Bowenoid papulosis of the genitalia in immunocompromised patients is associated with a high risk of recurrence and transformation to infiltrating squamous cell carcinoma on the one hand, and poor response to treatment on the other.1,2
We describe the case of a 50-year-old female smoker diagnosed with human immunodeficiency virus (HIV) infection in 1989 and invasive cervical cancer in 2000. She also had chronic hepatitis C infection complicated by cirrhosis. She had had histopathologically confirmed bowenoid papulosis since 2004. Treatments had included electrocoagulation, cryotherapy, podophyllin resin, as well as imiquimod, but with poor response and tolerance.
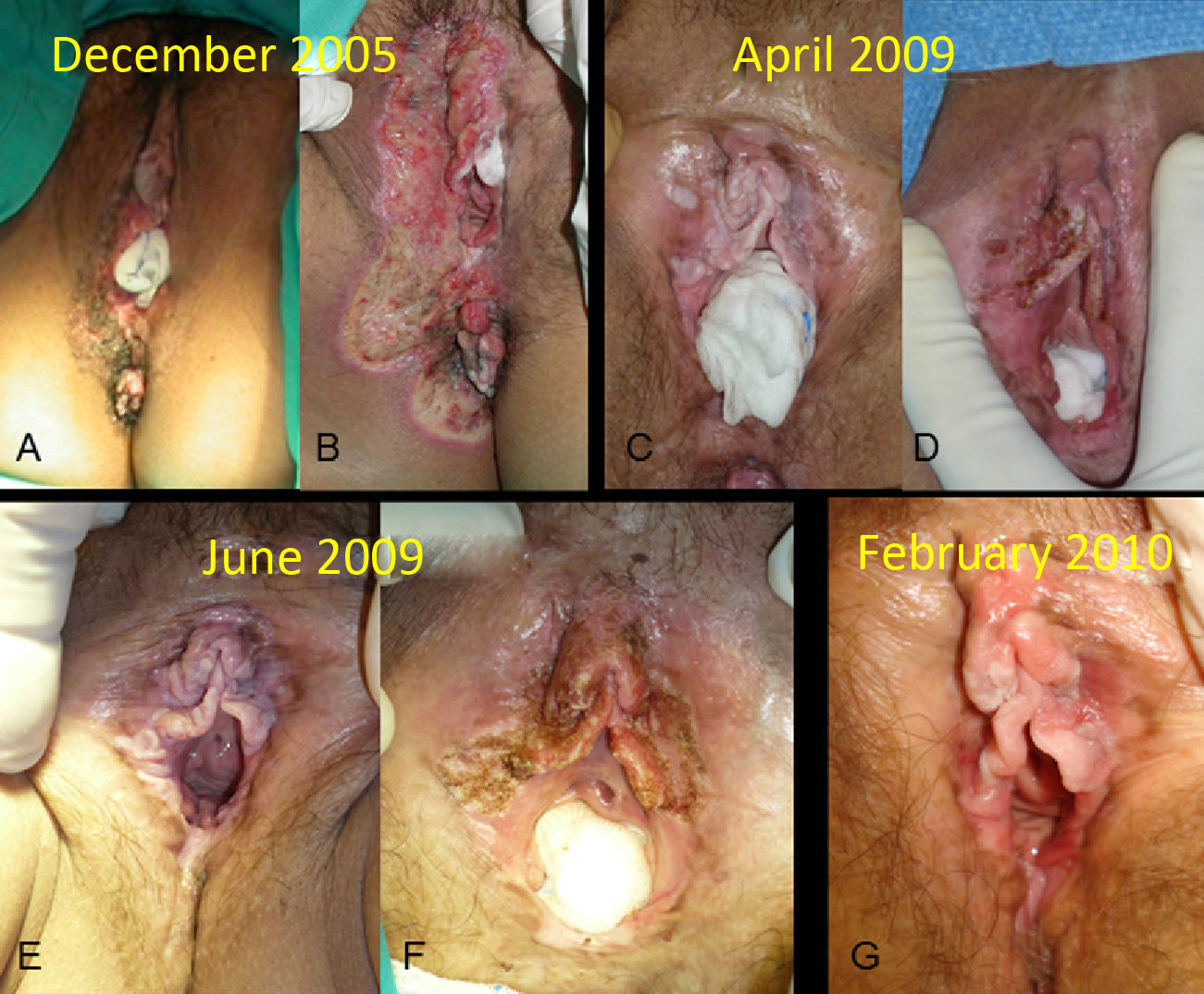
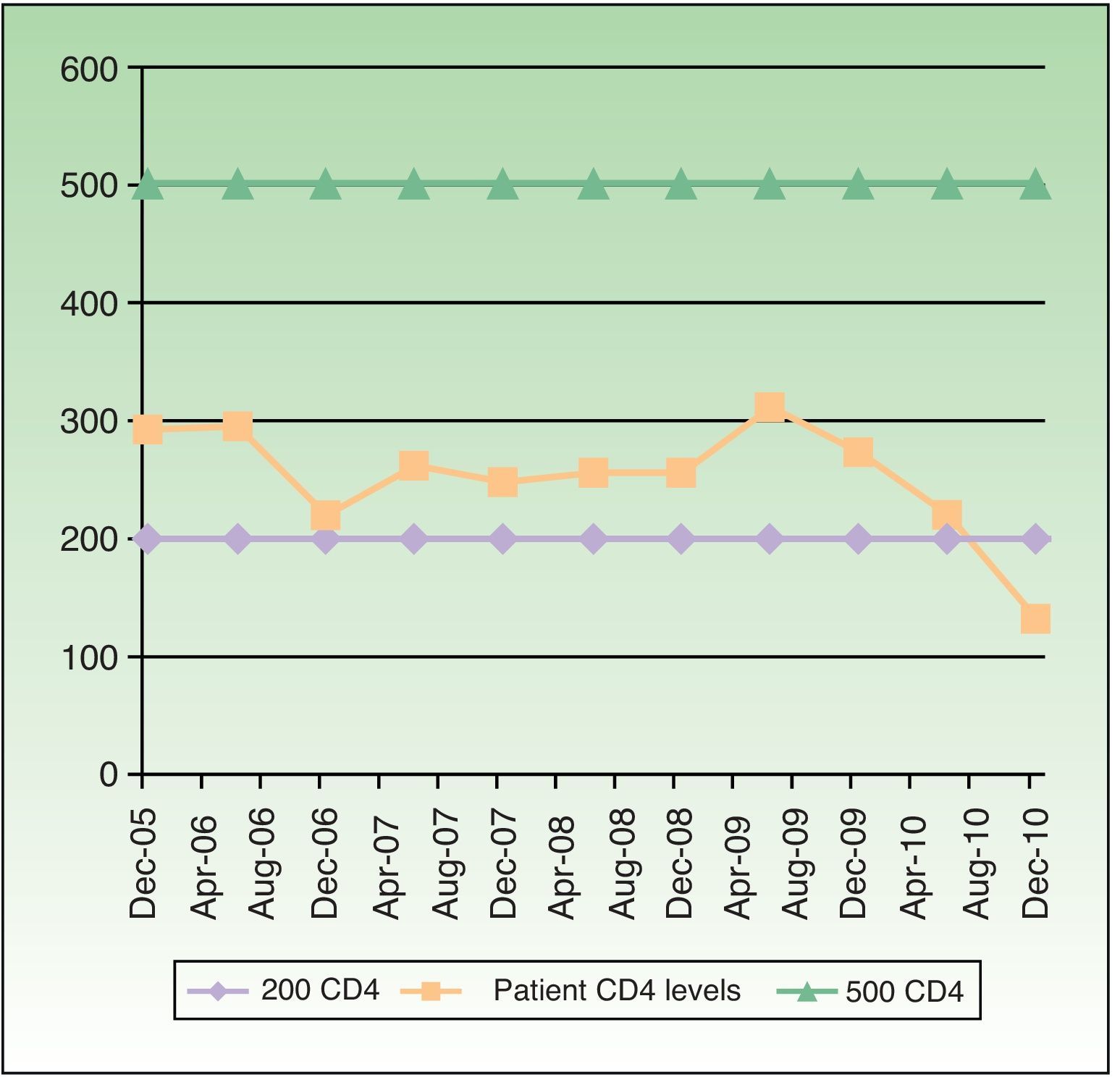
When the patient first visited our hospital in March 2005, she had a brownish plaque with well-defined borders and a verrucous surface covering almost the entire area of the external genitalia and the perianal area (Fig. 1A). A new biopsy confirmed the diagnosis of bowenoid papulosis. In December 2005, we decided to administer continuous-wave carbon dioxide (CO2) laser therapy at a power of 7.5 W to treat the affected area and the acetowhite lesions identified; a lateral safety margin of 4 to 5 mm was also treated due to the possible presence of subclinical human papillomavirus (HPV) infection. The procedure was performed with the patient under epidural anesthesia. The treated areas were subsequently cleaned and dressed with an antibiotic ointment, and prophylactic valacyclovir was prescribed at a dose of 500 mg every 8hours until complete reepithelization. Total clinical resolution of the lesions was observed at 1 month. The patient underwent follow-up examinations every 3 to 6 months, in addition to 4 treatment sessions with the same anesthesia, fluence, and postoperative care in October 2006, December 2007, April 2009, and June 2009. Complete clinical resolution was achieved each time (Fig. 1 B-G). The patient's CD4 count during follow-up is shown in Fig. 2. The control biopsies showed typical features of bowenoid papulosis, with no signs of infiltrating squamous cell carcinoma. During follow-up, the patient was diagnosed with hepatocellular carcinoma in 2008 and with a high-grade anal neoplasm in 2009. The respective treatments were chemoembolization and surgery followed by consolidation radiation therapy.
A, Multiple brownish flattened lesions on the vulva. B, Wound with granulation tissue 10 days after laser treatment. C, New whitish velvety plaques diagnosed as bowenoid papulosis (April 2009). D, Postoperative result following the second treatment session with carbon dioxide laser. E-G, Subsequent instances of recurrence, controlled with treatment.
In all, over a period of 6 years we performed 5 sessions of CO2 laser therapy, the last of which was in April 2009; no adverse effects were observed in any of the sessions. The patient remained free of lesions in the vulvar area from September 2009 until December 2010, when she died following progression of her hepatocellular carcinoma. The only treatment required during this period was cryotherapy of isolated lesions in the area.
CO2 laser therapy causes minimal postoperative pain3 and produces better cosmetic results than other methods, especially when used on the external genitals.4 It has been used since 1988 to treat large bowenoid papulosis lesions that are difficult to treat with other methods.5 The primary complications described to date are vesicovaginal fistulas6 and vulvodynia, especially of the posterior commissure or the vulval vestibule.7 CO2 laser therapy for bowenoid papulosis lesions achieves complete response, and the rate of recurrence is between 12.5% and 21%.8 The cure rate appears to be lower (just 34.5%) in HIV-positive patients, in whom HPV infection persists.9 Differences in cure rates are less substantial in condylomas treated with CO2 laser.10 In our case, due to the slight fluctuations in CD4 count during follow-up, it is reasonable to rule out an improvement in symptoms due to immune recovery. A number of approaches have been used to treat bowenoid papulosis in immunocompromised patients, such as electrocoagulation, cryotherapy, 5-fluorouracil, intralesional interferon gamma, imiquimod, podophyllin resin, CO2 laser, and Nd:YAG laser. However, the effectiveness of these treatments is difficult to assess due to the scarcity of cases in the literature.
As evidenced in the present case, immunocompromised patients are more susceptible to HPV-related neoplasms. We have presented this case because we achieved a good clinical response and high patient satisfaction with the cosmetic outcome after only 5 treatment cycles and with no adverse effects. In light of these results, CO2 laser therapy may be considered an appropriate treatment for immunocompromised patients with extensive and recurrent lesions.
Please cite this article as: Llamas-Velasco M, Vargas E, Delgado Y, García-Diez A. Tratamiento con láser de dióxido de carbono de una papulosis bowenoide vulvar extensa en paciente con sida. Actas Dermosifiliogr. 2013;104:934–936.