no statistically significant differences in the cosmetic result, dermal suture appears to be necessary to approximate the epidermal borders of the wound when using such a device. The device can be removed by the patient, and the time required to perform the suture is clearly lower, but further studies, such as ours, are needed to evaluate the improvement in risk of dehiscence.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Gonzalo Blasco Morente and Dr. Cristina Garrido Colmenero for their help in performing this study.
Please cite this article as: Tercedor-Sánchez J. Estudio piloto de valoración de dehiscencias posquirúrgicas tras sutura continua por planos. Actas Dermosifiliogr. 2017;108:371–372.