The high rate of relapse of acne lesions following oral isotretinoin treatment is a common problem which remains unsolved. To avoid or minimize relapses, topical retinoids have been used for many years as maintenance treatment. However, adverse effects frequently occur.
AimsTo determine the efficacy and safety of a new retinoid combination (Retinsphere technology) in maintaining post-treatment response to oral isotretinoin.
Patients and methodsProspective, randomized, double-blind and vehicle-controlled study of 30 patients with acne previously treated with isotretinoin. Treatment with the retinoid combination was applied to one side of the face and vehicle was applied to the other, once daily, for 3 months. Standardized photographs were taken using RBX technology at baseline, 1.5 months and 3 months. The primary efficacy endpoint was the appearance of relapse on the treated side compared to the vehicle-treated side. Other endpoints included lesion count, investigator-reported improvement, patient-reported improvement, impact on quality-of-life, and side effects.
ResultsAlthough the majority of patients did not reach the total target dose of oral isotretinoin, the relapse rate was significantly lower on the retinoid-treated side compared to the vehicle-treated side. Likewise, improved lesion count and excellent tolerance were observed.
ConclusionsThis new retinoid combination (Retinsphere technology) were effective and safe as maintenance therapy after post-treatment response to oral isotretinoin in patients with acne.
Existe un alto porcentaje de pacientes que presentan reidivas de acné tras el uso de isotretinoína oral. Para evitar o minimizar dichas recidivas el uso de retinoides tópicos se ha utilizado en ocasiones, aunque con mala tolerancia dada la sensibilidad de la piel tras los tratamientos con isotretinoína oral.
ObjetivosDeterminar la eficacia y seguridad de una nueva combinación de retinoides (tecnología Retinsphere®) en el mantenimiento de la respuesta postratamiento con isotretinoína oral.
Pacientes y MétodosEstudio prospectivo, aleatorizado, doble ciego controlado con vehículo en 30 pacientes con acné tratado previamente con isotretinoína oral. El tratamiento con la combinación de retinoides se aplicó en una hemicara, mientras que en la otra hemicara se aplicó vehículo, durante 3 meses. Se tomaron fotografías estandarizadas con tecnología RBX en el momento basal, al mes y medio y a los 3 meses. La variable principal para determinar la eficacia fue la aparición de recidivas en el área tratada con retinoides vs lado tratado con vehículo. Otras variables estudiadas fueron recuento de lesiones, mejoría percibida por el investigador y el paciente, impacto en la calidad de vida y efectos adversos.
ResultadosLa mayoría de los pacientes no habían alcanzado la dosis diana de isotretinoína oral, y sin embargo el porcentaje de recidivas fue significativamente menor en el lado tratado con retinoides frente al lado tratado con vehículo. Además se objetivó una disminución en el recuento de lesiones y una excelente tolerancia.
ConclusionesEsta nueva combinación de retinoides (tecnología Retinsphere®) demostró eficacia y seguridad en el mantenimiento de respuesta postratamiento con isotreinoína oral en pacientes con acné.
Acne is a common complaint among adolescents, although onset can occur at other stages of life. In fact, acne affects to a greater or lesser extent between 80 and 85% of individuals aged between 12 and 25 years1 and in addition to the potential physical discomfort (for example, pain, itching, superinfection, and scarring), serious psychological repercussions may occur as the face is often targeted by this disease.
We can classify acne into different types according to the predominant lesion, with classic forms including papulopustular, comedonal, and nodulocystic acne.1 There are several classes of therapeutic drugs used to tackle different types of acne. One of the most widely used medications is oral isotretinoin as it targets all levels of acne pathogenesis. According to expert consensus, the recommended dose is 0.3–0.5mg/kg/d for moderate papulopustular or nodular acne and more than 0.5mg/kg/d for at least 6 months (with a mean total cumulative dose of 120–150mg/kg) for acne conglobata. Other authors, however, recommend lower or pulsed doses for longer periods in cases of moderate acne.2–4
Regardless of the dosage regimen used, at the end of treatment most patients show substantial improvement in acne lesions, although this is coupled with erythema and deterioration in the quality of skin due to the extreme cutaneous dryness induced by the treatment. Moreover, recurrence of acne lesions following isotretinoin treatment remains an unsolved problem. According to recent studies, the percentage of patients with relapses is very variable and ranges between 10 and 61% depending on the cumulative dose,5 population characteristics, and duration of follow-up.6 There is some debate as to whether failure to reach the target dose leads to the early onset of acne relapse.7,8 To establish a basis for comparison of the mean relapse rate, the study with the greatest number of patients (17351), which described a mean relapse rate of 41%, can be taken as a reference.8 However, there are no specific data on relapse percentages over short periods of time after discontinuing isotretinoin administered at the standard dose of 120–150mg/kg.
To avoid relapses after isotretinoin administration, topical retinoids have been used for many years in patients with acne due to their capacity to reduce hyperseborrhea (by inhibiting the proliferation and differentiation of sebocytes) and normalize keratinization.3 Some authors have suggested that their use at the end of treatment with oral isotretinoin may help prevent future relapses.3,9–12 Consequently, the main objective of the present study is to demonstrate that a new product, whose main component is Retinsphere technology, is effective for reducing acne relapses or maintaining the results obtained by acne patients after treatment with oral isotretinoin. Furthermore, we will determine tolerance to the new product in these patients, without the usual adverse events seen with other retinoids.
Materials and methodsA prospective, randomized, double-blind, placebo-controlled (vehicle) study was carried out on both sides of the face. Thirty-two patients were recruited. Treatment with the retinoid combination was applied on a split-face model, applying the active product to one side of the face and the vehicle to the other, once daily for 3 months.
Inclusion criteriaPatients greater than 14 years of age who had finished treatment with oral isotretinoin (including patients who had or had not reached the conventional target dose of 120–150mg/kg) in the previous 6 months were included. Family and individual medical histories, previous treatments, weight, ingestion time of oral isotretinoin, time since discontinuation of oral isotretinoin, daily dose, total cumulative dose, and informed consent were recorded. The protocol was approved by the ethics committee of our hospital.
Exclusion criteriaPatients less than 14 years of age and those with other concomitant dermatoses or sensitization to any of the components of the product were excluded from this study. Women not using a contraceptive method were also excluded from the study.
TreatmentThe test product was a combination of 2 retinoids, retinol encapsulated in glycospheres and hydroxypinacolone retinoate, marketed under the name Retinsphere Technology, in a base enriched with natural humectant factors. The treatment protocol included the application of a fingertip of this retinoid combination (Biretix gel [Industrial Farmacéutica Cantabria SA, Madrid, Spain]) to one side of the face and vehicle alone to the other side of the face at night, for 3 months. Thus, each patient acted as his or her own control. All patients and, if required, their legal guardian, signed the informed consent.
Randomization was performed by an independent statistician using the Random Function of standard computer software. The code, which established which side of the face to apply product or vehicle, was kept in a sealed envelope until the end of the study. Neither the patient nor the investigator was informed about the composition of the 2 creams, which had the same texture and odor and were only distinguishable by the color of the tube.
Clinical assessmentThe assessments were carried out at baseline (T0) then after 1.5 months (T1) and 3 months (T2) by the same, blinded investigator. A physical examination was carried out together with a standard photographic record with RBX technology (Reveal, Canfield Inc., Fairfield, NJ, USA) on each visit.
Primary endpointThe primary endpoint was relapse incidence after 3 months from treatment with oral isotretinoin, compared to the standard relapse incidence without post-isotretinoin treatment (vehicle). Given the lack of consensus on the definition of relapse and that hardly any patients had acne lesions at the start of the study (as they had recently finished treatment with isotretinoin), we defined relapse as an increase in the number of lesions (comedones, papules or pustules), that is, when one or more new lesions compared to T0 appeared on either side of the face (T2>T0=relapse).
Secondary endpointsThe following were secondary endpoints
- •
Lesion count
- •
Investigator's Global Assessment (IGA): Validated scale.13 Scores ranged from 0 to 5, where 0 indicated absence of inflammatory and non-inflammatory lesions; 1, almost clear; 2, mild severity; 3, moderate severity; 4, severe; and 5, very severe.
- •
Quality-of-life: Improved quality-of-life of the patient measured by the Social Quality-of-Life (SOQOL) scale14 (0, no involvement to 27, intense involvement). There are 9 items (body perception, social aspects, emotional aspects, and symptoms of acne). Each item is graded from 0 to 3 where 0 indicates no involvement; 1, mild involvement, 2, moderate involvement; and 3, intense involvement.
- •
Improvement perceived by the patient with the Patient Global Assessment scale, (PGA)15: scores ranged from 0 to 4 where 0 indicated deterioration or no change; 1, mild improvement; 2, moderate improvement; 3, great improvement; and 4, excellent improvement.
- •
Patient satisfaction with previous treatments and after the retinoid combination (0–10, where 0 indicated no satisfaction and 10, maximum satisfaction).
- •
Shine subjectively perceived by the investigator (0, nonexistent when no shine at all was perceived; 1, mild when slight degree of shine in some areas of the face was perceived but it was not intense; and 2, intense when a high degree of shine all over the face was perceived).
- •
Erythema subjectively perceived by the investigator (0, nonexistent when no erythema at all was perceived; 1, mild when some areas of the face showed redness; 2, intense when almost all the face was red).
- •
Scaling subjectively perceived by the investigator (0, nonexistent when no desquamation was perceived; 1, mild when some grade of desquamation was perceived in some areas of the face; or 2, intense when rough desquamation was perceived in all the face).
- •
Hydration subjectively perceived by the investigator (0, nonexistent when all the face was dry; 1, mild when hydrated areas are mixed with dry ones; or 2, intense when no dry areas were perceived).
- •
Degree of improvement in scars (SCAR-S), according to the Goodman scale13 based on the morphology graded from 0 to 4, where 0 indicates absence of scars; 1, macular scars; 2, mild scars (depressions or millimetric papules); 3, moderate (boxcar, deeper depressions or papular or hypertrophic scars); and 4, severe (ice pick, deep, dystrophic scars).
- •
Subjective adverse effects reported by the patient: scaling, itching, burning, erythema or dryness (0, non-existent; 1, mild; or 2, intense).
Statistical analysis was performed with SPSS v18.0 software (Chicago, IL, USA). Results are presented as mean (SD) values. The Wilcoxon nonparametric test for paired data, as the comparisons were paired both in time and between treatments. In the subsection where the isotretinoin dose was analyzed for influence on the response to the product compared to vehicle, the Mann–Whitney non-parametric test was used, as they are two independent groups. The percentages of patients with deterioration and improvement were calculated for each group, and the McNemar test was used to determine the statistical significance of the difference between 2 percentages.
Before initiating the study and based on previous studies,16 in which the number of lesions decreased 90% after 3 months, assuming 10% rate of recurrent or persistent lesions, the statistical software estimated a sample size of 30 patients, assuming an SD of 3. Statistical significance was set to P≤0.05.
ResultsThirty-two patients who completed treatment with isotretinoin in the last year were included. Of these, 40.6% were male (mean age, 18.4±5.2 years) and 59.4% female (mean age, 23.5±5.6 years). Two patients did not complete the study due to work commitments.
The mean period from discontinuation of treatment with isotretinoin until initiation of the study was 2 months (range, 2 weeks to 6 months). Of the 30 patients who completed the study, 7 (23%) had reached the standard cumulative target dose of isotretinoin (mean dose for these patients, 147.71mg/kg). Twenty-three of the 30 patients (77%) had not reached the target dose but had reached a mean of 68.34mg/kg by the time they suspended oral isotretinoin due to the arrival of summer, intolerance or clearance of lesions. Thus, the majority of our patients had not reached the total cumulative target dose of 120–150mg/kg.
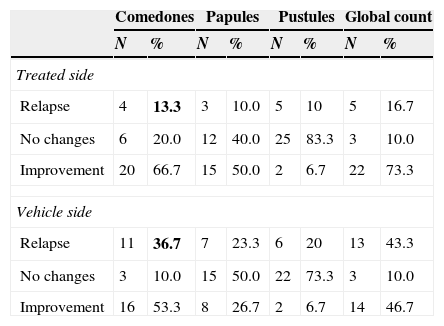
RelapsesThe percentage of relapses on the side treated with the retinoid combination was almost 17% compared to 43% on the vehicle side; this difference was statistically significant (P=0.021) (Table 1).
Evolution of lesions after 3 months of maintenance treatment with the retinoid combination. The percentage of relapses on the treated and vehicle side are shaded in a darker color and are significantly greater on the vehicle side.
| Comedones | Papules | Pustules | Global count | |||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| Treated side | ||||||||
| Relapse | 4 | 13.3 | 3 | 10.0 | 5 | 10 | 5 | 16.7 |
| No changes | 6 | 20.0 | 12 | 40.0 | 25 | 83.3 | 3 | 10.0 |
| Improvement | 20 | 66.7 | 15 | 50.0 | 2 | 6.7 | 22 | 73.3 |
| Vehicle side | ||||||||
| Relapse | 11 | 36.7 | 7 | 23.3 | 6 | 20 | 13 | 43.3 |
| No changes | 3 | 10.0 | 15 | 50.0 | 22 | 73.3 | 3 | 10.0 |
| Improvement | 16 | 53.3 | 8 | 26.7 | 2 | 6.7 | 14 | 46.7 |
There were no statistically significant differences in the number of relapses (regardless of whether they were inflammatory or non-inflammatory lesions) between those who stopped treatment with isotretinoin after reaching the target dose and those who stopped due to the arrival of summer, and therefore did not reach the total cumulative dose (data not shown).
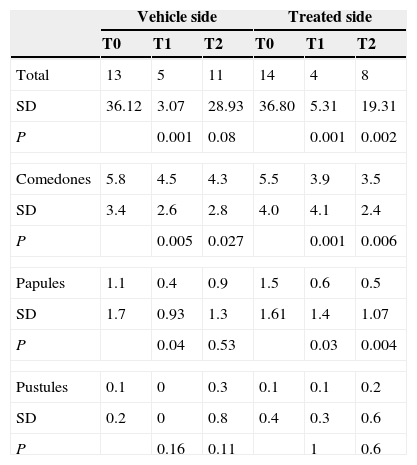
Lesion countThe reduction in the overall number of lesions at visits T1 and T2 on the treated side was statistically significant compared to the baseline count (P=0.001 and P=0.002, respectively), whilst on the vehicle side it was only significant at T1 (P=0.001) but not at T2 (P=0.08). In the case of comedones, the final reduction (T2) in the mean number of comedones on the treated side was statistically significant when compared to baseline (P=0.006) and so was the final reduction (T2) in the mean number of papules (P=0.004). An increase (not significant) in the final number of pustules was observed on the treated side compared to the baseline count, whilst on the vehicle side a 5-fold increase at visit T2 compared to the number of baseline pustules was observed (Table 2).
Mean number of global lesions and individual lesions (comedones, papules and pustules) in each visit (T0, T1 and T2) on treated side and vehicle side. SD (standard deviation). Statistical significance (P) refers to the mean number of lesions during visits T1 and T2 compared to the basal visit (T0), showing the vehicle side and the treated side.
| Vehicle side | Treated side | |||||
|---|---|---|---|---|---|---|
| T0 | T1 | T2 | T0 | T1 | T2 | |
| Total | 13 | 5 | 11 | 14 | 4 | 8 |
| SD | 36.12 | 3.07 | 28.93 | 36.80 | 5.31 | 19.31 |
| P | 0.001 | 0.08 | 0.001 | 0.002 | ||
| Comedones | 5.8 | 4.5 | 4.3 | 5.5 | 3.9 | 3.5 |
| SD | 3.4 | 2.6 | 2.8 | 4.0 | 4.1 | 2.4 |
| P | 0.005 | 0.027 | 0.001 | 0.006 | ||
| Papules | 1.1 | 0.4 | 0.9 | 1.5 | 0.6 | 0.5 |
| SD | 1.7 | 0.93 | 1.3 | 1.61 | 1.4 | 1.07 |
| P | 0.04 | 0.53 | 0.03 | 0.004 | ||
| Pustules | 0.1 | 0 | 0.3 | 0.1 | 0.1 | 0.2 |
| SD | 0.2 | 0 | 0.8 | 0.4 | 0.3 | 0.6 |
| P | 0.16 | 0.11 | 1 | 0.6 | ||
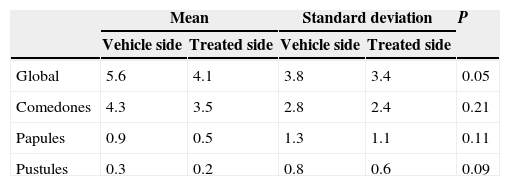
When comparing the results of both sides, the average number of comedones on the treated side showed an almost 20% larger reduction at visit T2 compared with the vehicle side, although the difference was not statistically significant (P=0.21). For papules on the treated compared to vehicle side, although the mean reduction on the treated side on visit T2 was almost 50% higher than that obtained with vehicle, the difference as not statistically significant (Table 3). The average total number of lesions was significantly lower on the side treated with the active product (P=0.05) compared to vehicle-treated side (Table 3).
Comparison at the end of the study (T2) between the vehicle side and the side treated with product, showing significant differences in the mean number of global lesions.
| Mean | Standard deviation | P | |||
|---|---|---|---|---|---|
| Vehicle side | Treated side | Vehicle side | Treated side | ||
| Global | 5.6 | 4.1 | 3.8 | 3.4 | 0.05 |
| Comedones | 4.3 | 3.5 | 2.8 | 2.4 | 0.21 |
| Papules | 0.9 | 0.5 | 1.3 | 1.1 | 0.11 |
| Pustules | 0.3 | 0.2 | 0.8 | 0.6 | 0.09 |
The mean IGA obtained at baseline was 2.2 (mild severity) on both sides of the face with no significant differences between them, while the IGA on finishing treatment at T2 on the side treated with retinoids was on average 1.4 (almost clear), significantly better than baseline (P<0.01), unlike the vehicle side where significant post-baseline changes were not observed (the mean severity at T2 was 2 [mild]; P=0.106).
The IGA improvement perceived by the investigator was demonstrated in 60% of the sides of the face treated with the product versus 30% of the sides of the face treated with vehicle.
Patient-reported improvementThe mean quality-of-life score, as measured by the SOQOL scale at baseline (T0) after discontinuation of isotretinoin treatment, was 3.8 (n=27) while the impact after topical treatment with the study product further improved this quality-of-life data by reducing the SOQOL score to 1.8 (n=27) at T2, after 3 months. The increase in overall satisfaction indicated an improvement in the perception of skin appearance described by the patient.
Overall, 90% of patients who received treatment experienced some degree of improvement during the treatment and almost 50% showed good or excellent improvement.
Investigator-reported skin quality and cutaneous toleranceThere were no differences between either side of the face in the scoring of shineness or scaling, either at the beginning or the end of the treatment. The mean baseline hydration was 0.53 (between non-existent and mild) with no differences between treated and untreated sides of the face. At T2, significant differences were observed (P=0.02) with a score of 1.3 (mild) on the side treated with the combination of retinoids versus 0.2 (non-existent) on the side treated with vehicle. In the case of erythema, on T2 the mean erythema showed no significant differences between either treatments indicating an excellent tolerance to retinoids.
Patient perceptionNo significant differences were registered at any time regarding subjective discomfort perceived by the patient (scaling, dryness, itching, burning and erythema). Only one case of pruritus was described on visit T1, which disappeared by visit T2.
Other variablesAt the end of the study (T2), a significant improvement in extent of scarring was observed on the treated side compared with the vehicle side (P=0.002).
No statistical differences in the PGA were found after the treatment compared with baseline.
DiscussionIn this study we have demonstrated the efficacy of a new product in decreasing the number of relapses following isotretinoin treatment compared to vehicle, while showing excellent tolerance and no adverse events. Although a significant reduction in the total number of lesions was found on the treated side compared to the vehicle side, when individual lesions were studied this difference was not statistically significant. This effect may be due to the small sample size and low number of total lesions at the beginning of the study (T0).
At the end of the treatment, the vehicle side showed a trend toward relapse of 43%, similar to that observed in literature in the follow-up of groups without post-isotretinoin treatment.8 Interestingly, the side treated with Retinsphere technology showed a significantly lower relapse rate (17%), demonstrating the efficacy of maintenance treatment with these topical retinoids. Although we did not find any significant differences between the target dose and onset of relapse, among patients with relapse (16 subjects), just 25% (4/16) had reached the target dose of 120mg/kg.
These results are consistent with those reported in some other published studies 5,6 but could also be due to the small sample size.
The mean follow-up time from suspension of oral isotretinoin to the end of the study was 6 months, which may appear short but given that the majority of patients (77%) in our study had not reached the target dose at the time of discontinuation (due to the arrival of summer, intolerance or clearance of lesions), in theory we expected an early relapse, although this latter point is controversial.7
Quereux et al.17 defined a maintenance treatment with topical retinoids as the most important protective factor for the prevention of relapse. Borghi et al.3 described the use of maintenance therapy with topical retinoids for 1 year after discontinuation of oral isotretinoin, with a very low relapse rate (9%) in spite of having used low doses of oral isotretinoin.
In our study, investigator-reported improvement was observed in 60% of patients treated with topical retinoids compared with an improvement of 30% on the vehicle side, demonstrating that Retinsphere technology is effective in improving acne lesions that persist after treatment with isotretinoin. Improvement on the vehicle side in our study can be attributed to long-term improvements induced by cumulative isotretinoin dose and the effect of the vehicle in improving skin quality after treatment with oral isotretinoin. According to our results, topical retinoids are useful in improving persistent non-inflammatory and inflammatory lesions.
The excellent tolerance and cutaneous compatibility of the product is supported by the immunomodulatory role of retinoids,1 their theoretical capacity for accelerated cutaneous regeneration18 attributed to the stimulation of neocollagenesis,19 as well as to the possible role, yet to be confirmed, of transforming growth factor β.20 Topical retinoids can be associated with skin irritation but this innovative retinoid combination maintained the efficacy of topical retinoids without observing associated dermatitis.
The new product is based on Retinsphere technology, which combines 2 topical retinoids, retinol encapsulated in glycospheres and hydroxypinacolone retinoate. This combination has been used previously in patients with active acne, with an improvement in the lesion count (macrocomedones and microcomedones), follicular keratinization, and measures of seborrhoea and acne severity according to the Global Acne Grading System with few side effects, all mild.21 The ester of retinoic acid, hydroxypinacolone retinoate, acts in a similar way to tretinoin but does not cause the irritation observed with this retinoid. Recently, Veraldi22 showed that the use of this new combination for 2 weeks in patients improved skin roughness by 50% and scaling by 40%. Unlike retinol and other derivatives that need to be converted to the biologically active form of retinoic acid, hydroxypinacolone retinoate binds directly to retinoic acid receptors.20,23
Some limitations of the study were that the time lapse between finishing oral isotretinoin and starting with topical treatment was very variable, ranging from 2 weeks to 6 months, possibly leading to increased variability of the results. In addition, the patients had received different total doses of oral isotretinoin. These limitations hinder assessment of whether the emergence of relapses is related to the total cumulative dose and/or to the small sample size.
The importance of maintenance treatment with retinoids is noteworthy from a psychological standpoint, as it helps to sustain an improved quality-of-life after use of oral isotretinoin, as well as the perception of improvement and satisfaction described by the patient.
ConclusionsAvoidance of a relapse after treatment with isotretinoin, especially if the target dose is not reached, has not been studied in depth. To prevent such relapses, this new retinoid combination has proven effective and is able to significantly improve acne lesions compared with baseline and with treatment with vehicle. In conclusion, the use of topical retinoids, after suspending isotretinoin either in the initial months or during the post-treatment year, when relapse rates are higher, could be a protective factor to prevent relapse, with efficacy and tolerance statistically demonstrated in this and previous studies.3,11,12 Likewise, this study confirms that maintenance therapy with retinoids after discontinuation of oral isotretinoin with residual acne lesions can reduce both non-inflammatory and inflammatory lesions.
Retinsphere technology has proven effective and safe in the maintenance treatment after oral isotretinoin in patients with acne, although future studies with a longer follow-up period may confirm the results observed.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe conduct of the present study was funded by Industrial Farmaceutica Cantabria S.A. (IFC S.A., Madrid, Spain).
Conflicts of interestM.T. Truchuelo receive economic compensation of IFC laboratories for external advice. The remaining authors declare that they have no conflict of interest.
The authors thank María Vitale, M.D., Medical Manager working at IFC laboratories for her contribution to this study and support while preparing the present manuscript.