Patients receiving treatment for tuberculosis may experience an unexpected deterioration of their disease; this is known as a paradoxical reaction. We present the case of a 59-year-old man with lupus vulgaris who experienced a paradoxical deterioration of cutaneous lesions after starting antituberculosis therapy. The reaction was self-limiting; the lesions gradually improved, and the final outcome was very good. Paradoxical reactions are well-known in patients with human immunodeficiency virus (HIV) infection who start antiretroviral therapy, but they can also occur in non–HIV-infected patients with tuberculosis who start antituberculosis therapy. In the literature reviewed, paradoxical reactions involving skin lesions were described in patients with miliary tuberculosis. The case we report is the first of a paradoxical reaction in lupus vulgaris. The increasing frequency of tuberculosis in Spain could lead to a rise in the number of paradoxical reactions.
Los pacientes diagnosticados de tuberculosis que reciben tratamiento antituberculoso pueden presentar un empeoramiento inesperado de su enfermedad, conocido como respuesta paradójica. Presentamos el caso de un varón de 59 años, con diagnóstico de lupus vulgar, que presentó un intenso empeoramiento paradójico de sus lesiones cutáneas tras iniciar tratamiento antituberculoso. Este fenómeno fue autolimitado, presentando mejoría progresiva con muy buena evolución final. La respuesta paradójica es un fenómeno conocido en pacientes infectados por el VIH tras iniciar tratamiento antirretroviral, y que también puede aparecer en pacientes no infectados por el VIH con tuberculosis que comienzan tratamiento antituberculoso. En la revisión de la literatura que se ha realizado los casos descritos con afectación tuberculosa cutánea y respuesta paradójica se refieren a tuberculosis miliar, siendo el que describimos el primero en lupus vulgar. El aumento de casos de tuberculosis en nuestro medio podría dar lugar a un aumento de la frecuencia de estas situaciones de empeoramiento paradójico.
Lupus vulgaris is the most frequent form of presentation of cutaneous tuberculosis in Europe.1,2 Lesions are most frequently found on the head and neck2 and present in patients who are highly sensitive to tuberculin.2 Infection follows a chronic course and can be very destructive. Diagnosis of tuberculosis infection is made using methods such as the Mantoux test and/or the QuantIFERON TB gold in-tube test. Diagnosis of cutaneous tuberculosis can be made by histopathology, culture, and identification of DNA through polymerase chain reaction (PCR).1,3 Lupus vulgaris is a paucibacillary form of cutaneous tuberculosis, and so techniques such as Ziehl-Neelsen staining may be negative and a negative result does not rule out diagnosis of tuberculosis.1,3 The same occurs with culture in mycobacterial media of cutaneous samples from patients with lupus vulgaris. Positive findings are reported in only 6% of cases,1 with a PCR sensitivity ranging from 50% to 74% according to a number of studies.1,3,4 The negative findings may be explained by the paucibacillary nature1 and the nonhomogeneous distribution of bacilli.3 According to the literature, factors that may be implicated in negative findings in the QuantIFERON TB gold in-tube test are presence of comorbidities and underlying immunosuppression, erroneous test conduct, and extrapulmonary site of tuberculosis infection.5 However, although these methods may give negative results in cases of cutaneous tuberculosis, a high degree of clinical suspicion, along with compatible histopathological lesions in skin biopsy and a satisfactory clinical response to tuberculosis treatment may also be considered a criterion for diagnosis.3 For treatment of lupus vulgaris, the same regimens are recommended as for pulmonary tuberculosis and tuberculosis infection at other sites. Paradoxical responses (PRs) in different diseases after initiating appropriate treatment have been widely published in patients with human immunodeficiency virus (HIV) infection, but such response is less common in non–HIV-infected patients with tuberculosis. The cases published regarding skin involvement due to paradoxical worsening make reference above all to miliary tuberculosis.6–8 We report the case of a patient diagnosed with lupus vulgaris who presented with paradoxical worsening after receiving tuberculosis treatment and review the literature on this phenomenon.
Case DescriptionA 59-year-old man presented with facial lesions which first appeared in 2008 and were assessed in another clinic. He was diagnosed with CD30+ large-cell lymphoma. After this diagnosis was made, he had received treatment with methotrexate at variable doses ranging from 5 to 20mg/week for 4 years, but without any improvement. He was finally referred to our clinic in 2012 to assess the possibility of radiotherapy. Previously, he had undergone 2 computed tomography studies (in 2008 and 2011) of the neck/chest/abdomen-pelvis, with normal findings.
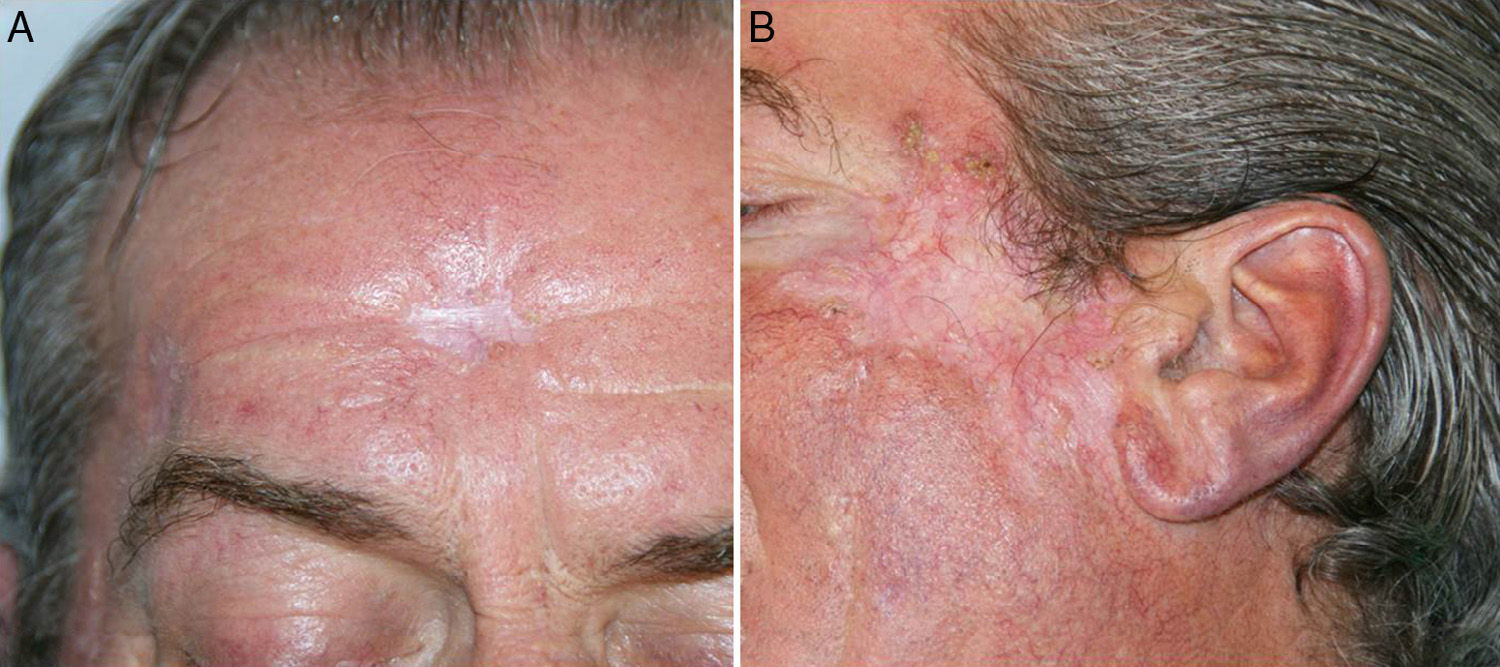
When assessed in our clinic, the patient had an extensive depressed plaque with central scarring and a raised border, measuring 6.5cm across along the long diameter, in the left zygomatic region (Figure 1). He also had 3 residual scars in the central frontal area and the right temple. There were no other lesions elsewhere on the skin nor enlarged lymph nodes in the main lymphatic territories.
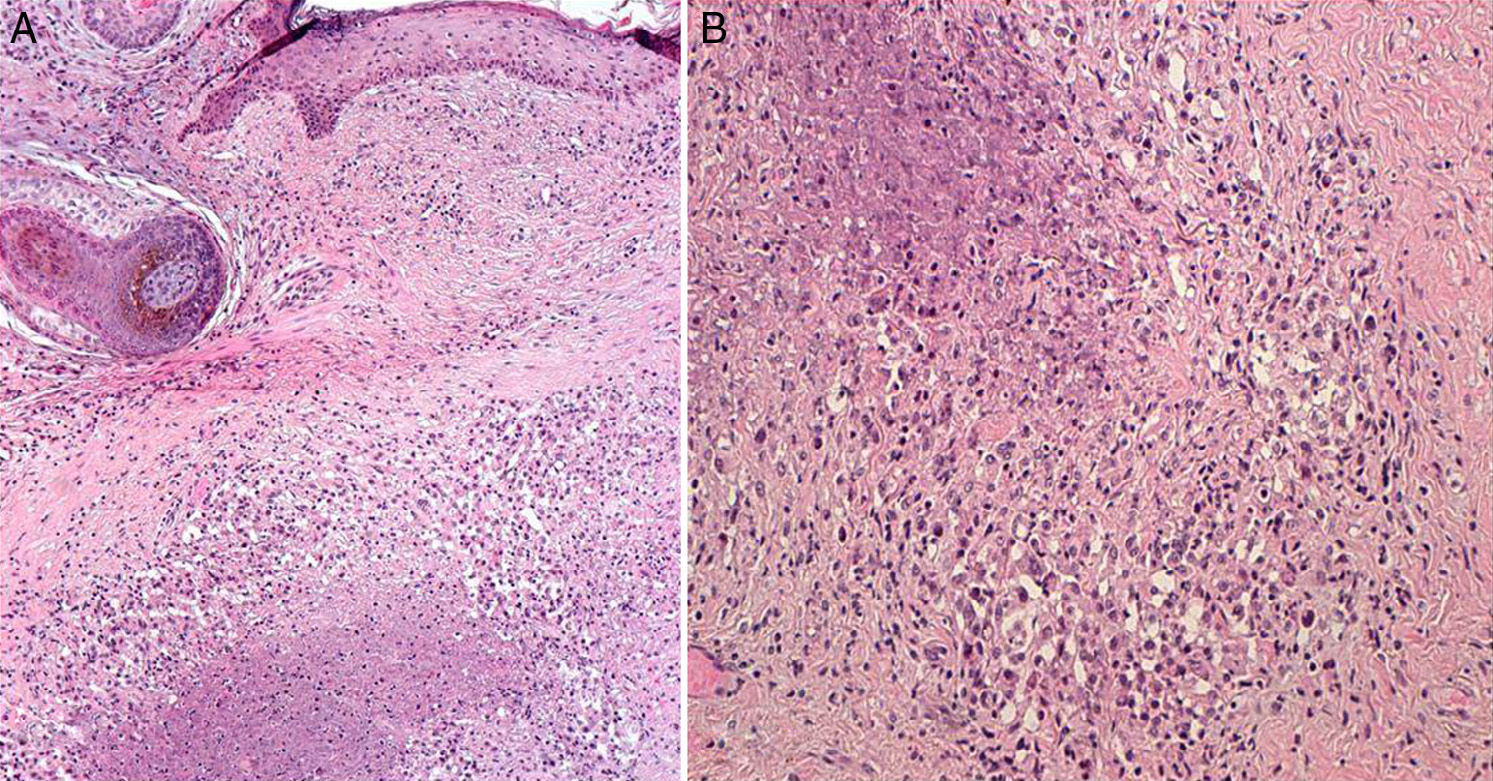
Two biopsies were performed of the lesion in the zygomatic area. Pathology did not detect any images suggestive of lymphoma, but it did reveal necrotizing granulomatous dermatitis of the tuberculosis type (Figure 2). Further histochemical studies were performed, with Periodic acid–Schiff and methenamine staining; these were negative for fungi. The Zhiel-Neelsen technique did not detect acid-alcohol resistant bacilli. In view of these clinical and histologic findings, complementary tests including culture and PCR were undertaken for Mycobacterium tuberculosis in the tissue, but these were negative. The Mantoux test was positive with a reading of 15mm after 72hours. The QuantIFERON TB gold in-tube test was negative. With these results, a clinical-histological diagnosis of lupus vulgaris was made, with the QuantIFERON result considered a false negative. We were unable to examine the samples from biopsies conducted in the other center that, years earlier, had formed the basis for diagnosis of T-cell lymphoma. Treatment with methotrexate was suspended and tuberculosis treatment was initiated with isoniazid, pyrazinamide, and rifampicin at the same doses as indicated for pulmonary tuberculosis.
Two weeks after starting tuberculosis treatment, the patient presented a sudden worsening of his lesions. An intense inflammatory reaction occurred, with scab formation and supuration in the main lesion on the zygomatic arch and in other apparently residual lesions on the central frontal region and right temple (Figure 3). His general state of health was good, with no fever or other symptoms, apart from worsening of the skin lesions.
The medication was maintained at the same dose, without adding any new drugs, but 1 month after starting tuberculosis treatment, liver toxicity was detected in a follow-up laboratory test with transaminase elevation of more than 5 times the upper limit of normal. Treatment was suspended to allow resolution of the abnormal laboratory values. Once the transaminase levels had returned to normal 1 month after suspending the treatment, tuberculosis treatment was reintroduced slowly, with a regimen consisting of isoniazid, ethambutol, and rifampicin for 2 months, and isoniazid and rifampicin for 7 months. Once again, the lesions worsened after reintroduction of the tuberculosis treatment, with more inflammation and scab formation. In the follow-up laboratory tests, the patient¿s transaminase levels remained normal and no further liver toxicity was detected. Tuberculosis treatment continued at the same dose. The dressing on the scabby inflammatory lesions was replaced and progressive improvement was observed. Finally, a good outcome with respect to the initial lesions was obtained, without having to resort to treatments such as corticosteroids or other treatments to manage the clinical worsening (Figure 4).
DiscussionPR is an adverse clinical consequence of restoring the specific antigen immune response induced by the treatment. A range of terms have been coined for PR, such as paradoxical reaction or worsening, immune reconstitution inflammatory syndrome (IRIS), and immune reconstitution syndrome (IRS), although they all refer to the same phenomenon. Within PR/IRIS, we can distinguish 2 forms, paradoxical IRIS, which refers to a worsening or relapse of disease already treated or under treatment, and unmasking IRIS, in which there is an accelerated presentation of a disease that was latent or subclinical.9–11 PR/IRIS is well known in patients with HIV infection when they begin antiretroviral therapy; however, this phenomenon is not specific to these patients and can occur in other situations, for example, in immunocompromised non–HIV-infected patients who undergo solid organ transplantation, bone marrow transplantation, or anticancer chemotherapy, and it has even been reported in immunocompetent patients.10 We should also highlight that PR/IRIS occurs both in infectious and noninfectious processes.10 Among the infectious processes, in addition to M tuberculosis, PR/IRIS has been associated with other atypical mycobacteria as well as with other microorganisms, whether bacteria, virus, fungi, parasites, or protozoa.10 Cases of PR/IRIS associated with Cryptococcus neoformans, with a clinical presentation in the form of meningitis or disseminated disease, and those associated with JC virus, leading to progressive multifocal leukoencephalopathy, are particularly serious.10,11
Of note is PR/IRIS in cases of type I leprosy reversal reactions after initiating antiretroviral treatment in patients with HIV-Mycobacterium leprae coinfection.10,12 This type of reaction is thought to correspond to cases of IRIS unmasking of infection with M leprae that was present as latent infection in patients with HIV infection.10
In the case of noninfectious processes, PR/IRIS can be associated with autoimmune, endocrine, and neoplastic diseases.10,11 In particular, PR/IRIS can be associated with Kaposi sarcoma, where infrequent and fatal forms associated with antiretroviral treatment have been reported9,10; cases of sarcoid PR/IRIS, which have been described with a later onset, usually several months after initiating antiretroviral treatment unlike other granulomatous diseases, such as mycobacteria, with an earlier onset9–11; and cases of PR/IRIS associated with Graves Basedow disease.9–11
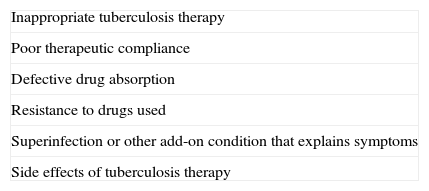
The development of PR/IRIS in non–HIV-infected patients with tuberculosis who receive appropriate tuberculosis treatment is not uncommon; indeed several studies report a frequency between 6% and 30% of patients who receive tuberculosis therapy.6,8,13 PR/IRIS affects both sexes equally, and has been described both in children and elderly patients.14 Diagnosis can only be made after ruling out other potential causes of the symptoms, such as superinfection, inappropriate tuberculosis therapy, poor therapeutic compliance, side effects of therapy, inappropriate absorption of the drug, and development of resistance to tuberculostatic agents (Table 1).6,8 This paradoxical worsening of tuberculosis in non–HIV-infected patients is more frequent in the central nervous system, the respiratory tract, and lymph nodes.6,8,15,16 Bones, tendons, pericardium, and the ileocecal region have also been reported to be affected by these responses, although much less frequently.6,8 In PR/IRIS with skin involvement, most cases are associated with the development of subcutaneous abscesses in miliary tuberculosis.7,8 Paradoxical clinical deterioration after the start of tuberculosis therapy is usually self-limiting and does not require changes or suspension of tuberculosis treatment.8 In some cases in which PR/IRIS presents in a severe form, particularly in intracranial tuberculomas, oral corticosteroids have been added on the grounds that these will help suppress the immune response thought to be responsible for this effect; however, it is not clear whether such an approach offers real benefit,16 as some authors have reported rapid improvement after initiating corticosteroid therapy whereas others have reported progression in clinical deterioration despite treamtent.17 In most published series, use of corticosteroids appears to be safe6 and beneficial during the course of PR, although prospective studies would be necessary to support its use.8 Some publications indicate specific situations in which it is appropriate to add prednisolone at a dose of 1 to 2mg/kg/d for no more than 6 weeks, as for example in cases of tuberculous polyserositis, sarcoid PR/IRIS, autoimmune PR/IRIS, PML due to JV virus, and more severe forms of PR/IRIS regardless of cause, among others.10
The mechanisms of PRs are not well known, but they appear to be immunomediated by abnormal immune response to proteins released by the destruction of tuberculosis bacilli,8 a decrease in immunosuppression, or a local phenomenon induced by mycobacterium-reactive lymphocytes.13,16 In our patient, we believe that these mechanisms, as well as immune reconstitution resulting from suspension of methotrexate, could explain the PR/IRIS.
In conclusion, we present a patient with lupus vulgaris who developed PR/IRIS with tuberculosis therapy, with a good final outcome. We have not found similar reports in the literature, probably because of underdiagnosis or because such cases have not been published. As in most cases of PR/IRIS, it was not necessary to discontinue or modify treatment because of worsening of the skin lesions, although liver toxicity required temporary suspension of treatment. The final outcome, after reintroduction of the drugs, was very satisfactory.
We believe that this early paradoxical immune reaction (occurring within 2 weeks) could be influenced by the suspension of methotrexate along with the initiation, almost at the same time, of tuberculosis treatment.
Given tuberculosis infection in Spain is increasing for a number of reasons such as the greater prevalence of AIDS, increased use of immunosuppressive drugs, immigration from developing countries, and the increased prevalence of strains of first-line drug-resistant M tuberculosis,1,2,8 there may also be an increase in cases of cutaneous tuberculosis. PR/IRIS after starting treatment could therefore occur more frequently in everyday clinical practice and we should be familiar with it.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Ethical ResponsibilitiesProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed their hospital's protocol on the publication of data concerning patients and that all patients included in the study have received sufficient information and have given their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare that patient data do not appear in this article. The authors declare that patient data do not appear in this article. The authors declare that patient data do not appear in this article.
Please cite this article as: Santesteban R, Bonaut B, Córdoba A, Yanguas I. Respuesta paradójica al tratamiento antituberculoso en un caso de lupus vulgar. Actas Dermosifiliogr. 2015;106:e7–e12.