Pemphigoid gestationis is a relatively rare autoimmune blistering disease that occurs during pregnancy. In very rare cases this process can be complicated by the appearance of generalized lesions with involvement of the oral mucosa.
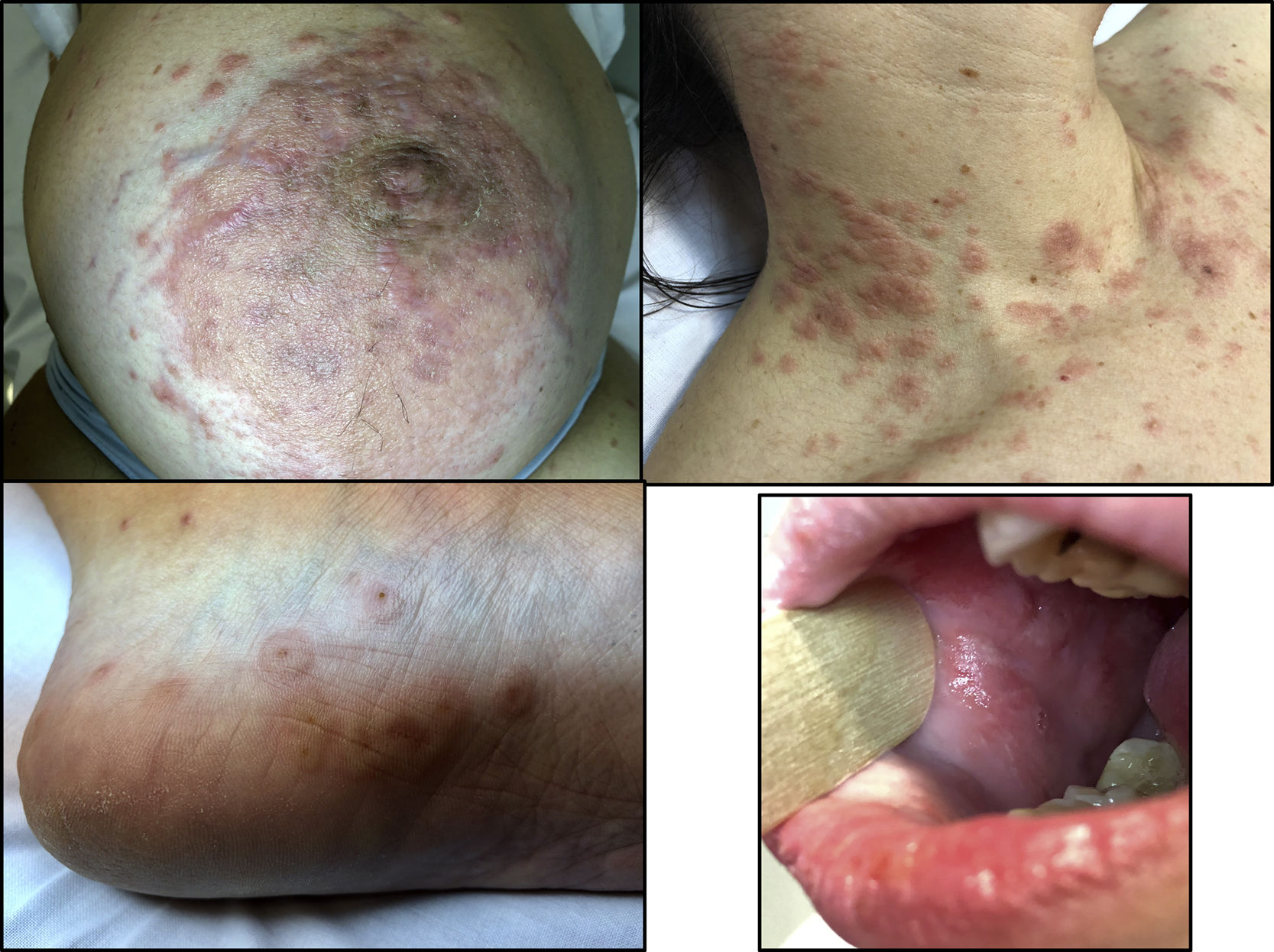
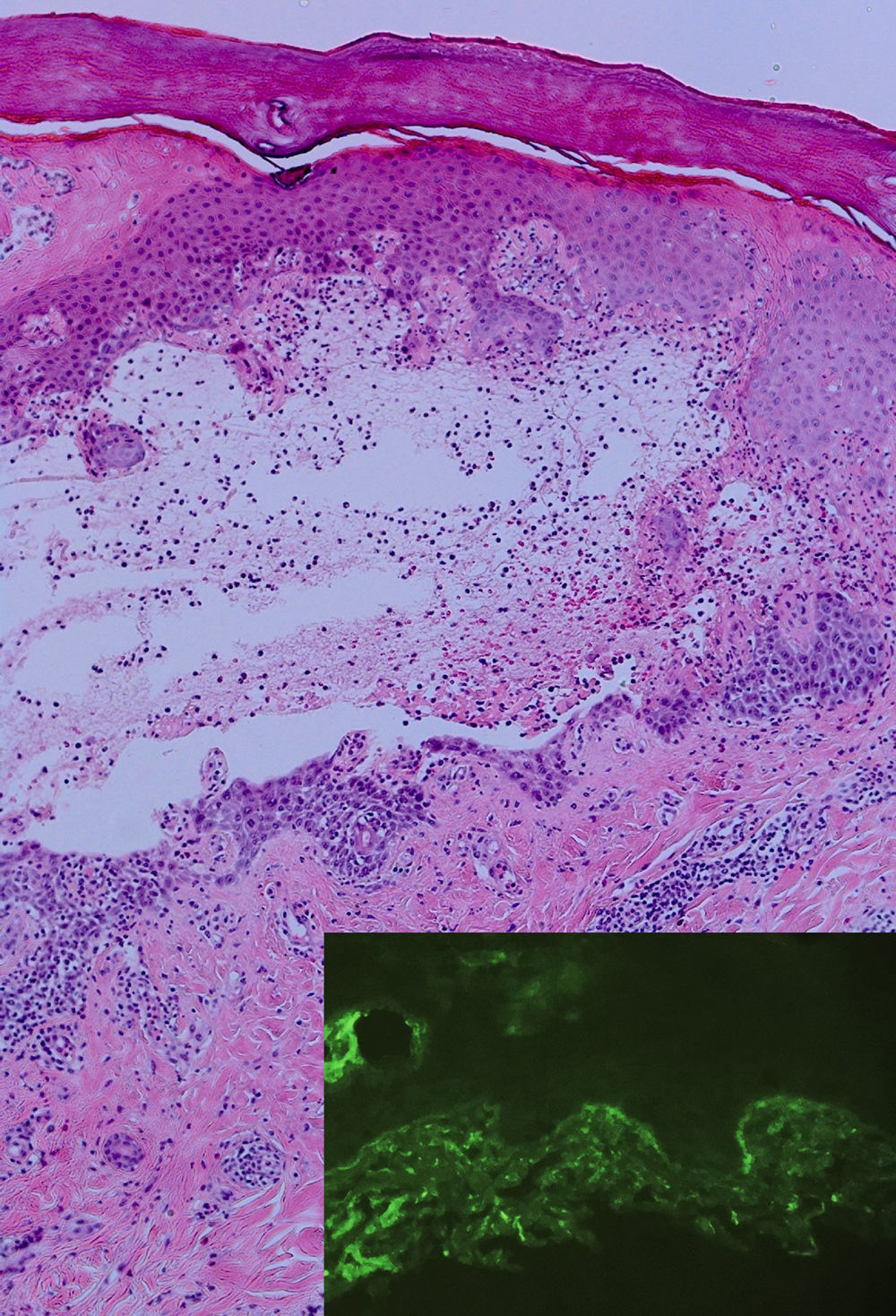
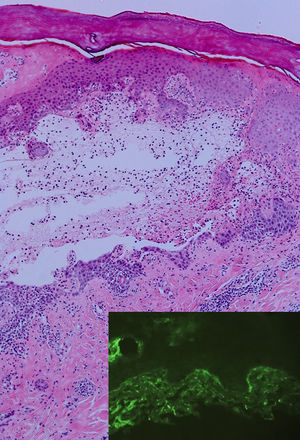
A healthy, 33-year-old woman in week 35 of her second pregnancy with the same partner was seen for generalized and buccal lesions. The patient reported no previous infectious processes and had not begun treatment with any new medications. Physical examination revealed large, erythematous-edematous plaques around the umbilicus and on the neck. Exudative erythema multiforme-like lesions were observed on the palms and soles, and extensive erosions without vesicles or blisters on the oral mucosa (Fig. 1). Skin biopsy revealed a subepidermal blister with eosinophilic spongiosis, without vacuolar degeneration of the epidermal basement membrane (Fig. 2). Direct immunofluorescence showed linear focal deposits of complement component 3 (C3) in the basement membrane. No anti-BP180 antibodies were detected by indirect immunofluorescence. Serology for Mycoplasma pneumoniae was negative for immunoglobulin (Ig) M and IgG. The patient began corticosteroid treatment with oral prednisone (0.75 mg/kg/d) and topical 0.05% clobetasol propionate cream. The lesions progressively improved and finally disappeared 2 months after the patient gave birth, leaving residual pigmentation. The baby was delivered without complications (eg, preterm birth, low birth weight) and without skin lesions. After 6 months of follow-up the patient remained free of lesions.
Pemphigoid gestationis, formerly known as herpes gestationis, is a rare autoimmune blistering disease associated with pregnancy. It usually occurs during the second or third trimester of pregnancy (68% of cases), with incidence ranging from 1 per 20,000 to 1 per 50,000 population, and tends to resolve after childbirth, although flare-ups can occur after delivery and during menstruation.1
The lesions begin as pruritic urticarial papules and plaques that rapidly evolve to vesicles but rarely progress to large blisters. In up to 65% of cases lesions initially appear in the periumbilical area, subsequently spreading to other areas including the abdomen, legs, arms, palms, and soles.2 A case series by Hallaji and coworkers2 reported no instances of mucosal involvement. In another case series, Castro et al3 reported involvement of the hard palate mucosa in 1 patient and of the genital mucosa in another. However, neither of those articles specify whether the aforementioned involvement consisted of erosions, ulcers, blisters, or vesicles. Another peculiarity in our case was the appearance on the patient's palms and soles of exudative erythema multiforme-like lesions, which are sporadically but infrequently described in the literature.1
Histological findings depend on the intensity and stage of evolution of the lesions. The presence of abundant eosinophils is a consistent finding in pemphigoid gestationis. The key finding in the blistering phase is the presence of a subepidermal blister in the basement membrane. In 100% of cases direct immunofluorescence reveals the presence of linear C3 deposition along the basement membrane. Deposition of IgG1 is observed in 25% to 30% of cases. Depending on the technique used, indirect immunofluorescence can detect IgG against the BP180 antigen in 30% to 100% of cases. However, titers do not always correlate with disease activity.
The first disease that should be included in the differential diagnosis is pruritic urticarial papules and plaques of pregnancy (PUPPP). The absence of striae gravidarum and the presence of periumbilical lesions in pemphigoid gestationis can facilitate distinction of pemphigoid gestationis from PUPPP. Pemphigoid gestationis should also be distinguished from other blistering diseases that can occur during pregnancy, including bullous pemphigoid, dermatitis herpetiformis, linear IgA disease, bullous systemic lupus erythematosus, exudative erythema multiforme, toxic drug reaction, and contact dermatitis.
Prednisolone (0.5–1 mg/kg/d) is one of the most effective and safest forms of treatment during pregnancy. Prolonged systemic corticosteroid therapy can result in an increased incidence of preterm birth or low birth weight. In cases of refractory and progressive pemphigoid gestationis other therapeutic options such as immunoglobulin or ciclosporin treatment can be considered, always bearing in mind the potential risk to the fetus.4,5 It should be noted that more severe flare-ups can occur during subsequent pregnancies or in conjunction with contraceptive use.6 In general the fetal prognosis is good: mild involvement in the form of wheals or vesicles is reported in 10% of cases.
In conclusion, we present a case of pemphigoid gestationis, confirmed by histology and direct immunofluorescence, with extensive exudative erythema multiforme-like lesions and involvement of the oral mucosa. Oral involvement in this type of blistering disease is very infrequent.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Lobato-Berezo A, Fernández Figueras MT, Moreno Romero JA, Pujol RM. Pemphigoid Gestationis Mimicking Erythema Multiforme With Mucosal Involvement. Actas Dermosifiliogr. 2019;110:696–697.