A 52-year-old woman presented with pruritic dermatitis that had been treated in different hospitals for more than 40 years. Atopic dermatitis was suspected during childhood and the patient was treated with cyclosporin A with some improvement. In 2002, she presented with facial nodules that were histologically compatible with B-cell lymphoma (CD20+, BCL2+, IgH rearrangement) and treatment with cyclosporin was suspended. After ruling out extracutaneous involvement, she was given intravenous rituximab at a dosage of 375mg/m2 in 4 weekly cycles. Symptoms improved but reappeared when treatment was suspended. In 2013, the patient presented again with facial nodules that were histologically compatible with B-cell lymphoid hyperplasia. the patient was treated with rituximab and showed an identical response.
Due to a change of address, she was sent to our department in 2016 with no definitive diagnosis. On questioning, she confirmed the recurrence of the lesions after long periods of exposure to sunlight.
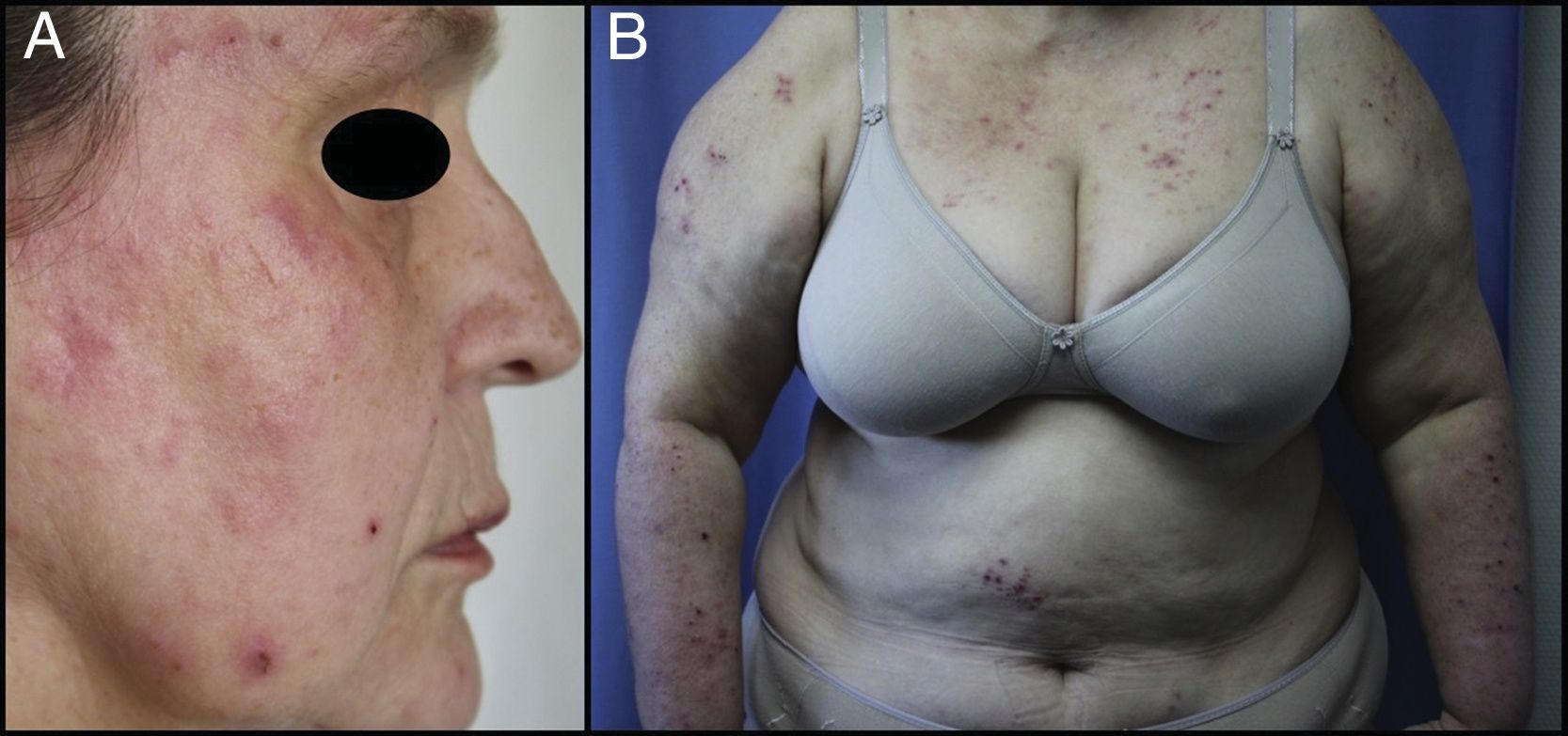
Physical ExaminationThe patient presented erythematous papules, many of which showed central excoriation, that were confluent in some locations (Fig. 1A), predominantly in the areas exposed to sunlight (Fig. 1B). Some residual hyperpigmented macules were visible in these areas.
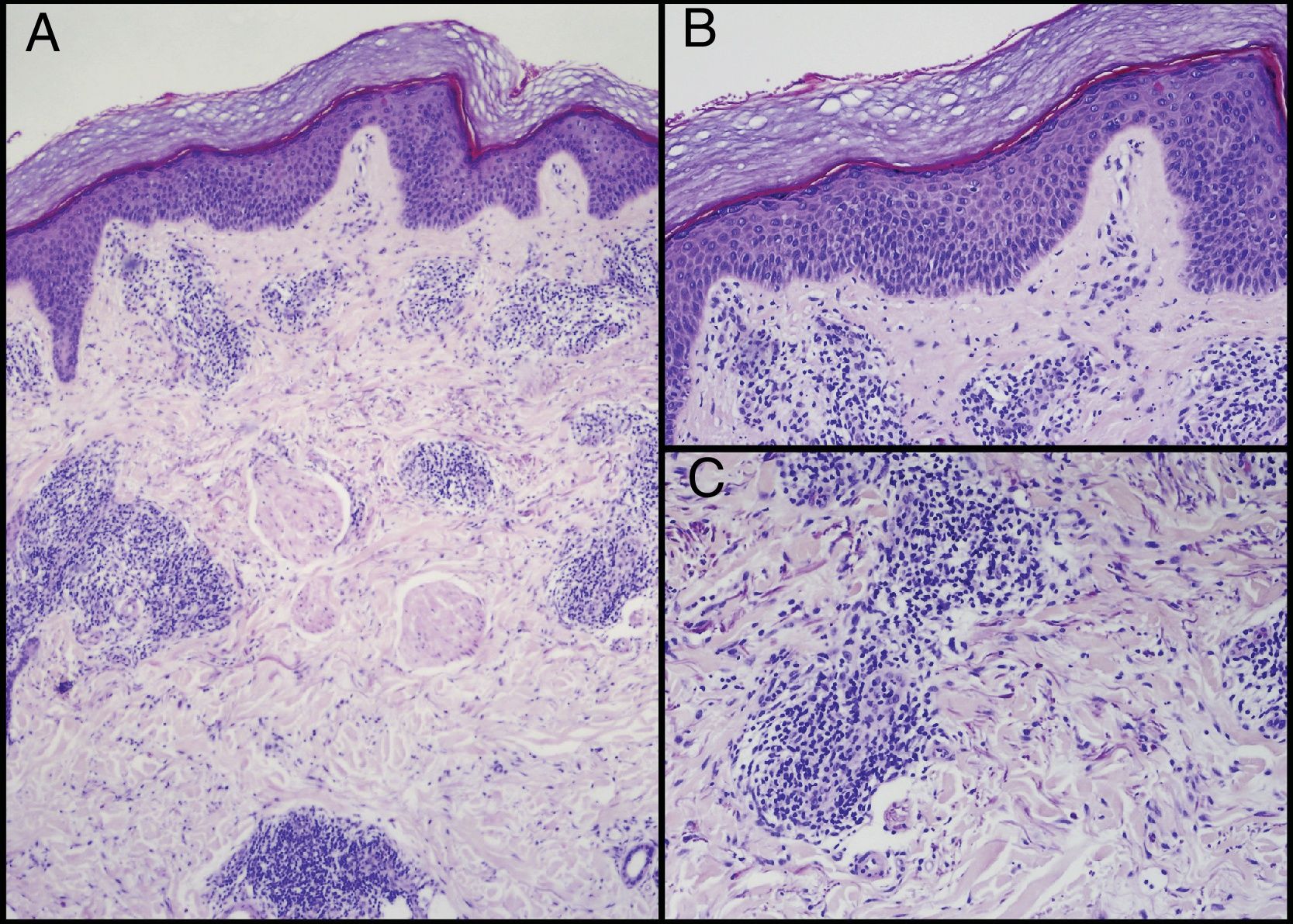
HistopathologyBiopsies were taken of a crusted papular lesion and an erythematous plaque on the temple, which the patient had stated were similar to those diagnosed as cutaneous lymphoma/lymphoid hyperplasia; both lesions were histologically similar (Fig. 2A): superficial perivascular dermal infiltrate (Fig. 2B) and deep T lymphocyte infiltrate with abundant eosinophils (Fig. 2C).
Other TestsHLA determination revealed the HLA-DR4 variant (DRB1*04:08). The autoimmune study was negative and IgE was normal.
What is your Diagnosis?
DiagnosisActinic prurigo (AP)
Treatment and CourseNarrow-band UVB phototherapy was instated to stimulate habituation, with irregular compliance by the patient, who finally abandoned this treatment despite some improvement of the condition. Thalidomide does not currently appear to be an option because the patient suffers from bilateral carpal tunnel syndrome, which makes monitoring potential neuropathy difficult. The patient is currently undergoing treatment with topical corticosteroids, oral antihistamines, and photoprotection, and maintains mild symptoms.
CommentAP is a frequent photodermatosis in Native Americans and few cases have been reported in the European population.1 The forms that present in childhood, generally before the age of 10 years, may improve during adolescence. Later onset, though less frequent, tends to be associated with persistence into adulthood.1–3 Half of patients present a family history of the disease and nearly 90% have HLA-DR4, and HLA-DRB1*04:07 is present in between 60% and 70% of patients.3,4 Our patient reported that her father had presented a similar dermatosis.
Clinical presentation consists of erythematous pruritic papulonodular lesions with excoriation due to scratching, predominantly in the areas exposed to sunlight, although they may also appear in unexposed areas. Associated clinical findings such as cheilitis (46% of cases), conjunctivitis (21% of cases), eczematous lesions, and lichenification have been reported.1
Histology may reveal nonspecific findings that are occasionally similar to the histology of polymorphic light eruptions: a superficial and deep perivascular T lymphocyte infiltrate with presence of eosinophils under a dermis with few abnormalities. Chronic lesions may reveal acanthosis and excoriation in the epidermis, fibrosis, and a larger infiltrate in the dermis. Labial lesions may present infiltrates with follicular hyperplasia as a reactive phenomenon.4 Association with B cell lymphoma occurred in only 2 patients.5 In our patient, doubt remained regarding whether the nodular lesions corresponded to lymphoma or to florid follicular lymphoid hyperplasia.
The differential diagnosis of PA includes bites and stings, scabies, porphyria, adult atopic dermatitis, and other photodermatoses, which have different courses and histology and should be ruled out to reach diagnosis of this entity.1
Different therapeutic approaches to AP have been reported, including topical treatments (photoprotection, corticosteroids, calcinuria inhibitors) and phototherapy (PUVA or narrowband UV-B). Thalidomide, cyclosporin, azathioprine and pentoxifylline have been used in severe cases, with varying results.6
In conclusion, AP is a rare entity in our setting but it cannot be ruled out. Lymphoid hyperplasia may develop during the course of the disease and this should be remembered in order to avoid an erroneous diagnosis that may condition future treatment. Diagnosis of this entity is based on clinical presentation and patient history, and the presence of HLA-DR4 is a finding that supports the suspected diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Schneller-Pavelescu L, Caso EV-d, Blanes MM. Erupción papulosa fotodistribuida. Actas Dermosifiliogr. 2019;110:309–310.