A 28-year-old man with no relevant past medical history consulted for a progressive, slow-growing exophytic lesion at the edge of the nail of the middle finger on the left hand. The lesion had been present for 2 years. The patient reported that he had had multiple sexual partners up to 6 years earlier.
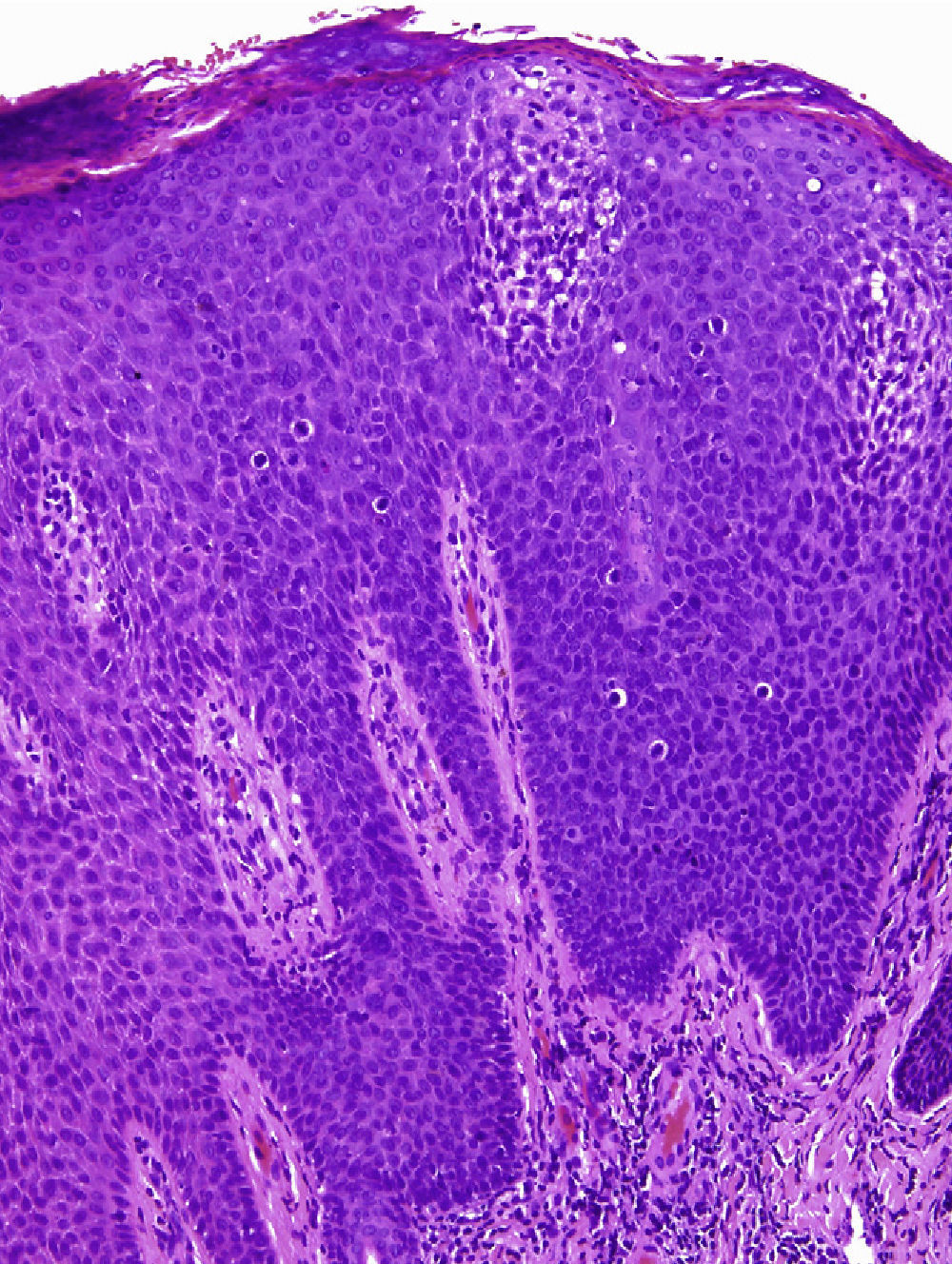
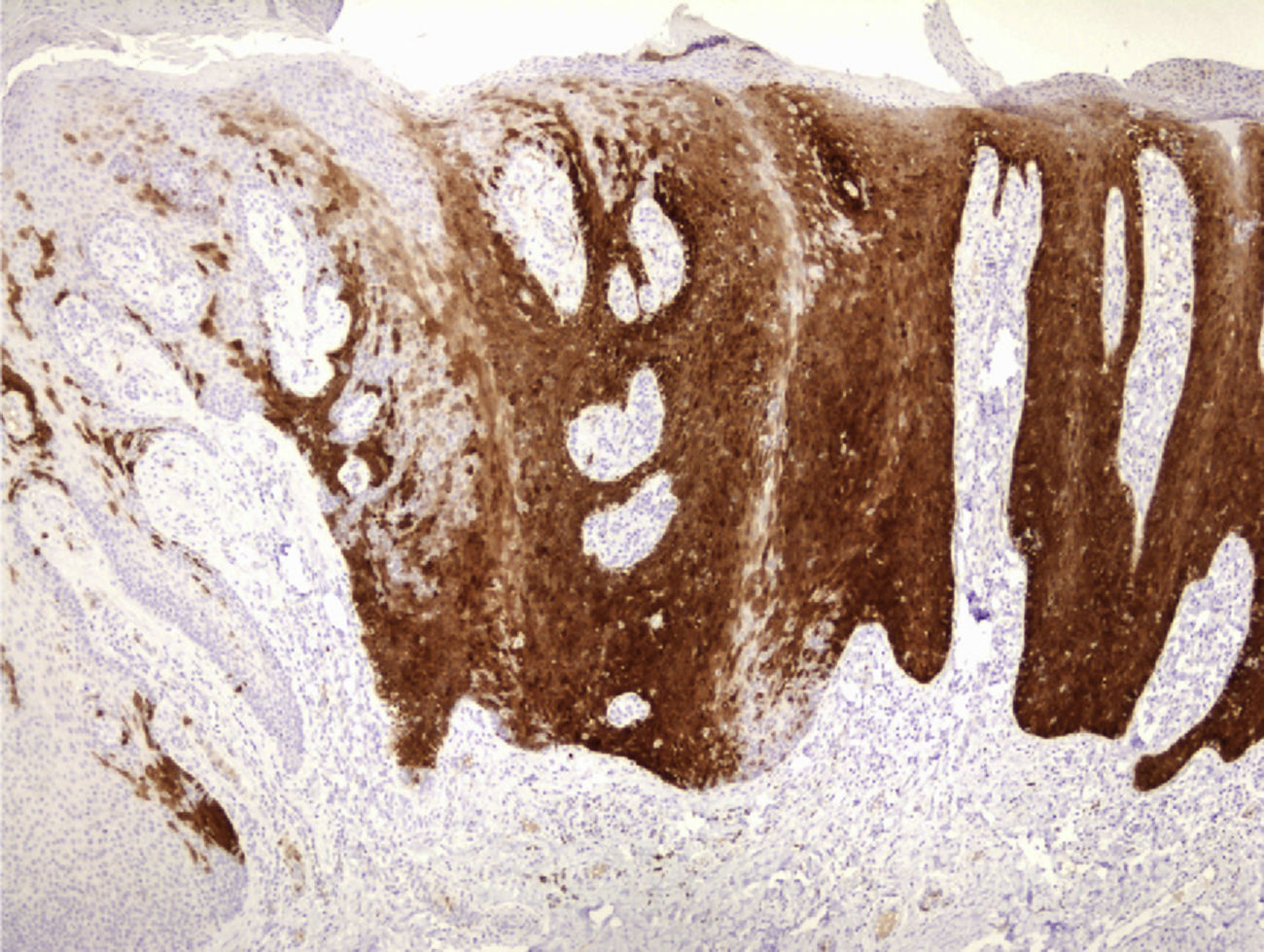
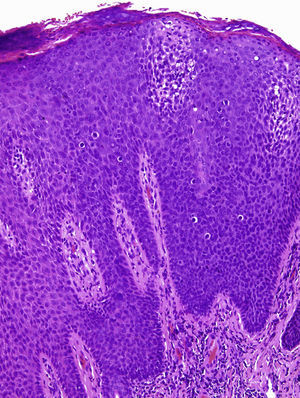
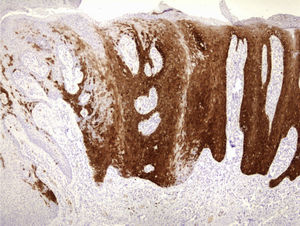
Physical examination revealed a red-grayish exophytic periungual lesion measuring 0.7cm in diameter with a hyperkeratotic surface (Fig. 1). Histopathologic examination showed a hyperplastic epidermis with loss of normal cell architecture, moderate cellular atypia, dyskeratosis, and koilocytes in the epidermis (Fig. 2). Overexpression of the tumor suppressor protein p16 was also observed (Fig. 3). Based on a diagnosis of extragenital bowenoid papulosis, the patient was re-questioned, but he reported that neither he nor his current partner had had genital or anal warts. Lymphocyte counts (including CD4 and CD8 counts) were normal and serologic testing for human immunodeficiency virus (HIV) was negative. Human papillomavirus (HPV) DNA testing using the hybrid capture assay detected HPV 42. It was decided to excise the entire lesion and schedule periodic follow-up visits for the patient and his partner. The patient was asymptomatic a year after diagnosis.
The term bowenoid papulosis was introduced to describe multiple wart-like papules in the genital region that are histologically similar to Bowen disease and clinically similar to genital warts. The condition typically affects young, sexually active individuals and mainly involves the genital, crural, and perianal regions. However, there have also been reports of extragenital bowenoid papulosis with or without concomitant genital lesions in both immunocompetent and immunodeficient patients.1
Bowenoid papulosis is associated with HPV infection. While there is a close link with HPV 16 infection,1,2 types 18, 31-35, 39, 42, 48, and 51-54 have also been implicated.1–4 HPV 16, 18, and 33 are considered to have the greatest oncogenic potential.
Bowenoid papulosis is considered to be a squamous cell carcinoma in situ and has an estimated risk of malignant transformation of 2.6%.2 The oncogenic mechanism is probably initiated by HPV-induced genetic changes in infected cells. High-risk serotypes produce HPV oncoproteins E6 and E7, which are capable of inactivating the Rb and p53 tumor suppressor proteins, respectively, giving rise to uncontrolled cell proliferation.4 HPV has been detected in bowenoid papulosis lesions and adjacent healthy skin, indicating that HPV infection is a necessary but not sufficient factor in the development of bowenoid papulosis. Other alterations, such as additional genetic mutations in the host cell, may be necessary.3,4
Bowen papulosis is histologically similar to Bowen disease, but exhibits more focal and less intense changes.1,5,6 To distinguish between the 2 entities, it is always necessary to correlate clinical and histologic findings.
The prevalence of Bowenoid papulosis is unknown, as the lesions are commonly confused with other wart-like lesions and are frequently destroyed without histological examination.7 Since the lesions tend to recur and have malignant potential, patients and their sexual partners should be referred for periodic follow-up and an immunological study in the case of persistent or recurrent lesions.7 The clinical course is variable, with some lesions progressing to chronic or malignant forms and others spontaneously regressing. Conservative treatment involving destruction of the lesions by simple excision, electrocoagulation, or cryosurgery is the most effective therapeutic approach.6,8
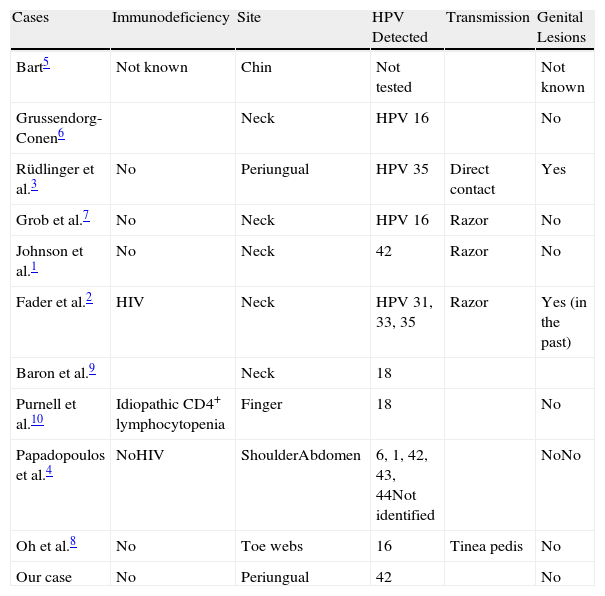
Bowenoid papulosis generally occurs with concomitant genital lesions or in patients with a history of HPV-induced lesions8–10 (Table 1).Transmission is believed to occur through direct contact, autoinoculation, or fomites.1,2,7,9 These transmission mechanisms would explain the involvement of different parts of the body. Reports in the literature describe lesions affecting the neck, the abdomen, the shoulder, the chin, and the periungual area, among others.1–10
A Selection of Published Cases of Extragenital Bowenoid Papulosis.
| Cases | Immunodeficiency | Site | HPV Detected | Transmission | Genital Lesions |
| Bart5 | Not known | Chin | Not tested | Not known | |
| Grussendorg-Conen6 | Neck | HPV 16 | No | ||
| Rüdlinger et al.3 | No | Periungual | HPV 35 | Direct contact | Yes |
| Grob et al.7 | No | Neck | HPV 16 | Razor | No |
| Johnson et al.1 | No | Neck | 42 | Razor | No |
| Fader et al.2 | HIV | Neck | HPV 31, 33, 35 | Razor | Yes (in the past) |
| Baron et al.9 | Neck | 18 | |||
| Purnell et al.10 | Idiopathic CD4+ lymphocytopenia | Finger | 18 | No | |
| Papadopoulos et al.4 | NoHIV | ShoulderAbdomen | 6, 1, 42, 43, 44Not identified | NoNo | |
| Oh et al.8 | No | Toe webs | 16 | Tinea pedis | No |
| Our case | No | Periungual | 42 | No |
Abbreviation: HIV, human immunodeficiency virus; HPV, human papillomavirus.
We have reported a new case of bowenoid papulosis affecting the periungual area of a finger in a patient with no past or present history of genital lesions. Two similar cases of extragenital bowenoid papulosis have been reported in the literature. One of the patients had bowenoid papulosis lesions in the perianal area that were detected on diagnosis of the nail lesion10 and the other patient had HIV infection.4 We believe that lesions in young sexually active patients should be examined histologically, even when they are located at a distance from the genital region. The possibility of immunosuppressive conditions should be investigated, as should the presence of genital lesions in the patients and their partners.
Please cite this article as: Gómez Vázquez M, Navarra Amayuelas R. Papulosis bowenoide periungueal por virus del papiloma humano 42. Actas Dermosifiliogr. 2013;104:932–934.